Translate this page into:
An Adolescent with Tuberous Sclerosis and Hypocalcemia and a Renal Mass
Corresponding Author: Dr. Sidharth Kumar Sethi, Pediatric Nephrology, Kidney Institute, Medanta, The Medicity, Gurgaon - 122 001, Haryana, India. E-mail: sidsdoc@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sethi SK, Nataraj SA, Sankhyan N, Rana A, Nair A, Bansal SB. An Adolescent with Tuberous Sclerosis and Hypocalcemia and a Renal Mass. Indian J Nephrol 2024;34:94-5. doi: 10.4103/ijn.ijn_103_23
Dear Editor,
A 13-year-old girl, a known case of tuberous sclerosis, presented with complaints of paresthesias for the last one year and documented severe hypocalcemia (serum calcium 5.5 mg/dl). She had a history of multiple episodes of myoclonic seizures since the last 10 years, which was being managed with multiple anti-epileptic drugs, namely, valproic acid, lamotrigine, and lacosamide. Her surgical history revealed a left frontal craniotomy with near-total excision of subependymal giant cell astrocytoma (2016; at age seven). Her laboratory parameters are listed in Table 1, and MRI scans are shown in Figure 1a. Contrast-enhanced MRI axial imaging of kidneys showed a T1 hypointense and T2 hyperintense exophytic heterogeneously enhancing mass arising from medial cortex of the lower pole of the right kidney. Cystic lesions were seen as hypointense lesions in the remaining visualized parenchyma. Axial short tau inversion recovery (STIR) image showed a heterogeneous mass with multiple internal hyperintense areas that were suggestive of necrosis.
| Blood | Values at presentation | Reference range |
|---|---|---|
| Serum calcium | 5.5 mg/dl | 8.4–10.2 mg/dl |
| Serum parathyroid hormone | 906.3 pg/ml | 15.0–68.3 pg/ml |
| 25-hydroxyvitamin D | 16.6 ng/ml | 20–40 ng/ml |
| Serum phosphorus | 6.8 mg/dl | 2.5–4.5 mg/dl |
| Blood urea | 24 mg/dl | 15–36 mg/dl |
| Serum creatinine | 0.50 mg/dl | 0.7–1.2 mg/dl |
| Serum uric acid | 3.9 mg/dl | 2.5–6.2 mg/dl |
| Serum sodium | 141 mmol/L | 137–145 mmol/L |
| Serum potassium | 3.5 mmol/L | 3.5–5.1 mmol/L |
| Hemoglobin | 11.5 g/dl | 12–15 g/dl |
| Serum albumin | 2.6 g/dl | 3.5–5 g/dl |
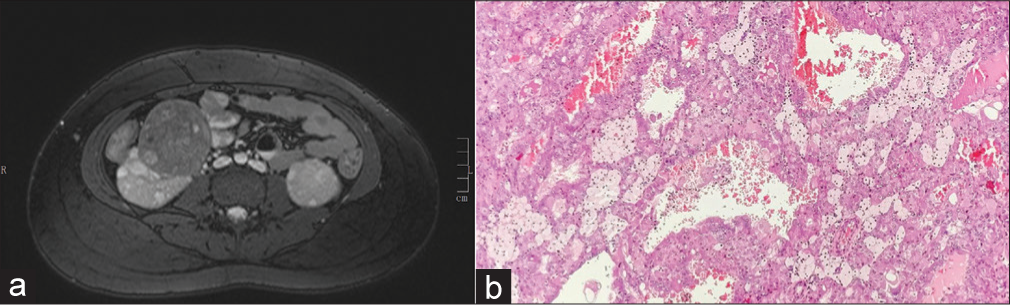
- (a) Contrast-enhanced MRI axial image of kidneys. There is a T1 hypointense and T2 hyperintense exophytic heterogeneously enhancing mass arising from the medial cortex of the lower pole of the right kidney. Cystic lesions are seen as hypointense lesions in the remaining visualized parenchyma. Axial short tau inversion recovery image shows a heterogeneous mass with multiple internal hyperintense areas suggestive of necrosis. (b) Papillary pattern composed of cells with abundant eosinophilic cytoplasm and hyperchromatic irregular nuclei with punctate nucleoli. Hob-nailing of cells is also seen focally.
The child received intravenous calcium gluconate and oral 1,25-vitamin D supplements to rapidly raise serum calcium. The child also received weekly 25-hydroxyvitamin D supplementation. The valproate dose was reduced based on the serum levels (126 mcg/ml; normal range 50–100 mcg/ml). The mass lesion revealed papillary renal cell carcinoma [Figure 1b]. Right open partial nephrectomy was performed. The child’s serum calcium and the need for oral calcium and active vitamin D supplement reduced over the next two weeks. Currently, at a follow-up of six months, the child is doing well, having a normal serum creatinine of 0.6 mg/dl, and is on RDA supplement of oral calcium.
Tuberous sclerosis (TSC) is caused by germline loss-of-function mutations of either the TSC1 or TSC2 gene. Approximately 60% of germline TSC gene mutations are de novo and 40% are inherited. TSC is a multisystemic neurocutaneous disorder affecting the brain (subependymal giant cell astrocytomas, cerebral cortical tubers), heart (rhabdomyomas), kidney (angiomyolipomas, cysts, renal cell carcinomas), lung (lymphangioleiomyomatosis [LAM]), and skin (angiofibromas). TSC patients can also develop seizures, autism, and cognitive disability.1
Hypocalcemia is a serious medical condition in patients with TSC who develop seizures and are on anti-epileptic drugs, namely, valproic acid, which increases degradation of 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D3 by upregulation of 24-hydroxylase CYP24A causing inhibitory effects on calcium absorption and end-organ resistance and inhibition of calcitonin secretion.2
The renal manifestations of TSC include angiomyolipomas, epithelial cysts which can resemble polycystic kidney disease, and renal cell carcinoma (RCC). Angiomyolipomas are the most frequent lesion (75%) followed by simple renal cysts (17%).1,2 Around 4% of patients develop RCC.2–5 Careful morphological studies of such RCC have permitted their subdivision into groups: clear cell (most common); others being papillary, chromophobe and unclassified RCC, and benign renal cell oncocytoma.3,4 Tumors in TSC, including angiomyolipomas and RCCs, develop after somatic “second hit” inactivation of the remaining wild-type allele of TSC1 or TSC2.5
RCC, though rare, should be kept in mind as a differential diagnosis when encountering a TSC patient with renal mass, even in children. Regular radiological surveillance may help in early detection and timely intervention to decrease renal morbidity and mortality.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Renal Tumors in Tuberous sclerosis complex. Pediatr Nephrol. 2021;36:1427-38.
- [CrossRef] [PubMed] [Google Scholar]
- Severe hypocalcemia in a patient with tuberous sclerosis complex. Electrolyte Blood Press. 2019;17:21-4.
- [CrossRef] [PubMed] [Google Scholar]
- Renal cell carcinoma in tuberous sclerosis complex. Am J Surg Pathol. 2014;38:895-909.
- [CrossRef] [PubMed] [Google Scholar]
- Tuberous sclerosis-associated renal cell carcinoma: A clinicopathologic study of 57 separate carcinomas in 18 patients. Am J Surg Pathol. 2014;38:1457-67.
- [CrossRef] [PubMed] [Google Scholar]
- Renal cell carcinoma in tuberous sclerosis complex. Genes (Basel). 2021;12:1585.
- [CrossRef] [PubMed] [Google Scholar]






