Translate this page into:
A Rare Parasitic Infection from the Common Cockroach: A Case of Lophomonas Blattarum from a Tertiary Center in Kerala
Corresponding author: Sunil George, Department of Nephrology, Baby Memorial Hospital, Kozhikode - 673004, Kerala, India. E-mail: drsunilgeo@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mavoor PP, George S, Chetambath R, Poornima MV. A Rare Parasitic Infection from the Common Cockroach: A Case of Lophomonas Blattarum from a Tertiary Center in Kerala. Indian J Nephrol. 2024;34:387-9. doi: 10.25259/ijn_520_23
Abstract
Immunocompromised patients are prone to various opportunistic infections. Most of the infections are easily detectable through staining, culture, and polymerase chain reaction techniques. Nevertheless, it is also important to have wet smear examinations of samples. We present a case of pneumonia in a post-transplant recipient who was on immunosuppressants and detected to have an infection from the parasite, lophomonas blattarum, which usually resides in the hindgut of cockroaches.
Keywords
Blattarum
Lophomonas
Pneumonia
Post renal transplant
Introduction
We present a renal allograft recipient with a right upper lobe consolidation caused by lophomonas blattarum, a commensal living in the hindgut of cockroaches. There has been discussions on the need of electron microscopy, and methods relying on polymerase chain reaction for the identification of the organisms. But they are not readily available, and we have identified the organism with staining methods. Though the infection responded to treatment with metronidazole, he had other clinical problems and he succumbed to the illness.
Case Report
A 40-year-old renal allograft recipient presented in May 2023 with anorexia, fatigue, and loose stools of around 1 week duration. He had his first transplant in 2003 with his father as the donor and the second transplant in 2017 with his aunt as the donor. He was on triple immunosuppressants (tacrolimus, deflazacort, and mycophenolate mofetil). Until the COVID pandemic, he was on regular follow-up with stable graft functions (creatinine 1.4 mg/dl). He took a train journey and gave a history of consuming food from a hotel, following which he developed the present symptoms. He also had fever, shortness of breath, and oliguria. The clinical examination showed tachypnoea and oxygen desaturation. He has coarse crackles in the right infrascapular area. Lab parameters are shown in Table 1.
| Tests | |
|---|---|
| Hemogram |
Hemoglobin 12 g/dl Total WBC count 25,400/cu.mm Differential count polymorphs 91.8% Lymphocytes 3% Platelet 291,000/cu.mm |
| Renal functions |
Blood urea 105 mg/dl Serum creatinine 5.6 mg/dl |
| Liver functions | Normal except for mild elevation of aspartate aminotransferase (56 U/L) |
| Serum proteins |
Total protein 6.6 g/dl Serum albumin 3.4 g/dl |
| Serum sodium | 126 meq/l |
| Serum potassium | 3.3 meq/l |
| Serum calcium | 7.9 g/dl |
| Serum magnesium | 1 mg/dl |
| Serum phosphorus | 1.7 mg/dl |
| Serum uric acid | 15.6 mg/dl |
| CRP | 290 ng/l |
| PT/INR | 14.8 s/1.43 |
| Urine routine | Protein 3+, RBC 5–8/hpf, pus cells 0–2/hpf |
| Blood culture | Sterile |
| Influenza polymerase chain reaction | Negative |
| Comprehensive respiratory panel | Streptococcus pneumoniae |
| Bronchoalveolar lavage | Gram stain, culture sensitivity, acid-fast bacilli negative, and cytology negative for malignancy |
WBC: white blood cell, CRP: C-reactive protein, PT/INR: prothrombin time/international normalized ratio, RBC: red blood cell
Chest X-ray showed nonhomogeneous opacity in the right upper zone, suggestive of right pneumonia with minimal right pleural effusion. Bronchoalveolar lavage showed motile flagellated trophozoites of Lophomonas blattarum and it was confirmed with special stains [Figure 1].
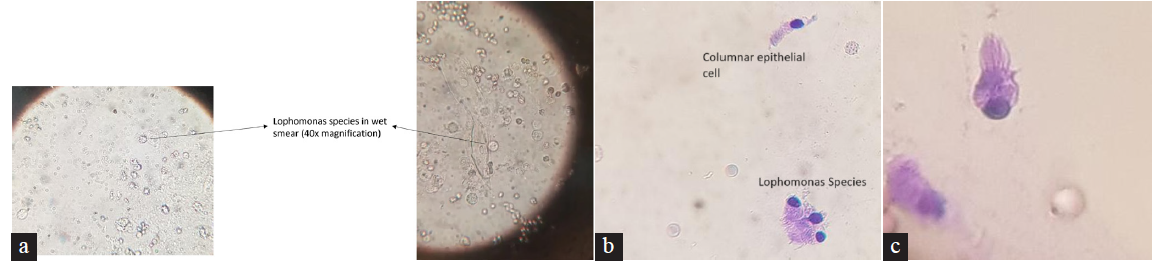
- (a) Wet mount smear (40× magnification), (b) staining with methylene blue (40× magnification), (c) staining with Papanicolaou stain (100× magnification).
The acid-fast bacillus culture, fungal smear, and fungal cultures were negative. Stool examination was normal and stool culture was negative. Computed tomography (CT) thorax showed consolidation changes involving the right lung with mediastinal lymph nodes. He was managed with broad-spectrum antibiotics, parenteral metronidazole, along with high flow nasal oxygen (HFNC) and optimization of the dose of immunosuppressants. He was given four sessions of hemodialysis, over a span of a week, he became nonoliguric and could be weaned off from hemodialysis; HFNC could be withdrawn and he maintained adequate saturation on minimal oxygen requirement via nasal cannula. The chest X-ray and CT images before and after treatment are shown in Figure 2.
