Translate this page into:
Adrenal histoplasmosis: An unusual cause of adrenomegaly
Address for correspondence: Dr. Sameer Vyas, Department of Radiodiagnosis and Imaging, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh 160012, India. E-mail: sameer574@yahoo.co.in
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Histoplasmosis is a geographically restricted form of fungal infection. Adrenal involvement is seen in disseminated disease but sometimes it may be the only site of demonstrable disease. Early diagnosis and treatment may save the patient from catastrophic adrenal insufficiency. We present two patients showing bilateral adrenomegaly on ultrasonography and contrast-enhanced CT, and was diagnosed to have histoplasmosis on fine-needle aspiration cytology.
Keywords
Histoplasmosis
computed tomography
adrenal
Introduction
Histoplasmosis is an infective condition caused by a dimorphic, saprophytic fungus, Histoplasma capsulatum and is acquired by inhalation of its spores. Soil rich in bird and bat dropping is its natural habitat, and it exists as a mycelium in the atmosphere. The disease is endemic in the United States, Africa and Asia. Although most infections are asymptomatic, self-limiting acute pneumonitis and hilar lymphadenopathy may occur with inhalation of large aerosol.[1] It may occur in disseminated form in some patients with impaired host defence mechanism and frequently involves liver, spleen, lymph node, bone marrow and adrenal.[2–4] Adrenal involvement is usually sequelae of previous infection.[1] We encountered two patients presenting with nonspecific features of systemic disease and imaging revealed bilateral adrenomegaly. Transabdominal ultrasound guided fine-needle aspiration cytology (FNAC) of the adrenal showed histoplasmosis. A brief review of imaging of adrenal histoplasmosis is discussed along with the cases.
Case Reports
Case 1
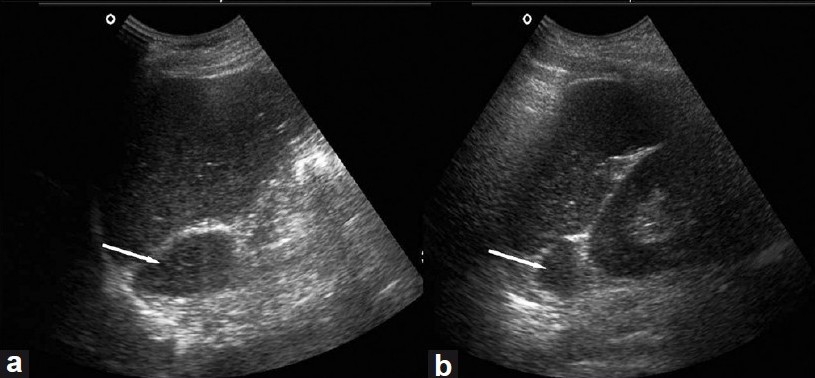
A 60-year-old diabetic male presented with low grade, intermittent fever, loss of weight and appetite for duration of 4 months. He had lost about 7 kgs in the past 6 months. He had been on oral hypoglycemics for noninsulin-dependent diabetes mellitus for 7 years. General examination of the patient was normal. Routine blood examination, urine examination, renal function test and chest X-ray were normal. Blood culture was sterile. The tests for malaria, tuberculosis and HIV were negative. Ultrasonography of the abdomen revealed hepatosplenomegaly without any focal lesion. Both adrenal gland were enlarged and hypoechoic [Figure 1]. Contrast-enhanced CT of the abdomen showed hepatosplenomegaly with enlarged, hypoattenuated bilateral adrenals showing peripheral rim enhancement and enhancing internal septations [Figure 2]. The adrenal endocrine profile was normal. Transabdominal ultrasound-guided FNAC [Figure 3] revealed numerous organism ranging in size from 2 to 4 μm in a necrotic background which were positive on Periodic Acid Schiff staining consistent with histoplasmosis. Fungal cultures from sample grew H. capsulatum. The patient was treated with itraconazole 200 mg twice daily and clinical improvement was seen within 4 weeks.

