Translate this page into:
Anti-Thymocyte Globulin Induced Acute Lung Injury in a Case of Renal Allograft Recipient
Address for correspondence: Dr. Nimish Gupta, Consultant Nephrology, Metro Heart Institute with Multispeciality, Sector 16a, Faridabad, Haryana, India. E-mail: nimish392005@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor,
Rabbit anti-thymocyte globulin (rATG) is a T-cell-depleting immunosuppressive agent that is widely used in both living and cadaveric renal transplantation. Its dosage and usage vary among different transplant centers.[1] rATG may be associated with a number of adverse effects such as increased posttransplant infections and possibly malignancy.[2] Various immunological reactions have been reported in the literature with rATG use such as serum sickness syndrome,[3] non-cardiogenic pulmonary edema,[3] refractory hypotension,[3] and fatal anaphylaxis. We report here a case of acute lung injury (ALI) with cytokine syndrome due to rATG with heightened immune reaction with each subsequent dose.
A 46-year-old woman was admitted electively for living unrelated kidney transplantation with basic disease being diabetic nephropathy. She was planned for a living unrelated renal transplant with donor being her brother-in-law. The donor and recipient were 0/1/2 A/B/DR HLA matched. CDC and flow crossmatch were negative including SARS COVID 19 RT PCR. She was asymptomatic on the day of transplant. Induction Immunosuppression was planned with intravenous corticosteroids and rATG, to be given at a dose of 3.5 mg/kg in three divided doses.
On the morning of surgery before being shifted to the operation theatre, she received rATG 50 mg in 250 mL 0.9% normal saline with premedication of pheniramine and acetaminophen. Thirty minutes after the infusion, she developed sudden shortness of breath. Physical examination revealed bilateral chest crepitations mainly in the basal region. Lab investigations were sent and revealed serum procalcitonin was 0.3 ng/ml (normal value <0.15 ng/mL), hemoglobulin was 10.1 gm/dL, total leucocyte count of 9800 cells/mm3 and platelet counts of 1,91,000//mm3. A high-resolution CT (HRCT) scan of the chest was suggestive of bilateral lung infiltrates (right more then left) in basal regions [Figures 1 and 2]. Blood cultures revealed no growth. It was decided to postpone the surgery. She was started on empiric antibiotics for a presumed diagnosis of pneumonia and sent home. Serial chest X-rays showed persistent right lower lobe infiltrates though with decreasing intensity.
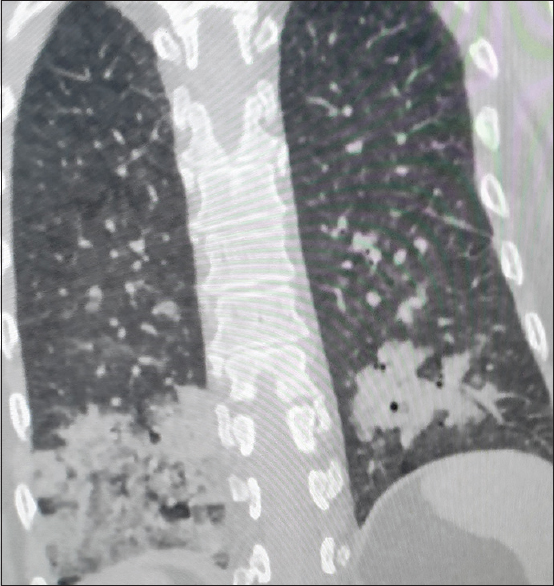
- High-resolution CT scan of chest showing bilateral lung infiltrates, right more then left
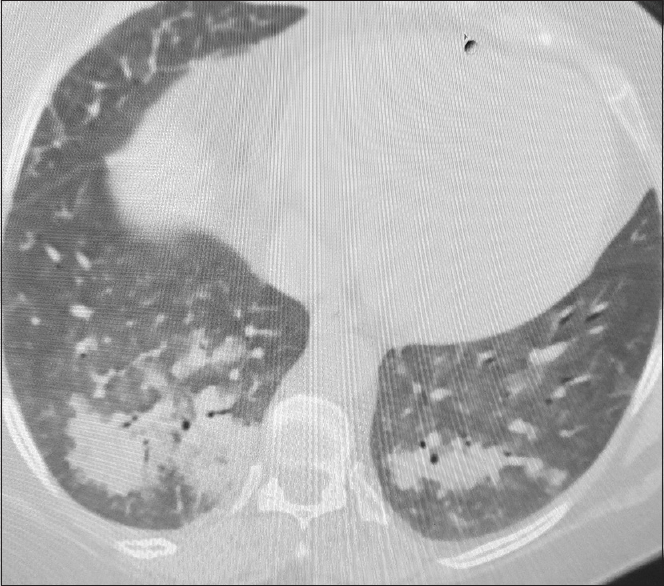
