Translate this page into:
A Unique Case of Renal Infiltration by Lymphoplasmacytic Lymphoma with Cast Nephropathy
Address for correspondence: Dr. Kiran P. Malhotra, Additional Professor, Department of Pathology, Dr. Ram Manohar Lohia Institute of Medical Sciences, Gomti Nagar, Lucknow - 226 010, Uttar Pradesh, India. E-mail: drkiranpreetmalhotra@yahoo.co.in
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
A 65-year-old male presented with dull pain abdomen, anorexia and weakness for 3 months. Cervical lymphadenopathy and moderate hepatosplenomegaly was present. Total leucocyte count were raised (49,440 cells/cmm) with marked lymphocytosis and atypical lymphocytes. Serum Creatinine was 2.74 mg/dl. Serum protein and albumin were 9.53 and 3.54 g/dl. Urine protein was 2.5 gm/day with inactive sediments. β2 microglobulin was 13,800 mcg/L. Serum free light chain assay showed Kappa/Lambda ratio of 77.56. No skeletal lesions were identified.
Among the differentials considered for the renal disease was lymphoma infiltration of kidney, favoured by presence of hepatosplenomegaly. However, non-nephrotic illness and lack of renal mass on radiology countered it. Myeloma cast nephropathy was considered due to renal dysfunction, anemia, reversed Albumin: Globulin ratio, non-albumin proteinuria and elevated β2 Microglobulin. However, it did not explain hepatosplenomegaly, lymphadenopathy, atypical lymphocytosis and non-existent bone lesions. Organomegaly and paraproteinemia suggested primary amyloidosis; but non-nephrotic presentation and elevated creatinine were against it.
Renal biopsy showed intense interstitial infiltrate of medium-sized atypical lymphoid cells, positive for CD-20 and negative for CD-3. CD-138 highlighted numerous plasma cells with Kappa restriction. Amyloid stains were negative. Bone marrow biopsy showed similar infiltration. Few renal tubular fractured hyaline casts were noted [Figure 1]. Lymphoplasmacytic lymphoma (LPL) with Kappa light chain cast nephropathy was diagnosed. The patient was treated with Bortezomib, dexamethasone and plasmapheresis. On one-month follow-up, significant reduction of serum creatinine (to 1.6 mg/dl), serum IgM and Kappa light chains was recorded.
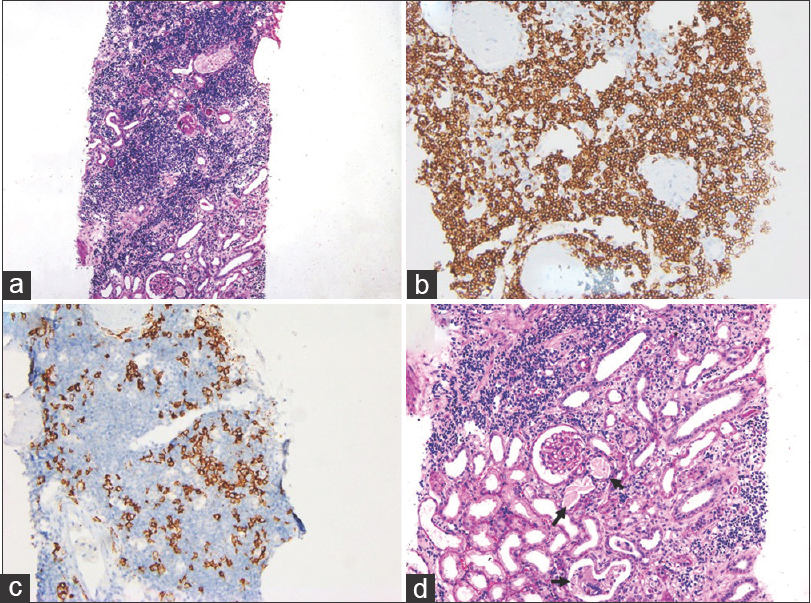
- Sections from renal biopsy showing (a) intense interstitial infiltrate of atypical lymphocytes (Periodic Acid Schiff, ×100); (b) CD20 positivity in atypical lymphocytes (Diaminobenzidine, ×200); (c) CD138 positivity highlighting plasma cells (Diaminobenzidine, ×200) and (d) Fractured renal tubular casts (arrows) (Periodic Acid Schiff, ×200)
LPL is a lymphoproliferative disorder characterized by lymphomatous infiltration of lymph nodes, hepatosplenomegaly and serum immunoglobulin M paraprotein. Renal infiltration is rarely seen.[1] Cast nephropathy though common in Multiple Myeloma is exceptional in LPL. Paraproteins are nephrotoxic and can cause acute kidney injury.[2] We report a unique case with renal infiltration by LPL with concomitant renal failure attributable to cast nephropathy. A single similar case was identified in Mayo Clinic archives over twenty years.[2] Renal biopsy is of utility in LPL in revealing cellular infiltration, tubulo-interstitial lesions, amyloid and non-amyloid glomerulopathy. Tubulointerstitial lesions herald the worst prognosis in LPL and could limit the renal response to haematological treatment.[2]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Renal disease related to Waldenström macroglobulinaemia: Incidence, pathology and clinical outcomes. Br J Haematol. 2016;175:623-30.
- [Google Scholar]
- Kidney involvement of patients with waldenström macroglobulinemia and other IgM-producing B cell lymphoproliferative disorders. Clin J Am Soc Nephrol. 2018;13:1037-46.
- [Google Scholar]