- Abdominal ultrasonography showing enlarged, hypoechoic right (a) and left (b) adrenal glands (arrows)
- Contrast-enhanced axial CT section of the upper abdomen showing enlarged and hypodense bilateral adrenals (white arrows) with peripheral rim enhancement and enhancing internal septations (black arrows)

- Fine-needle aspiration smear showing numerous degenerating Histoplasmosis capsulatum organisms in the necrotic background (Periodic Acid Schiff stain, ×1000)
Case 2
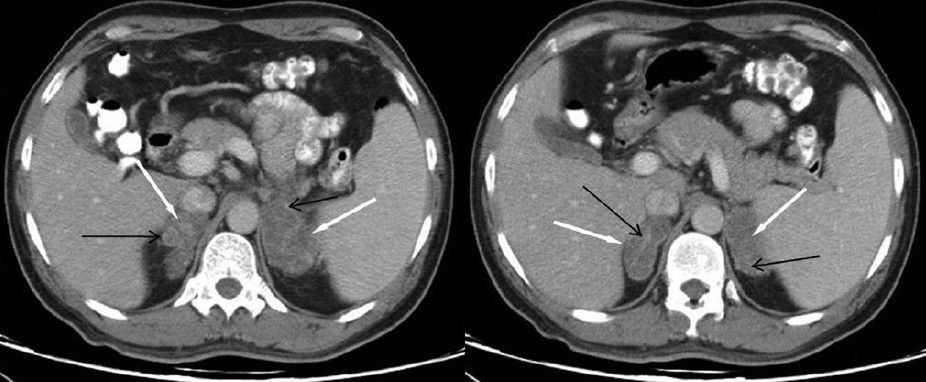
A 56-year old male presented with 6 month history of on and off fever, loss of weight and appetite, and hyperpigmentation all over the body. General physical examination was normal. Random cortisol level was 118.4 nmol/L (171-536 nmol/L) and post stimulation was 115 nmol/L (64-327 nmol/L). He had decreased calcium 8.3 gm/dl (8.6-10.2 gm/dl) and potassium 3.04 meq/L (3.5-5 meq/L) levels. Rest of the laboratory investigations including routine blood examination and blood sugar levels were normal. Ultrasonography of the abdomen revealed bilateral adrenomegaly [Figure 4] and contrast-enhanced CT showed peripherally enhancing hypodense bilateral adrenals with peripheral rim and septate enhancement [Figure 5]. The diagnosis of histoplasmosis was confirmed by transabdominal ultrasound guided FNAC. The FNAC showed a similar picture as in the case 1 confirming histoplasmosis which was also positive by fungal culture studies. The patient was treated with hydrocortisone, fludrocortisone and amphotericin B. The patient showed clinical improvement within one week.