- High-resolution CT scan of chest showing bilateral lung infiltrates, right more then left
After 24 days of the initial event, she was admitted again for renal transplant surgery. Repeat HRCT scan of the chest showed resolution of previous lung infiltrates [Figures 3 and 4]. Repeat CDC and flow crossmatch were negative. She received 50 mg rATG in 250 mL of 0.9% normal saline on the morning of surgery. Kidney transplant surgery was uneventful. Preoperative hemoglobin was 10.2 gm/dL and estimated blood loss intraoperatively was around 1 L. In the immediate posttransplant period, she had good urine output of around 800 mL in the first hour post-surgery. After 60 minutes she had sudden fall in blood pressure to 60/40 mm Hg. A stat hemoglobin value was 4.3 gm/dL. Rapid infusion of crystalloid intravenous fluids and inotrope nor adrenaline was started, and the patient was shifted to operation theater for re-exploration for a suspected bleed. However, quick ultrasound doppler showed good flow in both artery and vein with no fluid collection around the transplanted kidney. The surgical drain remained dry during this interval. She was given two packed red blood cell transfusions urgently. Her urine output remained 600–800 mL/h throughout. Chest X-ray was performed and showed no infiltrates. She gradually improved and blood pressure stabilized to 120/80 mm Hg. The cause of this event remained elusive.
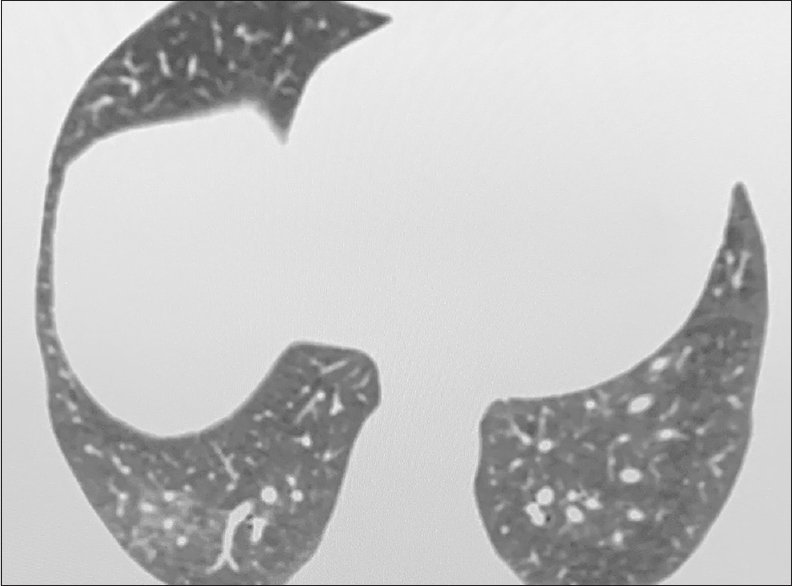
- After 24 days of primary event repeat CT shows improvement in lung infiltrates

- After 24 days of primary event repeat CT shows improvement in lung infiltrates
Postoperative days 1 and 2 remain uneventful with no history of fever, cough, or any breathlessness. There was good urine output with improving serum creatinine levels. Her vitals remain stable and oxygen saturation was 99% on room air. On postoperative day 3, she again received 50 mg of IV ATG over 3 h with pre-medications. Five hours post-infusion, she had a sudden cardiac arrest and brief CPR of 2 mins was done. Injection epinephrine (1:10000) i.v. was given and the return of spontaneous circulation achieved quickly in less than 2 min. The patient was subsequently intubated and put on ventilatory support. Chest X-ray was done and showed bilateral lower zone infiltrates [Figure 5]. The patient was put on inotropic support and dose was titrated as per blood pressure. For suspected acute coronary event, a coronary angiography was done which revealed normal coronary arteries. IL-6 levels were sent to corroborate with possibility of cytokine release syndrome and they were high: 15.26 pg/mL (normal range <7.00 pg/mL). Holter monitoring revealed normal sinus rhythm.
