Translate this page into:
A Mysterious Case of Pleuroperitoneal Leak Leading to Recurrent Hydrothorax in a Child with Nephrotic Syndrome
Corresponding author: Jasmine Sethi, Department of Nephrology, Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, India. E-mail: jasmine227021@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vijayakumar NA, Sethi J, Nadda N, Venkatasubramanian V, Mittal BR. A Mysterious Case of Pleuroperitoneal Leak Leading to Recurrent Hydrothorax in a Child with Nephrotic Syndrome. Indian J Nephrol. 2024;34:518-9. doi: 10.25259/ijn_567_23
Abstract
We describe a young girl of steroid resistant nephrotic syndrome with rapidly reaccumulating right sided pleural effusion. On evaluation, the patient was diagnosed with right side pleuro-peritoneal leak leading to recurrent right hydrothorax. To the best of our knowledge, hydrothorax due to transdiaphragmatic shunting in a nephrotic patient has not been reported earlier.
Keywords
Nephrotic syndrome
Pleural effusion
Pleuroperitoneal leak
Hydrothorax
Shunt
Introduction
Serous effusions are a well-known complication of severe nephrotic syndrome. However, recurrent hydrothorax in a nephrotic child due to pleuroperitoneal leak is not reported in the literature. We emphasize the importance of looking beyond the common etiologies of transudative pleural effusion, such as decompensated congestive heart failure, nephrotic syndrome, hepatic hydrothorax, or severe hypoalbuminemia, and consider diaphragmatic leak as one of the differentials. Pleuroperitoneal leak is a rare but a treatable important complication and needs consideration in any patient presenting with recurrent unilateral pleural effusion.
Case Report
A 13-year-old girl presented with recurrently accumulating right-sided pleural effusion for 1 year. She also had history of mild pedal edema, abdominal fullness, and persistent heavy proteinuria. She denied any history of fever, trauma to chest, cough, weight loss, jaundice, palpitations, joint pains, or alternate medicine intake. She was diagnosed with nephrotic syndrome (biopsy-proven cellular variant of focal segmental glomerulosclerosis) 3 years back. She had a secondary steroid- and calcineurin inhibitor-resistant phenotype. Clinical exome sequencing did not reveal any pathogenic mutation. Currently, her medication included angiotensin receptor blockers/statins/diuretics and prophylactic anticoagulation with warfarin. Physical examination revealed grade 1 pedal edema, ascites, and gross right-sided pleural effusion with tracheal shift to the left side. Lab parameters revealed hemoglobin of 11 g/dl, serum creatinine of 0.6 mg/dl, serum albumin of 1.7 g/dl, serum cholesterol of 300 mg/dl, and 24-h urine protein excretion of 6 g/day. Rest of the liver function tests and coagulogram were normal. Chest X-ray revealed gross right pleural effusion with mediastinal shift, and transthoracic echocardiography revealed normal left ventricular ejection fraction. Contrast-enhanced computed tomography (CT) chest and abdomen showed only right-sided pleural effusion and ascites with no lymphadenopathy or evidence to suggest tuberculosis [Figure 1]. A therapeutic right side yielded transudative effusion. Pleural fluid cytology, GeneXpert test for tuberculosis DNA and culture were negative. To determine whether communication existed between pleural and peritoneal cavity, Tc-99 sulfur colloid scintigraphy was performed, which showed prompt (within 5 min) appearance of tracer on the right side with no tracer leak in the left hemithorax [Figure 2a–c]. Thus, the etiology of recurrent hydrothorax was likely due to congenital diaphragmatic defect that got exacerbated by persistently elevated intra-abdominal pressure from ascites due to nephrotic state. A cardiothoracic surgery consult was taken, and the patient is planned for video-assisted thoracoscopic surgery (VATS). For the basic disease, patient was started on rituximab pulse (375 mg/m2) and has received 2 pulses till now.

- CT scan of thorax (axial view) showing unilateral right-sided pleural effusion (white arrowhead). CT = computed tomography.
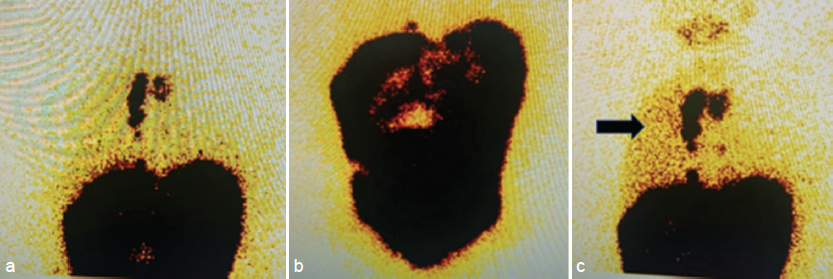
- (a) Tc-99 sulfur colloid scintigraphy showing multiple static images of the abdomen and chest acquired immediately and at 1 and 4 h following intraperitoneal injection of 99m Tc sulfur colloid. (b) The image acquired 1 h after intraperitoneal injection shows the heterogeneous intraperitoneal distribution of the tracer in the abdomen. (c) There are also multiple foci of tracer activity in the thoracic region, which intensify at 4 h (marked by black arrowhead).
Discussion
Pleuroperitoneal leak is an uncommon complication mostly reported in patients on peritoneal dialysis.1 The resultant pleural effusion is usually transudative, and the postulated mechanism is due to increased intra-abdominal pressure in the presence of underlying congenital or acquired diaphragmatic defects. In most cases, as ours, the effusion is right sided as the left side is partially protected by the heart and the pericardium, resulting in a lower incidence of leaks. Till date, as to the best of our knowledge, we could find one reported case of chylous ascites and chlothorax due to transdiaphragmatic shunting in an adult patient with nephrotic syndrome.2 In view of the refractory nephrotic state of our patient, serositis due to severe hypoalbuminemia can be considered as a differential diagnosis. However, recurrent unilateral pleural effusion in the absence of significant anasarca and confirmation with scintigraphy point to a diaphragmatic defect as the cause in our patient. Definitive diagnosis is usually made by peritoneal scintigraphy. However, a CT scan with intraperitoneal (IP) radiocontrast administration can also demonstrate the leak.
Conclusion
Management includes conservative therapies like salt restriction/aggressive diuretic therapy and chemical pleurodesis. Minimally invasive surgical interventions like VATS, with or without diaphragmatic repair, can also be tried in refractory cases.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
References
- Pleuroperitoneal leak: An unusual cause of acute shortness of breath in a peritoneal dialysis patient. Case Rep Radiol. 2014;2014:614846.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Chylous ascites and chylothorax due to the existence of transdiaphragmatic shunting in an adult with nephrotic syndrome. Nephrol Dial Transplant. 2005;20:1501-2.
- [CrossRef] [PubMed] [Google Scholar]







