Translate this page into:
Determination of human cytomegalovirus pp65 antigenemia among renal transplant patients
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Human cytomegalovirus (HCMV) is an important cause of morbidity and mortality in immunosuppressed transplant recipients. Isolation of HCMV from peripheral blood leukocytes (PBLs) is considered a reliable marker of disseminated HCMV infection. HCMV pp65 antigenemia is widely used for monitoring CMV infection and guiding preemptive therapy. The aim of this study was to compare pp65 antigenemia with culture technique for detection of HCMV in PBLs among kidney transplant patients and also to determine the threshold value of significant pp65 antigenemiat. Fifty-one peripheral blood samples from post-renal transplant patients collected during August 2009 to March 2011 were processed for pp65 antigenemia assay. These were also tested for isolation of the virus by inoculation into human corneal fibroblast cells. The results of pp65 antigenemia and culture were compared to determine the clinical significance of pp65 antigenemia. HCMV was isolated in 21 cases. On comparing the pp65 antigenemia results with that of the viral isolation, a mean of 23 cells was determined to yield a positive isolation of HCMV. The values of pp65 antigenemia and isolation results were correlated (paired t-test, P = 0.0029). A pp65 count of 23 and above was considered significant in our clinical settings since we found that these clinical specimens yield positive culture result.
Keywords
Corneal fibroblast culture
human cytomegalovirus
threshold pp65 antigenemia count
Introduction
More than 80% of the adult population worldwide is infected with human cytomegalovirus (HCMV). Primary infections occur early in the childhood and may cause exanthema subitum. HCMV infection is an important cause of morbidity and mortality in immunosuppressed organ transplant recipients.[1–3]
As the diagnosis of HCMV infections cannot be made reliably on clinical grounds alone, laboratory confirmation is required. The most specific laboratory method for diagnosis of HCMV infection is isolation of the virus in culture. Isolation of HCMV from blood leukocytes (CMV viremia) is considered the most reliable marker of disseminated CMV infection, and predicts invasive CMV disease.[4–8] HCMV can infect a number of cell types, namely, fibroblasts, epithelial and endothelial cells, and smooth muscle cells.[9] In particular, HCMV has been shown to infect and replicate in endothelial cells of the vascular tree. HCMV is also present in peripheral myeloid cells of 50-90% of normal individuals. In disseminated infection, cytomegalic endothelial cells may circulate in the peripheral blood, and virus dissemination is mediated by peripheral blood leukocytes (PBLs) carrying infectious virus acquired from infected endothelium and transmitting the infection to uninfected endothelial cells.[10–12] Isolation of HCMV from human PBLs has been documented. Successful isolation was reported for various leukocyte subpopulations such as granulocytes, T lymphocytes, or monocytes.[1314] pp65 antigen of HCMV is recognized by more than 70% of HCMV-specific circulating T lymphocytes (CTLs). As pp65 is processed and presented before endogenous viral replication, pp65-specific CTLs may initiate the HCMV spread.[15–20]
The detection of HCMV pp65 antigenemia is widely used for monitoring CMV infection and guiding preemptive therapy in patients at risk of developing HCMV disease, as a semiquantitative analysis of HCMV viral replication.[2122] The CMV pp65 antigenemia assay, which quantitates the number of HCMV-infected leukocytes in peripheral blood, has proven efficacy in the detection and monitoring of this virus infection in immunocompromised patients.[23–26] This study was undertaken to determine the significant pp65 antigenemia count among renal transplant patients, by evaluating the test against viral isolation.
Materials and Methods
Samples
Peripheral blood samples from renal transplant recipients were collected in 2 ml EDTA vacutainer tubes and were transported immediately to the laboratory. All the patients included in the study were symptomatic and referred for laboratory investigation. All specimens were transported in their native form without any transport medium. The blood specimens were processed immediately for pp65. The study was approved by the research and ethics committees of our institute.
Antigenemia assay
The pp65 antigenemia assay was carried out on smears containing 2×105 leukocytes prepared from 5 ml of EDTA anticoagulated blood within 6 hours of receipt of the specimen. Smears were fixed in methanol for 10 minutes. Immunofluorescence staining was carried out on the smears using a pp65 staining kit obtained from Argene SA, France. The smears were stained with mouse monoclonal antibody (Argene SA, France) and examined under a fluorescent microscope (Optiphot, Nikon, Japan) with a blue filter.