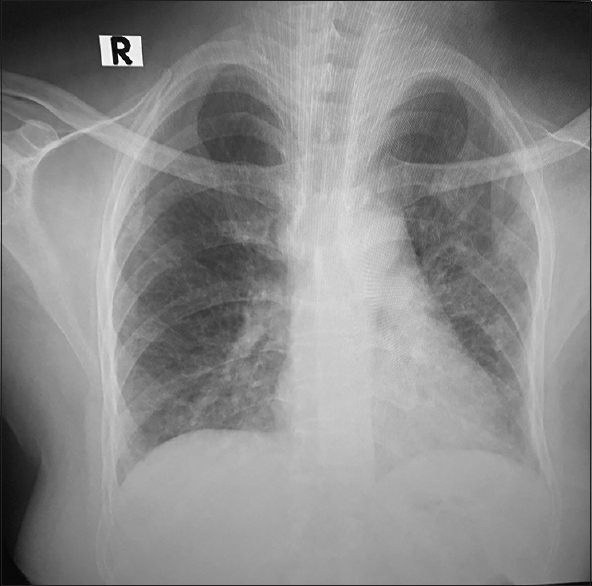
- Chest X-ray showing lower lung infiltrates after repeat ATG administration
On postoperative day 5, she was extubated with no inotropic requirement. All these previous episodes of pulmonary edema, hypotension with escalating severity were likely due to rATG hypersensitivity. No further infusion of rATG was given. Pulmonary edema was managed with injection torsemide on titrated doses. She was discharged after 6 days with a nadir serum creatinine of 0.8 mg/dL. During subsequent follow-up, her allograft remained stable. Her serum creatinine continues to be 0.9 mg/dL at 3 months post-transplantation.
Discussion
rATG is made by immunizing rabbits who are devoid of any pathogens with a cell suspension of human thymocytes.[4] rATG is widely used as an induction agent in renal transplantation especially in high-risk cases.[3] In the present case, there was heightened severity of symptoms with each subsequent dose of rATG. Also, each time there was recovery by conservative measures only which further strengthen the association of sudden onset pulmonary infiltrates with rATG. Isolated ALI due to rATG is sparsely reported in literature. There are few case reports of ALI with rATG in cases other than renal transplantation.[5] rATG can increase pulmonary capillary endothelium permeability by increasing TNF-α and interleukin levels similar to sepsis.[5] rATG induced acute lung injury without other signs of hypersensitivity is a rare finding. More studies are needed in future to elucidate the pathogenesis and thus to prevent such complications if possible.
Declaration of patient consent
Informed and written consent was obtained from all individual participants included in the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Rabbit anti-thymocyte globulin induction in renal transplantation: Review of the literature. Transpl Res Risk Manag. 2014;6:9-21.
- [Google Scholar]
- Induction by anti-thymocyte globulins in kidney transplantation: A review of the literature and current usage. J Nephropathol. 2015;4:110-15.
- [Google Scholar]
- Anti-thymocyte globulins in kidney transplantation: Focus on current indications and long-term immunological side effects. Nephrol Dial Transplant. 2017;32:1601-8.
- [Google Scholar]
- Thymoglobulin and its use in renal transplantation: A review. Am J Nephrol. 2013;37:586-601.
- [Google Scholar]
- Acute lung injury during antithymocyte globulin therapy for aplastic anemia. Can Respir J. 2009;16:e3-5.
- [Google Scholar]