- Ultrasonography of the abdomen revealing right (a) and left (b) adrenomegaly (arrows)

- Contrast-enhanced axial CT showing enlarged adrenals glands (white arrows) with rim enhancement (black arrows) of periphery and internal septations and central hypodensity
Discussion
Histoplasmosis is usually a self-limiting pulmonary infection, which is usually asymptomatic and can be associated with mild influenza like symptoms.[1] There are three major clinical presentations: pulmonary, progressive disseminated and primary cutaneous histoplasmosis. Progressive disseminated form of the disease is rare and occurs in the immunocompromised patients in the endemic areas.[14] Progressive disseminated disease may manifest as chronic disease in immunocompetent host or acute progressive disease in immunosuppressed hosts. In the patients with disseminated histoplasmosis, abdominal imaging usually reveals mild to moderate hepatomegaly with or without splenomegaly. Abdominal lymphadenopathy and focal hypodense lesions in the spleen are also been described.[5] The patients of adrenal histoplasmosis usually reveal bilateral adrenal masses of varied imaging features. On ultrasonography, they may show uniformly hypoechoic to heterogenous echopattern. Bilateral symmetrical adrenomegaly with preservation of the contour of the gland, central hypodensity with peripheral enhancement and presence of calcification has been described in CT.[6]
In both cases, abdominal imaging revealed hepatosplenomegaly with enlargement of bilateral adrenal glands. They were hypoattenuating with peripheral rim enhancement and enhancing internal septations. The differential diagnoses of bilateral adrenomegaly are metastasis, lymphoma, adrenal haemorrhage, sarcoidosis and infections which include histoplasmosis, tuberculosis, cryptococosis, coccidioidomycosis and blastomycosis.[67] But, central hypodensity and peripheral rim enhancement of the adrenals narrow down the differentials only to tuberculosis and histoplasmosis.[8] As the adrenal gland is frequently the only demonstrable site of active disease, adrenal FNAC can suggest the diagnosis which is further confirmed by culture, polymerase chain reaction, and urine antigen. It again can differentiate between tuberculosis and histoplasmosis.[9] H. capsulatum is an intracellular dimorphic fungus which is commonly seen within the cytoplasm of the macrophages and exhibit narrow based budding.[10–12] In fine-needle aspiration smears, these organism can also be seen extracellularly as the fragile cytoplasm of the macrophages may get disrupted at the time of making smears. In our two cases, there was necrosis in the smears which may have resulted in their presence extracellularly scattered throughout the necrotic material. These fungi can also be easily identified at the time of onsite adequacy evaluation in contrary to previous data which suggest that it is difficult to appreciate on routine cytological stains.[10–12] Rapid onsite cytopathological evaluation can suggest immediate diagnosis of the infection and hence the treatment can be started at the earliest.[11] Although this was not performed in our cases, the diagnosis was obtained the next day permitting prompt institution of treatment.
In the regions where endemic, possibility of histoplasmosis should always kept in a patient with enlarged, hypoattenuating bilateral adrenal glands with peripheral rim enhancement and enhancing internal septations. Image guided FNAC will demonstrate the disease and should be performed without delay as a great number of patients with adrenal histoplasmosis may develop life-threatening adrenal insufficiency if untreated.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Adrenal histoplasmosis: clinical presentation and imaging features in nine cases. Abdom Imaging. 2003;28:703-8.
- [Google Scholar]
- Addison's disease associated with histoplasmosis: report of four cases and review of literature. Am J Med. 1956;20:23-9.
- [Google Scholar]
- Disseminated histoplasmosis: clinical and pathological correlations. Medicine. 1980;59:1-33.
- [Google Scholar]
- Histoplasmosis in eastern India: the tip of the iceberg? Trans R Soc Trop Med Hyg. 1999;93:540-2.
- [Google Scholar]
- Disseminated histoplasmosis: Abdominal CT findings in 16 patients. AJR Am J Roentgenol. 1991;157:955-8.
- [Google Scholar]
- Adrenal histoplasmosis manifested as Addison's disease: unusual CT features with magnetic resonance imaging correlation. Clin Radiol. 2001;56:682-4.
- [Google Scholar]
- Disseminated histoplasmosis with bilateral adrenal enlargement: diagnosis by computed tomography directed needle biopsy. Tex Med. 1991;87:88-90.
- [Google Scholar]
- Spectrum of CT findings in non-malignant disease of the adrenal gland. Radiographics. 1998;18:393-412.
- [Google Scholar]
- Imaging spectrum in disseminated histoplasmosis: case report and brief review. Australas Radiol. 2005;49:175-8.
- [Google Scholar]
- Fine needle aspiration cytology in bilateral adrenal masses in a 58-year-old man. Acta Cytol. 2010;54:234-6.
- [Google Scholar]
- Bilateral adrenal gland enlargement secondary to histoplasmosis mimicking adrenal metastases: diagnosis with EUS-guided FNA. Diagn Cytopathol. 2010;38:357-9.
- [Google Scholar]