Establishment of corneal fibroblast cultures
The stromal layer of the donor was cut into large pieces and placed in tissue culture flasks. The tissues were nourished with Dulbecco's minimum essential medium (DMEM) and F12 medium combination (Gibco, Invitrogen, New York, USA). The medium was supplemented with 15% fetal calf serum (Hi-Media, India), and fibroblast growth factor (Sigma, USA) at 1 μg/ml concentration. At the end of 24 hours and 48 hours, the outgrowth of fibroblast from the tissue was noted. Upon confluency, the cells were trypsinized onto 12-well tissue culture plates for growth of cells for subsequent inoculation of leukocytes for isolation of HCMV.
Viral culture
The cultured human corneal fibroblast cell line established from one donor eye and not more than 3-5 passages maintained in DMEM was used for the study. The leukocytes isolated from pp65 antigenemia-positive blood samples were inoculated onto a monolayer of cells on 12-well tissue culture plates (BD Falcon, USA) for the isolation of HCMV. The plates were rocked gently on a rocking machine for 1 hour at room temperature. The cells were incubated at 37°C in a CO2 incubator. The cultures were observed for cytopathic effect (CPE). The cultures showing CPE typically of HCMV were harvested using cell scrapers and stored at -80°C. Forty-nine randomly selected pp65-positive PBLs were tested for isolation of HCMV. Uninoculated corneal fibroblast cultures were also maintained to rule out nonspecific changes.
Real-time PCR assay
Real-time PCR (RT-PCR) targeting the morphologically transforming region mtr II sequence was applied onto the DNA extracted from the culture isolates in the rotor gene RT-PCR machine (QIAGEN, 5 Plex) using primers and thermal profile described earlier.[27] The intra- and inter-assay reproducibility were evaluated using triplicates of plasmid dilutions (101, 103, and 105) corresponding to an input of 2.5 × 103, 2.5 × 105, and 2.5 × 107 copies/ml per reaction in the same and four independent runs, respectively. RT-PCR for the quantification of CMV was performed on the viral isolates that propagated on corneal fibroblast culture. Uninoculated corneal fibroblast culture DNA was used as the culture control to rule out the presence of viral markers in each lot of the cell lines. Reagent controls were also included in each run of the RT-PCR assay.
Results
pp65 antigenemia assay
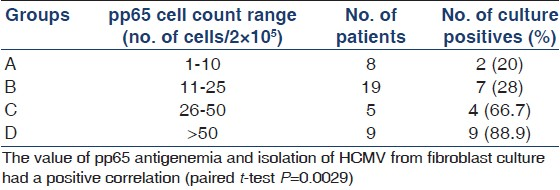
Among the 51 prepared PBLs, 49 specimens were positive for pp65 antigenemia. Based on the results, the specimens were grouped into four (groups A-D). Patients in group A had a cell count ranging from 2 to 10; group B had a count ranging from 11 to 25 cells, group C had a count ranging from 26 to 50 cells and group D had a cell count >50.
Comparison of pp65 antigenemia assay and viral isolation
Among the 49 peripheral blood specimens used for inoculation, the cultures showed megaloblastic changes in 21 (42.86%) specimens [Figure 1]. Patients under group A had a cell count ranging from 2 to 10 cells, with a mean 6.3. This group of patients had an isolation rate of 20%. Group B had a cell count ranging from 10 to 25 cells, with a mean of 15.2, and there were 7 (28%) isolates from this group of patients. Group C had a count ranging from 25 to 50 cells with a mean cell count of 39.3, and 4 (66.67%) specimens of the virus were isolated. Group D had a cell count >50 cells with a mean count of 229.11, and cultures were pisitive in 8 (88.89%) specimens [Table 1]. Isolation of the virus was further confirmed on RT-PCR assay performed on the cell culture isolates.
