Translate this page into:
Holistic health assessment tool for patients on maintenance hemodialysis
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The recent emphasis on assessment of the psychological status, availability of newer and better methods of interpreting the anthropometric measurements of renal patients on dialysis therapy prompted the authors to develop the “Holistic Health Assessment Tool for dialysis patients (HHAT-D).” A total of 30 subjects (25–65 years), enrolled from dialysis centers in Mumbai were administered the HHAT-D tool to assess anthropometric, biochemical, functional, and psychological status (knowledge, needs, that coping strategies) along with dietary intake. The results showed that majority of the patients (73.3%) were mild to moderately malnourished. A highly significant negative correlation of anthropometric measurements (BMI, lean body mass, mid arm circumference, arm muscle area, bicep skin fold thickness, % usual body weight, and % standard body weight) with the HHAT-D scores (P<0.01) confirmed the validity of the tool in assessing the degree of malnutrition. The poor health status of the patients was further confirmed by the average (40%) to poor (36.6%) flexibility status and poor dietary nutrient intake. Moderate (36.6%) to high (60%) coping effectiveness was recorded in the patients as assessed using the “coping effectiveness inventory.” A high degree of interitem correlation (Cronbach's coefficient alpha-test value 0.836) also proved the reliability of the HHAT-D tool. Thus, the HHAT-D was found to be a specific and reliable tool for assessment of holistic health status of patients on maintenance hemodialysis to improve quality of life and facilitate faster recovery.
Keywords
Dialysis malnutrition score
dialysis
holistic health assessment tool
malnutrition
Introduction
Protein-energy malnutrition is prevalent in 16–54% of patients undergoing maintenance hemodialysis (MHD).[1–3] Subjective global assessment (SGA) is a tool that integrates various tests to derive a combined overall score of malnutrition[4] that has been used to determine the nutritional status of patients[56] and other populations at risk of protein energy malnutrition.[7] However, due to its subjective nature, Kalanter-Zadeh et al.[8] modified it into a fully quantitative scoring system called the dialysis malnutrition score (DMS) that is more reproducible and accurate.[9] Lowrie et al.[10] noted that increased psychological stress and related depression in 85% of dialysis patients was regarded as a major predictor of patient outcome and also influenced long-term compliance with diet and medication. Regular assessment of physical functioning and encouragement of increased physical activity are still given minimal attention within the nephrology community.[11] Thus, a need was felt by the authors to develop a new tool using additional subjective and objective tests to assess the holistic health of renal patients on MHD.
Materials and Methods
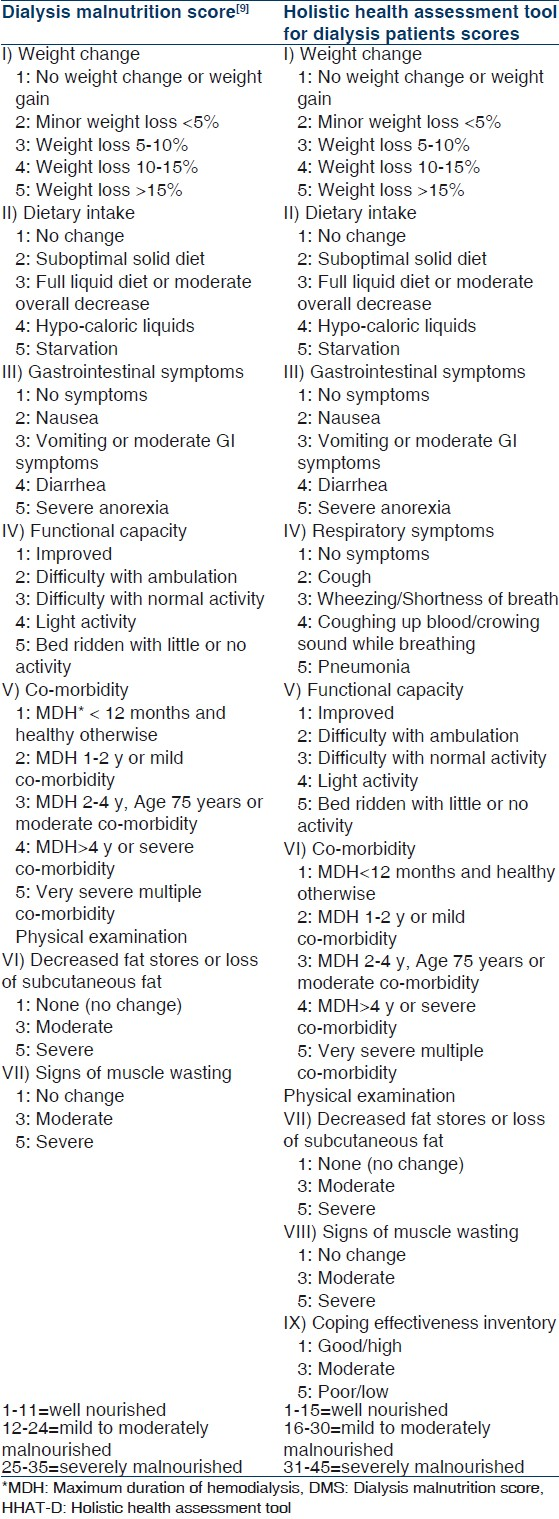
Thirty subjects (13 males and 17 females) in the age group of 25–65 years and maintained on hemodialysis for ≥3 months were selected using purposive sampling technique after obtaining written informed consent. Patients in a disoriented state or with severe multiple complications were excluded from the study. The study protocol was approved by the Ethics Committee for Research in Human Subjects (ECRHS) of Seth G.S. Medical College and K.E.M. Hospital, Mumbai. The subjects were administered the Holistic Health Assessment Tool (HHAT-D) as well as the DMS (modified SGA tool). The details of the scoring system for DMS and HHAT-D tools are given in Table 1.
