Translate this page into:
An unusual cause of acute deterioration in a chronic kidney disease patient
Address for correspondence: Dr. Srilatha Vadlamudi, Department of Nephrology, NRI Medical College, Chinakakani, Guntur District, Andhra Pradesh, India.
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
A 43 year old non diabetic, non hypertensive female presented with fever, loin pains, shortness of breath and vomiting of 1 week duration. She had undergone total hysterectomy 15 years back. Evaluation revealed serum creatinine 9 mg/dl, serum calcium 8.6 mg/dl, serum albumin 3.0 gm/dl, Haemoglobin - 7.1 gm/dl, neutrophilic leukocytosis, antinuclear antibody (ANA) positive. Urinalysis revealed pyuria, microscopic hematuria and culture grew Escherichia coli. Patient underwent renal biopsy which revealed neutrophilic infiltration in interstitium, no evidence of chronicity, immunofluoresence studies were negative, diagnosed as acute pyelonephritis. Patient was treated accordingly and discharged with a serum creatinine of 2.3 mg/dl with a discharge advice of antibiotics, iron, calcium and vitamin D supplements.
Follow up after 1 month revealed stable renal function but persistent anaemia. Evaluation revealed actively bleeding haemorrhoids was managed by hemorrhoidectomy. During follow up, patient was persistently anaemic. Iron studies were normal and peripheral smear revealed normocytic normochromic anaemia. She was started on erythropoietin.
Five months after initial presentation, patient presented with acute deterioration in renal function. Investigations revealed serum creatinine 7.6 mg/dl, serum calcium 11 mg/dl, hemoglobin 6.2 gm/dl, total count 8300, urine microscopy normal and culture was sterile. Computed tomography (CT) abdomen showed normal kidneys and fractures of D10, D12 vertebra.
Persistent hypercalcemia despite discontinuation of vitamin D analogues, persistent anaemia inspite of iron and erythropoietin therapy, vertebral fractures previously attributed to osteoporosis raised the suspicion for multiple myeloma. Serum protein electrophoresis revealed monoclonal band, bone marrow aspiration showed 30% plasma cell load. Repeat renal biopsy revealed myeloma cast nephropathy [Figure 1]. Immunofluoresence revealed casts positive for lambda chain.
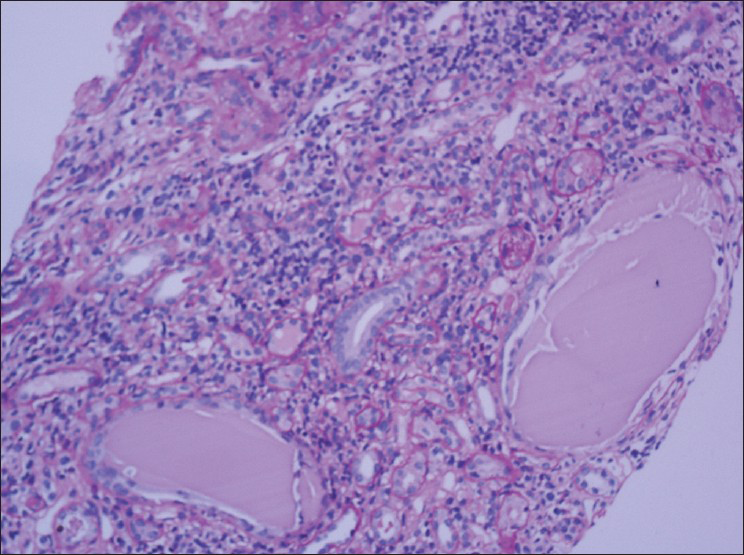
- PAS stain showing fractured casts in the tubules surrounded by giant cell reaction and interstitial inflammation
Retrospectively, this patient might have myeloma prior to the initial presentation which predisposed to pyelonephritis and might have contributed to incomplete recovery. Given the initial biopsy report as acute pyelonephritis and persistent renal insufficiency for three months, a diagnosis of Chronic Kidney Disease (CKD) was made. This led to diagnostic dilemma when patient presented with acute deterioration later in the course, as myeloma is elusive to diagnosis in CKD.
Bone pains, the most common symptom effecting myeloma patients (70%)[1] may be attributed to renal osteodystrophy or osteoporosis. Short of bone biopsy accurate diagnosis of bone disease in a CKD[2] patient is not possible. Anaemia which affects 80%[1] of myeloma patients may be attributed to anaemia of CKD. Anaemia is normocytic normochromic in both conditions and is not useful until erythropoietin hyporesponsiveness[3] is documented, there by delaying diagnosis. Hypercalcemia, the most common metabolic complication of myeloma effecting one third of patients[4] may be attributed to calcium, vitamin D supplements which many of CKD patients will be using as well as hyperparathyroidism.
High index of suspicion is required to identify plasma cell dyscrasia in a patient with chronic kidney disease. As the diagnosis dramatically alters the patient's subsequent management and clinical outcome, multiple myeloma also should be considered in differential diagnosis of cause for acute deterioration without obvious evident cause in chronic kidney disease patient.
References
- Plasma Cell Disorders; Harrison's Principles of Internal Medicine. (17th ed). India: Mc Graw Hill; 2008. p. :701-5.
- [Google Scholar]
- Metabolic bone disease in chronic kidney disease. J Am Soc Nephrol. 2007;18:875-85.
- [Google Scholar]