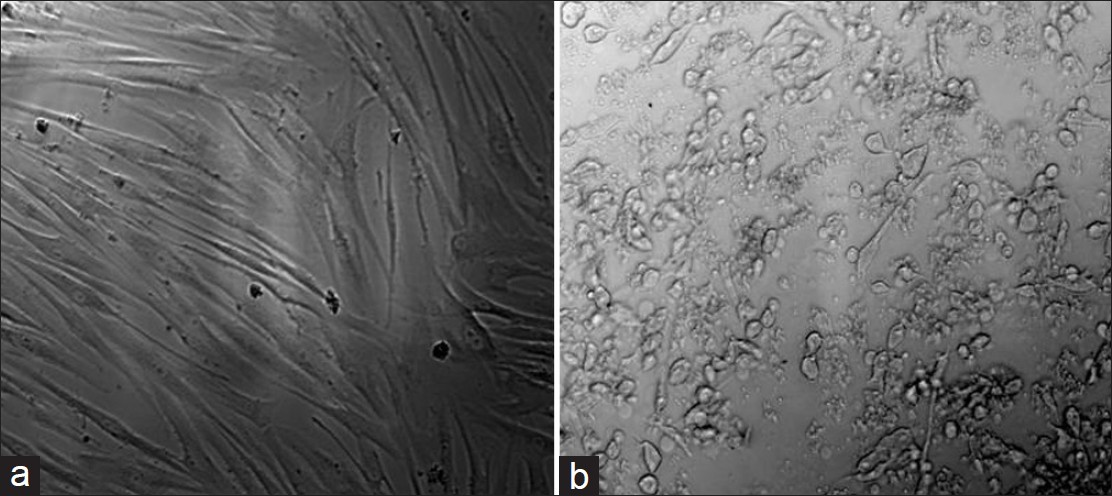
- (a) Uninfected cell control. (b) Infected fibroblast cultures
Inactivation of the virus was ruled out as all the isolates were stored at -80°C until processed. Each lot of fibroblast cell culture without exposure to leukocytes was harvested and DNA extracted from them was subjected to rule out the presence of endogenous HCMV infection.
RT-PCR assay
The RT-PCR assay performed on the DNA extracted from the culture harvests revealed copy numbers ranging from 1 to 7.4 lakh copies/ml of DNA. The range of copy numbers varied for each group (group A 10-431 copies/ ml, group B 369-7.1 lakh copies/ml, group C 328-7.04 lakh copies/ml, and group D 1734-3.2 lakh copies/ml).
The mean values of all four groups were correlated with the positivity of HCMV in culture. The results were not statistically significant (paired t-test P = 0.7). However, when the actual pp65 antigenemia value of the 49 patients was correlated with the corresponding culture results, by the paired t-test the results were statistically significant, indicating a strong correlation between the pp65 antigenemia value and the culture result (P = 0.0029).
We evaluated the most likely value of pp65 antigenemia that yields culture positive results. It was found that a count of 22.5 and above has more probability of HCMV isolation in our renal transplant patients. A count of 23 cells per 200000 leukocytes is considered as significant
Discussion
Gregory et al.,[28] compared three different assays designed for the rapid and sensitive detection of CMV in blood: quantitative shell vial culture (QSVC), PCR, and the pp65 antigenemia assay. It was found that PCR was the most sensitive of the three, allowing recognition of CMV in blood specimens from a larger number of patients and at an earlier time after transplantation than the other assays, and PCR also remained positive for the longest time after transplantation. Quantitative shell vial culture and the antigenemia assay were comparable both in the number of patients in whom CMV was detected in blood and in the time to detection. The advantage of culture was highlighted by the observation that when antiviral therapy was used, QSVC tended to become negative first, while PCR stayed positive the longest. The study finally concluded that the pp65 antigenemia assay and shell vial culture are quantifiable and comparable in sensitivity. Either is recommended for rapid detection of CMV in blood specimens from solid-organ transplant recipients.[28]
Reina et al.[29] concluded that the inoculation of all of the leukocytes extracted from blood samples in the SVC seems to produce a slight increase in the sensitivity of the cell culture and that the SVC becomes positive before the antigenemia for the detection of CMV in peripheral blood, especially in the first blood sample.[29]
In another study, assays that analyzed 10,000 leukocytes had moderate analytical sensitivity, thereby exhibiting moderate positive predictive value (PPV) and specificity for the prediction of CMV disease in patients after stem cell transplantation. The sensitivity of RT-PCR depends on the assay conditions. PCR tests with high sensitivity have a low PPV and specificity, and threshold values need to be evaluated under clinically relevant conditions to obtain an appropriate specificity and PPV as close to 100% as possible to avoid unnecessary CMV treatment. In addition to the question of sensitivity, the availability of patient specimens may influence the choice of a test. pp65 antigen detection requires leukocytes from freshly collected blood samples, which cannot be stored or frozen. In contrast, RT-PCR can be performed with small volumes of plasma, which may be stored frozen for long periods without loss of DNA integrity.[30]
Ksouri, et al. have described that polymorphonuclear leukocytes (PMNLs)-based assays are more efficient in monitoring CMV reactivation, but for high-risk patients with graft-versus-host disease, more sensitive RT-PCR assays must be carried out.[31] A standardized RT-PCR assay is more appropriate than the antigen assay for detecting CMV. It allowed earlier diagnosis of active CMV infection and monitoring of the response to anti-CMV treatment.[32] The PCR detected all clinically significant CMV infections (>10 positive cells in pp65 test) and infections which required antiviral treatment. Other authors have described that the quantitative PCR appears to be a suitable alternative to diagnose and monitor CMV infections in transplant patients.[33] Therefore, we undertook this study to know the value of pp65 antigenemia using the culture technique.
