Translate this page into:
Everolimus for the treatment of CD20+ diffuse large B-cell lymphoma in a renal allograft recipient
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
A 42-year-old man received a renal allograft from his mother and achieved good graft function (serum creatinine (SCr), 0.9 mg/dL). Maintenance of immunosuppression included the use of prednisolone (10 mg/day), tacrolimus (level 5-8 ng/mL), and mycophenolate (1.5 gm/day). Two years after the transplantation, he developed lymph-node (LN) swelling in the submandibular area (right > left) without ulceration/fever, but weight loss was present. Histopathology of the LN revealed non-Hodgkin's lymphoma (NHL), diffuse large B-cell (DLBCL, CD20+ CD3+ LCA+) type Figure 1a and b with perinodal extension and tumor-free salivary gland tissue. The bone-marrow histology was normal. Polymerase chain reaction of ruled out cytomegalovirus, herpes simplex virus, varicella zoster virus, and Epstein-Barr virus infections. Laboratory investigations revealed normal complete blood count and liver function tests. SCr was 1 mg/dL, with no proteinuria; lactate dehydrogenase, 479 IU/dL; and uric acid, 2.6 mg/dL. The Eastern Cooperative Oncology Group performance status was grade 0. He was able to work or carry out any normal activity; but no special care was needed. The Karnofsky performance status scale was 90.
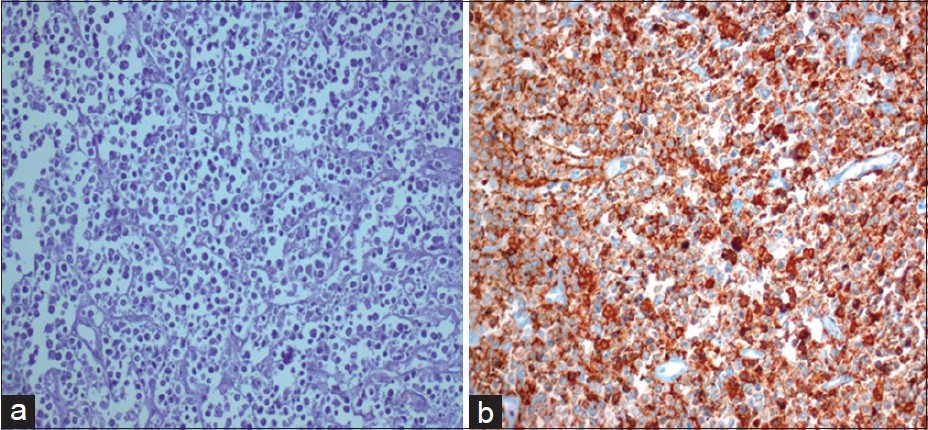
- (a) Histopathology revealed diffuse large B cell lymphoma of the lymph node. (b) CD20 positivity on immunohistochemistry
Tacrolimus and mycophenolate were discontinued, prednisone was given at a dose of 7.5 mg/day, low-dose everolimus (1-1.5 mg/day, and trough concentration (C0) 4-5.5ng/mL) was initiated. The NHL was treated with R-CHOP regime. Complete clinical and radiological remission was achieved after six cycles. He was continued on prednisolone and everolimus with no side effects. He continues to be in complete remission with SCr. –1.1 mg/dL without proteinuria at 15 months’ follow-up. Combined fluorodeoxyglucose, positron emission tomography, and computed tomography (FDG-PET/CT) scanning revealed inactive disease.
Lymphoproliferative disorders are serious and potentially fatal complications of chronic immunosuppression in organ-transplant recipients. In the new era of immunosuppression, despite a lower occurrence, malignancy tends to appear earlier after transplantation. Switching calcineurin inhibitor to sirolimus or everolimus was associated with a favorable outcome in post-transplant malignancy.[12] We used everolimus due to the encouraging results of an mTORi-based regimen for post-transplant malignancies.[1–7] Everolimus has shown antiangiogenic and antiproliferative activities on cell lines derived from human tumors and on xenograft models of human tumors.[3] Activation of PI3-K, Akt, growth factor receptors, Ras/Raf, and PTEN are responsible for inappropriate activation of the signaling pathway leading to PTLD. Everolimus displays a potent inhibitory effect by inhibiting these pathways in a dose range, leading to prevention of allograft rejection, and may prove effective in both the prevention and treatment of PTLDs in transplant patients.[5] In addition, MTORi reduces the morbidity and mortality after kidney transplantation.
Our report suggests that immunosuppressive therapy with everolimus is safe and efficient for renal recipients who develop DLBCL. Whether everolimus has antitumor effects or any synergistic effect that may be beneficial in the treatment of DLBCL should be explored in future trials.
References
- Leflunomide with low-dose everolimus for treatment of Kaposi's sarcoma in a renal allograft recipient. Nephrol Dial Transplant. 2011;26:3412-5.
- [Google Scholar]
- Monotherapy rapamycin in renal transplant recipients with lymphoma successfully treated with rituximab. Transplant Proc. 2009;41:2435-7.
- [Google Scholar]
- mTOR inhibitor RAD001 (everolimus) has antiangiogenic/vascular properties distinct from a VEGFR tyrosine kinase inhibitor. Clin Cancer Res. 2009;15:1612-22.
- [Google Scholar]
- Sirolimus therapy after early cyclosporine withdrawal reduces the risk for cancer in adult renal transplantation. J Am Soc Nephrol. 2006;17:581-9.
- [Google Scholar]
- Results of the conversion to everolimus in renal transplant recipients with posttransplantation malignancies. Transplant Proc. 2010;42:277-9.
- [Google Scholar]
- Maintenance immunosuppression with target-of-rapamycin inhibitors is associated with a reduced incidence of de novo malignancies. Transplantation. 2005;80:883-9.
- [Google Scholar]
- Clinical evidence on the use of anti-mTOR drugs in renal transplantation. Nefrologia. Nefrologia. 2011;31:27-34.
- [Google Scholar]