Anthropometry and body composition
Various anthropometric indicators of body composition including BMI, percent usual body weight (%UBW) and percent standard body weight (%SBW), skin fold thickness [triceps (TSF), biceps (BSF), subscapular (SCSF), suprailiac (SISF)], body fat mass (BFM), lean body mass (LBM), and limb muscle measurements [midarm circumference (MAC) and arm muscle area (AMA)] were recorded.
Biochemical tests: Total protein, serum albumin, blood urea nitrogen, and hemoglobin levels were noted from patients’ records.
Clinical assessment: In addition to GI symptoms, the presence and severity of respiratory symptoms were also recorded since impaired pulmonary function is associated with malnutrition and inflammation and predicts mortality in CKD patients.[12]
Dietary assessment: Dietary nutrient consumption and eating patterns of the patients were recorded using a 24 h diet recall.
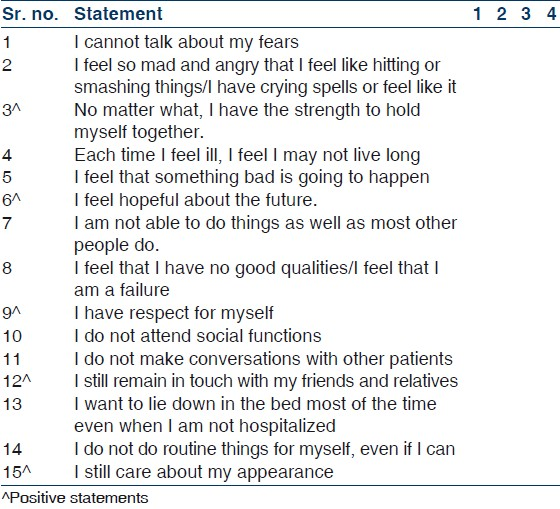
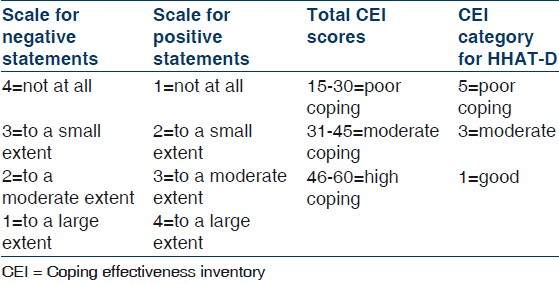
Psychological assessment: A detailed questionnaire was used to assess knowledge about the disease, causes and dietary restrictions and needs (occupational, physical, social, emotional, spiritual, and financial) of the patients. The importance of learning to cope with stress in preventing severe malnutrition was evaluated using coping effectiveness inventory (CEI). This tool originally developed by Almeida and Agarwal[13] was modified to include 15 statements dwelling on the five themes such as containment of feelings, generation of hope, self esteem, relationships, and well being with score ranging from 15 (poor) to 60 (high). Three statements related to each of the five themes were included containing two negative and one positive statement [Table 2] that were graded according to the scale [Table 3].
Assessment of functional capacity: The subjects were asked to perform a simple test for flexibility i.e. “sit and reach test”[14] to understand readiness for initiating exercise program among them.
In addition to the seven parameters of DMS (Asgarani et al. 2004), patients were scored on two additional parameters including respiratory symptoms and coping effectiveness inventory. Each component had a score from 1 (normal) to 5 (very severe) thereby obtaining scores ranging from 9 (well nourished/normal) to 45 (severely malnourished) [Table 3]. Patients with the lower score were considered to have near normal nutritional status while those with higher scores had greater risk of complications.