Human fibroblasts have represented the conventional cell substrate for recovery of HCMV from clinical samples since the beginning of medical virology. Due to the increasing need for recovery of HCMV from the blood of immunocompromised patients, in our study, we have demonstrated the successful isolation of HCMV from human corneal fibroblast cultures. We have also demonstrated the correlation of pp65 antigenemia count of renal transplant patients and isolation of HCMV from the leukocytes of the same group.
The isolation of HCMV is not easy. As the experiment of isolation needs to be carried out with the same batch of fibroblast culture, we performed the viral isolation on 51 consecutive pp65 antigenemia-positive peripheral blood specimens. We would also like to state that the rate of isolation in the manuscript is 41.17% using the human fibroblast cell culture. In a study conducted by Veal et al.,[34] the HCMV isolation rate was 16.9%. In another study, Mazzulli et al. compared the isolation of HCMV and pp65 antigenemia assay and reported an isolation rate of 40.89%. The HCMV isolation rate reported in our study correlated with the results of Mazzulli et al.[35]
Human corneal fibroblast cultures have proven to be the best substrate for the isolation of the virus in this study. It has been proved that HCMV can be isolated from 42.85% of the pp65 antigenemia-positive individuals, but in our laboratory setup the cutoff value was 23 cells /2 × 105 cells.
From the literature it is evident that the cutoff pp65 value of 10 is considered to be significant in renal transplant patients,[333637] except a report made by Gerna et al. in which it is suggested that a pp65 antigenemia count of 100 was considered significant.[38] In India, the seroprevalence of HCMV is reported to be very high among normal population and renal transplant patients.[39–41] In our earlier report, we reported the rate of positivity of HCMV to be very high among the transplant patients.[27] Therefore a pp65 antigenemia count of 10 reported based on the Western literature[42–46] may not reflect the true situation of replication of HCMV in PBLs in Indian patients. It should also be borne in mind that pp65 antigenemia assay is subjective as it is prone to the visual errors of individuals reporting on the smears. Therefore, we attempted to estimate the significant pp65 antigenemia count that would have viable HCMV in the peripheral blood.
Despite the fact that pp65 antigenemia is the most valuable tool in the diagnosis of HCMV infections, the viral isolation has also been a useful tool in diagnostics of HCMV disease.
In conclusion, HCMV was successfully cultivated for the first time in India on human corneal fibroblast culture. A pp65 count of 23 was determined to be the value of clinical significance as it gives culture positive results among renal transplant patients.
Acknowledgment
The study was approved by the Research and Ethics Sub-Committee of our institute (study code no: 34-2003/P).
Source of Support: Nil
Conflict of Interest: None declared.
References
- Herpesvirus infection: An overview of the clinical manifestations. Scand J Infect Dis. 1991;80:15-20.
- [Google Scholar]
- Serious cytomegalovirus disease in the acquired immuno deficiency syndrome (AIDS) Ann Intern Med. 1988;108:585-94.
- [Google Scholar]
- Cytomegalovirus infection after organ transplantation: An update with special emphasis on renal transplantation. Transpl Int. 1989;2:147-64.
