Translate this page into:
Acute Renal Infarction – A Rare Thrombotic Complication in Essential Thrombocytosis
Corresponding author: MP Shamsudheen, Department of Nephrology, Government Medical College (GMC), Ernakulam, Kerala, India. E-mail: drshamsudheenmp@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shamsudheen MP, Samuel U. Acute Renal Infarction – A Rare Thrombotic Complication in Essential Thrombocytosis. Indian J Nephrol. doi: 10.25259/IJN_121_2025
Abstract
Renal infarction is an arterial vascular event causing irreversible damage to kidney tissues. This case report highlights acute renal infarction as a thrombotic complication in a patient with essential thrombocytosis and the consideration of hypercoagulable states in its differential diagnosis.
Keywords
Essential thrombocytosis
Hypercoagulable state
Renal infarction
Thrombotic complication
Introduction
Acute renal infarction (ARI) is a rare but potentially serious condition, frequently missed or diagnosed late due to symptoms that mimic common disorders such as nephrolithiasis and pyelonephritis. While ARI’s etiology is often attributed to embolisms caused by events like atrial fibrillation or atherosclerosis, it can occur in hypercoagulable states like essential thrombocytosis (ET). Although venous thromboembolism and arterial thrombosis in cerebral or coronary circulation are more frequently associated with ET, renal infarction remains rare.
Case Report
A 44-year-old lady, diabetic for 8 years, presented to our emergency department with severe left loin pain lasting 10 days. She did not have fever, vomiting, dysuria, or hematuria. She was conscious and afebrile, with an 88/min pulse rate, and 140/90 mmHg blood pressure. Her general physical and systemic examination was unremarkable, with no renal angle tenderness.
Blood analysis revealed thrombocytosis (5.8 lakh/µL) with normal hemoglobin level, total leukocyte count, and liver and renal parameters. Urine examination was noncontributory. Lactate dehydrogenase (LDH) level was elevated (551 U/L), but serum amylase and c-reactive protein (CRP) were normal. An abdominal ultrasonogram showed normal kidneys, with no evidence of renal stones or hydronephrosis.
A contrast-enhanced computed tomography (CECT) scan was used to investigate this persistent loin pain of unclear etiology. It revealed multiple wedge-shaped, non-enhancing, hypodense areas in the left kidney, suggestive of infarcts and thrombus in segmental renal arteries and a suprarenal aorta with partial occlusion [Figure 1a]. Interventional radiology and cardiology services recommended no intervention for this partial occlusion with normal renal parameters. Intravenous hydration, analgesics, and unfractionated heparin (later switched to rivaroxaban) were administered.
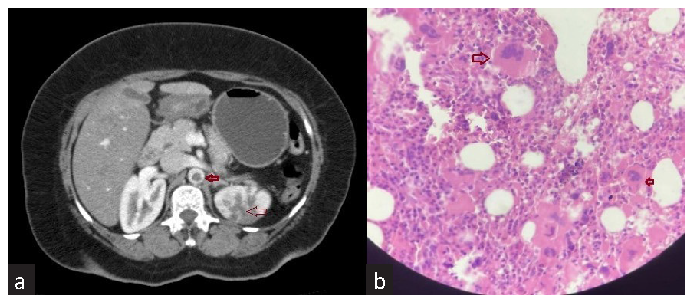
- (a) Contrast-enhanced CT abdomen showing infarcts in left kidney (thin red arrow) and thrombus in suprarenal aorta (thick red arrow). (b) Bone marrow image showing megakaryocytic (thick red arrows) hyperplasia.
The echocardiography and electrocardiogram were normal. Immunological tests, like antinuclear antibodies and antiphospholipid antibodies, were negative. Other thrombophilia markers like protein c, protein s, and antithrombin III levels were normal, but homocysteine was elevated (25 µmol/L). A peripheral blood smear revealed thrombocytosis with large platelets. The bone marrow was examined as recommended by the hematologist. It showed megakaryocytic hyperplasia with relatively normal erythroid and myeloid lineages [Figure 1b]. Molecular analysis revealed a JAK2 V617F mutation. She was diagnosed with ET according to WHO diagnostic criteria. Hydroxyurea was added to her treatment regimen. At the 4-month follow-up, she was asymptomatic, with a 3 lakh/μL platelet count and a 0.9 mg/dL serum creatinine level.
Discussion
Autopsy studies indicate a renal infarction rate of ∼14 cases per 1000 individuals (1.4%).1 In contrast, retrospective studies analyzing emergency department admissions report a significantly lower incidence, from 0.004% to 0.007%.2,3
Patients often present with flank or abdominal pain accompanied by fever, vomiting, or hematuria.2 Laboratory findings include leukocytosis, elevated CRP, elevated LDH, microscopic hematuria, and proteinuria.4 Renal dysfunction is more pronounced in patients with extensive renal infarction or bilateral kidney involvement. The diagnosis can be confirmed by contrast-enhanced CT, isotope perfusion scanning, or renal arteriography; however, ultrasonography lacks sufficient sensitivity.
ET is characterized by thrombocytosis (> 450,000/µL) and megakaryocytic hyperplasia of the bone marrow, with a JAK2, V617F, CALR, or MPL mutation (WHO diagnostic criteria). The JAK2 mutation causes constitutive activation of the Janus kinase-signal transducer and activator of transcription (JAK-STAT) signaling pathway, leading to dysregulated platelet production, promoting a hypercoagulable state.
In conclusion, ARI is a rare complication of ET with nonspecific presentations.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
References
- Acute renal infarction: A case series. Clin J Am Soc Nephrol. 2013;8:392-8.
- [CrossRef] [PubMed] [Google Scholar]
- Acute renal infarction Clinical characteristics of 17 patients. Medicine (Baltimore). 1999;78:386-94.
- [CrossRef] [PubMed] [Google Scholar]
- ED presentations of acute renal infarction. Am J Emerg Med. 2007;25:164-9.
- [CrossRef] [PubMed] [Google Scholar]
- Problems in the initial diagnosis of renal infarction. Intern Med. 1997;36:330-2.
- [CrossRef] [PubMed] [Google Scholar]







