Translate this page into:
A Rare Case of Peritonitis in a Patient on CAPD for Nine Years
Corresponding author: Georgi Abraham, Department of Nephrology, MGM Healthcare, Chennai, Tamil Nadu, India. E-mail: abraham_georgi@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Parthasarathy A, Mathew M, Sundar D, Abraham G. A Rare Case of Peritonitis in a Patient on CAPD for Nine Years. Indian J Nephrol. doi: 10.25259/IJN_64_2024.
Abstract
We report a case of peritonitis due to multi-drug-resistant Escherichia coli in a patient with diabetic kidney disease on continuous ambulatory peritoneal dialysis for nine years. As the peritonitis did not resolve with conventional medical therapy, a contrast-enhanced CT was done, which showed superior mesenteric artery thrombosis with bowel ischemia. The peritoneal dialysis catheter was removed, and appropriate antibiotics were continued as per International Society for Peritoneal Dialysis guidelines. A year later, the patient while on maintenance hemodialysis presented with obstructive jaundice due to a growth in the ampulla of vater.
Keywords
Bowel ischemia
CAPD
peritonitis
peritoneal dialysis
thrombosis
Introduction
Peritonitis is a common complication in patients on continuous ambulatory peritoneal dialysis. In certain cases, when the peritonitis episodes are not resolving, the gut pathology should be ruled out.1 Here, we present a case of underlying superior mesenteric artery (SMA) thrombosis responsible for bowel-leak peritonitis.
Case Report
A 64-year-old man with diabetic kidney disease on continuous ambulatory peritoneal dialysis for 9 years presented with cloudy peritoneal effluent. The peritoneal fluid grew MDR E. coli. as it was sensitive to tigecycline, he was treated with the same antibiotic intra-peritoneally. As his peritonitis was not resolving, contrast-enhanced CT abdomen was done which showed severe luminal narrowing of SMA caused by soft atheromatous plaque extending into the branches supplying the proximal and mid-jejunal loops in the left lumbar region and umbilical region [Figure 1]. 2D-Echo with doppler was normal. Investigations showed Hb, 10.4 g/dl; WBC count, 11.84 x 103/µL; N, 94.1%; L, 3.2%; M, 1.9%; E, 0.1%; B, 0.7%; platelet count, 222 x 103/µL; calcium, 8.8 mg/dl; phosphorus, 3.5 mg/dl; electrolytes, Na 133 mmol/L, K 4.31 mmol/L, Cl 95.1 mmol/L; HCO3, 18.7 mmol/L; LFT, total protein 5.8 g/dL; albumin, 2.6 g/dL; procalcitonin, 3.99 ng/ml; CRP, 387.95 mg/L; D-dimer, 2445 ng/mL; and plasma fibrinogen, 869 mg/dL. Emergency laparotomy with resection and anastomosis of ischemic small bowel along with peritoneal catheter removal was done, and the patient switched over to hemodialysis, after which he did not experience further clotting episode.
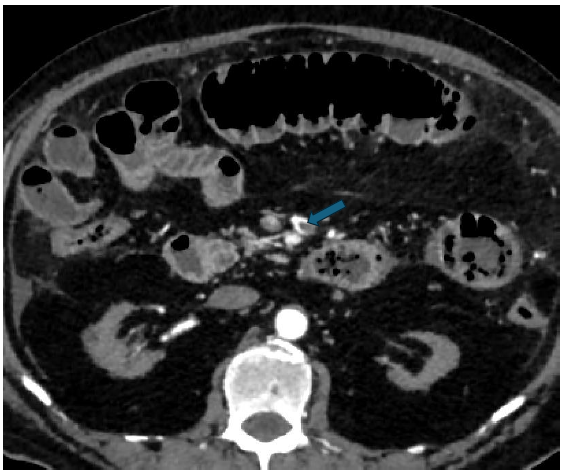
- Superior mesenteric artery thrombosis (blue arrow).
On 4th May 2023, the patient came with complaints of fever and jaundice for 2 days. Investigations showed total bilirubin of 7.35 mg/dl 7.08 mg/dl, indirect bilirubin 0.27 mg/dl, ALT 56.1 U/L, AST 43.3 U/L, ALP 594.7 U/L, GGT 797.5 U/L, total protein 5.9 g/dL, albumin 2.8 g/dL, and globulin 3.1 g/dL, suggesting neutrophilic leukocytosis with obstructive jaundice. A permanent metallic stent was implanted in the common bile duct, which relieved the jaundice.
PET-CT scan showed metabolically active enhancing lesions in the ampulla of vater. Culture from the blood and bile showed the growth of E. coli and Serratia marcescens, respectively. He was treated with appropriate antibiotics. Endoscopic biopsy of the ampullary growth showed fragmented adenomatous polypoidal lesion with high-grade dysplasia [Figure 2].
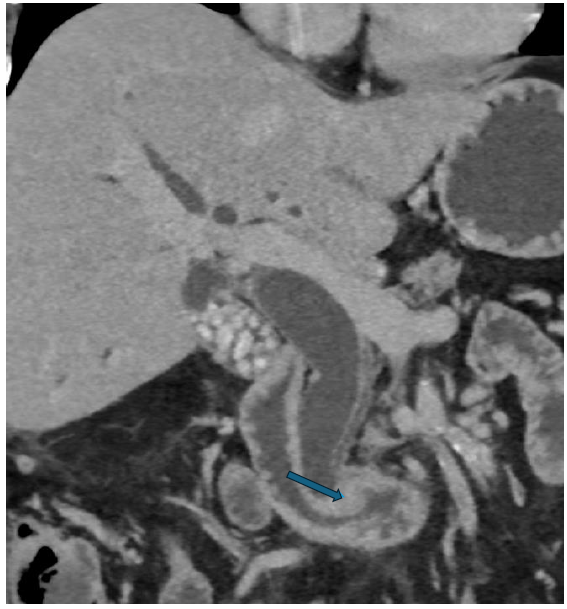
- Contrast Enhanced-CT abdomen - Delayed phase - coronal section - showing enhancing polypoidal lesion in ampulla causing gross upstream dilatation of intra and extra hepatic biliary radicle dilatation (blue arrow).
Discussion
Although diabetic patients on CAPD have mild hypercoagulability, we have not come across a similar report.1 The SMA thrombosis was diagnosed only with the help of CECT. We speculate that the thrombus may be idiopathic or due to a premalignant condition words struck. Re-insertion and re-initiation for peritoneal dialysis were not considered due to bowel–ischemia.2,3 Although previous reports of the three patients mentioned that SMA thrombosis occurred after peritonitis episodes, SMA thrombosis was the reason for bowel-leak peritonitis in this patient. This case highlights the importance of investigations for ischemic bowel when the peritonitis does not respond to conventional therapy.
Conclusion
Evidences have mentioned superior mesenteric artery thrombosis occurring after peritonitis episodes. Whereas in this case, superior mesenteric artery thrombosis is the reason for bowel-leak peritonitis. The underlying thrombus may be due to the premalignant condition leading to bowel ischemia.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
References
- Superior Mesenteric artery syndrome complicating dialysis patients with peritoneal failure--report of 3 cases. Clin Nephrol. 2011;75:37-41.
- [CrossRef] [PubMed] [Google Scholar]
- Differences in coagulation between hemodialysis and peritoneal dialysis. Perit Dial Int. 2014;34:33-40.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Ischaemic Enteritis in a Patient with chronic renal failure: Diagnosis and management decisions. BMJ Case Rep. 2010;2010:bcr0920092249.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