- [Google Scholar]
- Practices for cytomegalovirus diagnosis, prophylaxis and treatment in allogeneic bone marrow transplant recipients: A report from the working party for infectious diseases of the EBMT. Bone Marrow Transplant. 1993;12:399-403.
- [Google Scholar]
- Rapid detection of cytomegalovirus in MRC-5.cells inoculated with urine specimens by using low-speed centrifugation and monoclonal antibody to an early antigen. J Clin Microbiol. 1984;19:917-9.
- [Google Scholar]
- Cytomegalovirus excretion as a predictor of cytomegalovirus disease after marrow transplantation: Importance of cytomegalovirus viremia. J Infect Dis. 1990;162:373-80.
- [Google Scholar]
- Predictive value of cytomegalovirus viraemia for the occurrence of CMV organ involvement in AIDS. J Med Virol. 1990;32:160-3.
- [Google Scholar]
- Disseminated cytomegalovirus infection: Molecular analysis of virus and leukocyte interactions in viremia. J Clin Invest. 1988;81:75-81.
- [Google Scholar]
- Fibroblasts, epithelial cells, endothelial cells and smooth muscle cells are major targets of human cytomegalovirus infection in lung and gastrointestinal tissues. J Gen Virol. 1995;76:741-50.
- [Google Scholar]
- Circulating cytomegalovirus (CMV)-infected endothelial cells in patients with an active CMV infection. J Infect Dis. 1993;167:270-7.
- [Google Scholar]
- Human cytomegalovirus and human umbilical vein endothelial cells: Restriction of primary isolation to blood samples and susceptibilities of clinical isolates from other sources to adaptation. J Clin Microbiol. 2002;40:233-8.
- [Google Scholar]
- Human cytomegalovirus replicates abortively in polymorphonuclear leukocytes after transfer from infected endothelial cells via transient microfusion events. J Virol. 2000;74:5629-38.
- [Google Scholar]
- Epidemiology of cytomegalovirus infection after transplantation and immunosuppression. J Infect Dis. 1975;132:421-33.
- [Google Scholar]
- Isolation of human cytomegalovirus from peripheral blood T cells of renal transplant patients. J Lab Clin Med. 1982;99:92-7.
- [Google Scholar]
- Identification of the major late human cytomegalovirus matrix protein pp65 as a target antigen for CD81 virus-specific cytotoxic T lymphocytes. J Med Virol. 1994;43:103-10.
- [Google Scholar]
- Comparative analysis of fourteen individual human cytomegalovirus proteins for helper T cell response. J Gen Virol. 1995;76:153-60.
- [Google Scholar]
- Proliferative T cell responses to four human cytomegalovirus (HCMV)-specific proteins in healthy subjects and solid organ transplant recipients. J Infect Dis. 1995;172:879-82.
- [Google Scholar]
- Recognition of human cytomegalovirus gene products by HCMV-specific cytotoxic T cells. Virology. 1996;222:293-6.
- [Google Scholar]
- The human cytotoxic T-lymphocyte (CTL) response to cytomegalovirus is dominated by structural protein pp65: Frequency, specificity, and T-cell receptor usage of pp65-specific CTL. J Virol. 1996;70:7569-79.
- [Google Scholar]
- Isolation and expansion of cytomegalovirus-specific cytotoxic T lymphocytes to clinical scale from a single blood draw using dendritic cells and HLA-tetramers. Blood. 2001;98:505-12.
- [Google Scholar]
- Infections in solid organ transplant recipients. Clin Microbiol Rev. 1997;10:86-124.
- [Google Scholar]
- Quantification of cytomegalovirus: Methodologic aspects and clinical applications. Clin Microbiol Rev. 1998;11:5333-54.
- [Google Scholar]
- Risk factors for cytomegalovirus infection after human marrow transplantation. J Infect Dis. 1986;153:478-88.
- [Google Scholar]
- Ganciclovir prophylaxis to prevent cytomegalovirus infection after allogeneic marrow transplant. Ann Intern Med. 1993;118:173-8.
- [Google Scholar]
- Treatment of cytomegalovirus pneumonia with ganciclovir and intravenous immunoglobulin in patients with bone marrow transplant. Ann Intern Med. 1988;109:783-8.