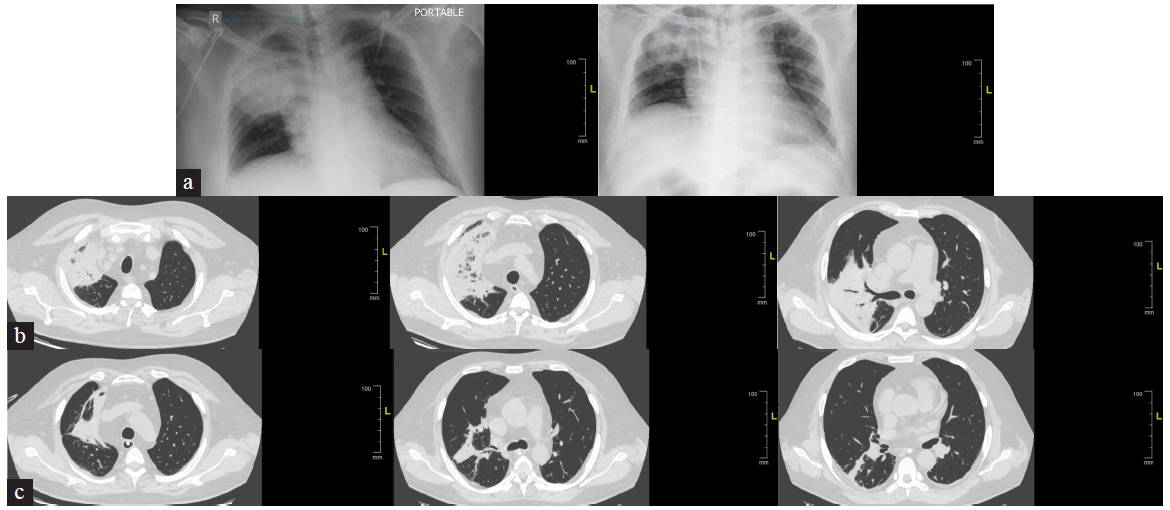
- Images before and after treatment: (a) Chest X-ray before and after treatment. (b) CT images before treatment. (c) CT images after treatment. CT: computed tomography.
The patient continued to have hypokalemia and hypomagnesemia with abdominal distension. CT scan of the abdomen showed dilated bowel loops. He had fever spikes and antibiotics were escalated. On the 13th day of hospitalization, he developed acute right-sided abdominal pain with tachypnea, oxygen desaturation, and hypotension requiring multiple vasopressor support suggestive of gastrointestinal sepsis and he expired.
Discussion
Lophomonas blattarum is a flagellate protozoan parasite which was originally described as a commensal in the gut of cockroaches. It causes upper and lower respiratory tract infections.1
All over the world, less than 200 cases have been reported, around 136 from China. Only four2–5 cases have been reported from India.
The bronchopulmonary site is most commonly infected given the nature of entry of the pathogen by inhalation. Some infrequent sites affected include the maxillary sinus, urinary tract, and uterus. Eosinophilia is found in 21.5–35% of cases only. It has also been reported in an immunocompetent patient.2
Many discussion regarding the correct identification of the parasite and differentiation from ciliated columnar respiratory epithelial cells has been given in the existing literature. The differentiating features are tabulated in Table 2.6
| Feature | Lophomonas blattarum | Ciliated epithelial cells |
|---|---|---|
|
Shape |
Pyriform or spherical |
Conical or columnar |
|
Flagella/cilia |
Flagellar tuft with >50 flagella Unequal length of flagella Irregularly arranged |
Ciliary tuft with ∼200 cilia Uniform length Regularly arranged |
|
Nucleus |
Located at the base of the flagellar tuft, both at the anterior end of the cell |
Located at the bottom of the cell, opposite to the ciliary tuft, which emerges from the apical face of the cell |
|
Others |
The axial filament may be found at the posterior end No terminal bar below the origin of flagella |
Absent A marked terminal bar at the apical end of the cell is present just below the origin of cilia |
The parasite can be stained by the Papanicolaou method, Wheatley’s trichrome stain, or by regular Giemsa or Wright stain. In unstained fresh specimens, a characteristic to-and-fro movement can be seen. The organism may be detected by polymerase chain reaction in the nasal discharge.
Metronidazole is the treatment of choice, at the usual dose of 500 mg every 8 h orally for 7–10 days in adults, and 7.5 mg/kg every 8 h in children. A single intravenous dose of 15 mg/kg over 1 h (as a loading dose), followed by 7.5 mg/kg every 6 h has also been used. Tinidazole is also used as an alternative drug.1
Conclusion
Even when a conventional pathogen has been identified as a cause of respiratory tract infection, it is important to look for such uncommon organisms; right from the initial wet mount smear examination of the bronchoalveolar lavage fluid so that the indicated treatment can be initiated and the infection responds.
Conflicts of interest
There are no conflicts of interest.
References
- Lophomonas blattarum: A new flagellate causing respiratory tract infections. Trop Parasitol. 2020;10:7-11.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Lophomonas blattarum infection in immunocompetent patient. Lung India. 2016;33:667-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Dual infection with pulmonary tuberculosis and Lophomonas blattarum in India. Int J Tuberc Lung Dis. 2015;19:368-9.
- [CrossRef] [PubMed] [Google Scholar]
- Broncho-pulmonary infection by Lophomonas blattarum: A case report. Int J Infect Dis. 2020;101:175-6.
- [CrossRef] [Google Scholar]
- A rare case of bronchopulmonary infection due to lophomonas blattarum: Case report and review of literature. Int J Health Sci Res. 2015;5
- [Google Scholar]
- Lophomonas blattarum Infection or Just the Movement of Ciliated Epithelial Cells? Chinese Med J. 2016;129:739-42.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]