- [Google Scholar]
- Clinical strategies for the management of cytomegalovirus infection and disease in allogeneic bone marrow transplant. Bone Marrow Transplant. 1997;19:135-42.
- [Google Scholar]
- pp65 antigenemia and real time polymerase chain reaction (PCR) based-study to determine the prevalence of human cytomegalovirus (HCMV) in kidney donors and recipients with follow-up studies. Virol J. 2010;7:322-8.
- [Google Scholar]
- Comparison of PCR and pp65 antigenemia assay with quantitative shell vial culture for detection of cytomegalovirus in blood leukocytes from solid-organ transplant recipients. J Clin Microbial. 1994;32:997-1003.
- [Google Scholar]
- Shell-vial culture and pp65 antigenemia assay in the detection of cytomegalovirus in the first blood sample of renal transplant recipients. J Med Virol. 1998;55:240-2.
- [Google Scholar]
- Quantitative real-time PCR compared with pp65 antigen detection for cytomegalovirus (CMV) in 1122 blood specimens from 77 patients after allogeneic stem cell transplantation: Which test better predicts CMV disease development? Clin Chem. 2003;49:1683-5.
- [Google Scholar]
- Analysis of cytomegalovirus (CMV) viremia using the pp65 antigenemia assay, the amplicor CMV test, and a semi-quantitative polymerase chain reaction test after allogeneic marrow transplantation. Transpl Infect Dis. 2007;9:16-21.
- [Google Scholar]
- Algorithm based on CMV kinetics DNA viral load for preemptive therapy initiation after hematopoietic cell transplantation. J Med Virol. 2011;83:490-5.
- [Google Scholar]
- Comparison of plasma polymerase chain reaction and pp65-antigenemia assay in the quantification of cytomegalovirus in liver and kidney transplant patients. J Clin Virol. 2001;22:111-6.
- [Google Scholar]
- Novel DNA assay for cytomegalovirus detection: Comparison with conventional culture and pp65antigenemia assay. J Clin Microbiol. 1996;34:3097-100.
- [Google Scholar]
- Multicentre comparison of the digene hybrid capture CMV DNA assay (version 2.0), the pp65 antigenemia assay, and cell culture for detection of cytomegalovirus viremia. J Clin Microbiol. 1999;37:958-63.
- [Google Scholar]
- Antigenemia for cytomegalovirus in renal transplantation: Choosing a cutoff for the diagnosis criteria in cytomegalovirus disease. Transplant Proc. 2005;37:2781-3.
- [Google Scholar]
- Comparison of pp65 antigenemia quantitative PCR and DNA hybrid capture for detection of cytomegalovirus in cytomegalovirus in transplant recipients and AIDS patients. J Virol Methods. 2007;143:23-8.
- [Google Scholar]
- Diagnosis of human cytomegalovirus infections in the immunocompromised host. Clin Diagn Virol. 1996;5:181-6.
- [Google Scholar]
- Seroprevalence of cytomegalovirus among voluntary blood donors in Delhi, India. J Health Popul Nutr. 2002;20:348-51.
- [Google Scholar]
- Birth prevalence and natural history of congenital cytomegalovirus infection in a highly seroimmune population. Clin Infect Dis. 2009;49:522-8.
- [Google Scholar]
- Comparison between viremia and antigenemia for detection of cytomegalovirus in blood. J Clin Microbiol. 1988;26:2531-5.
- [Google Scholar]
- A prospective study comparing quantitative cytomegalovirus (CMV) polymerase chain reaction in plasma and pp65 antigenemia assay in monitoring patients after allogeneic stem cell transplantation. BMC Infect Dis. 2006;6:167.
- [Google Scholar]
- Relationship between pp65 antigenemia levels and real-time quantitative DNA PCR for HCMV management in immunocompromised patients. BMC Infect Dis. 2007;7:138.
- [Google Scholar]
- Cytomegalovirus disease in patients with acquired immunodeficiency syndrome.Report of 63 cases. Med Clin (Barc). 1993;100:41-5.
- [Google Scholar]
- Comparison of two leukocyte extraction methods for cytomegalovirus antigenemia assay. J Clin Microbiol. 1996;34:182-4.
- [Google Scholar]