Statistical analysis
Data were analyzed using descriptive statistics including frequencies, percentage, mean, S.D. and advanced statistics such as Pearson's correlation coefficient test to assess the strength of association between the variables using SPSS (version 12.0). Reliability of the HHAT-D was tested using Cronbach's coefficient alpha test.
Results
HHAT-D was found to be as effective as the DMS in determining the extent of malnutrition among the patients as there was no major difference in the percentage of patients identified at different levels of malnutrition [Figure 1]. According to the %UBW, majority (46.6%) of the subjects were found to have mild to moderate malnutrition whereas the %SBW was within the normal range. The HHAT-D scores showed a highly significant negative correlation with anthropometric parameters such as BMI, LBM, MAC, AMA, BSF, %UBW, and %SBW (P<0.01) [Table 4]. Also, loss of subcutaneous fat showed a significant negative correlation with the body fat mass (P<0.05) calculated from the skin fold measurements at four sites. Similarly subjective evaluation of muscle wasting correlated significantly and negatively with the lean body mass measurements (P<0.05).
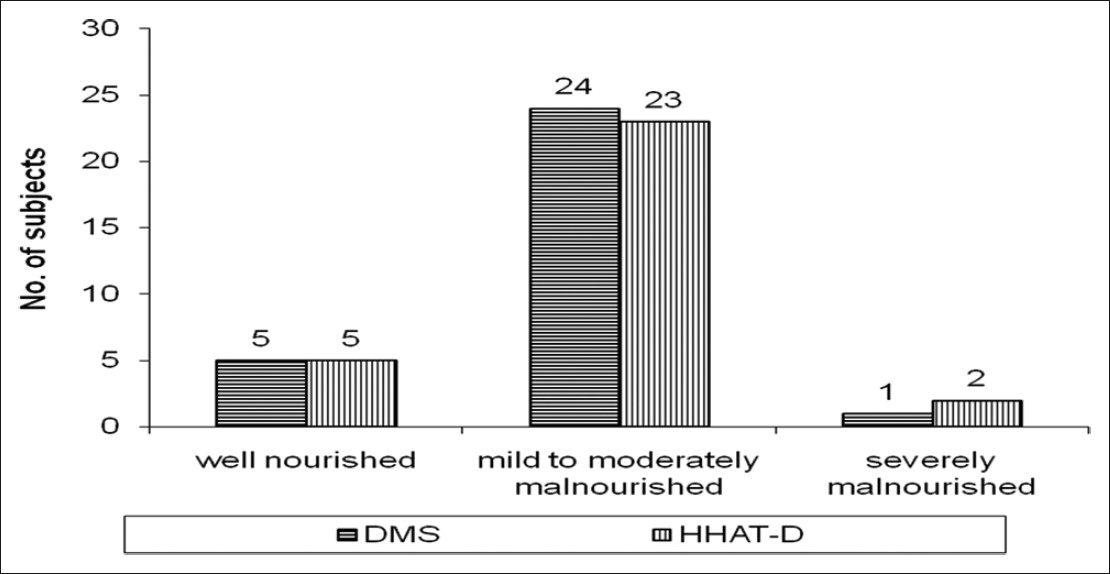
- Degree of malnutrition assessed using the dialysis malnutrition score (DMS) and holistic health assessment tool for dialysis patients (HHAT-D)
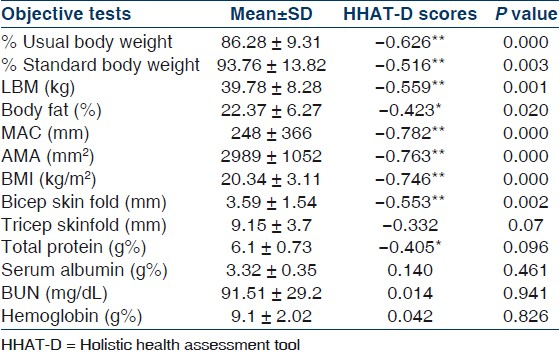
No significant correlation was found between the HHAT-D scores and biochemical parameters, except for total protein that showed a significant negative correlation (P<0.05) indicating that low serum protein was associated with greater malnutrition. The mean serum albumin level (3.32 g %) was toward the lower range of the normal value 3.5–5.0 g% [Table 4]. The BUN values were found to be higher than normal while haemoglobin levels were found to be much lower than normal range in the patients [Table 4]. Cough (26.6%) and shortness of breath (46.6%) were the most commonly reported respiratory symptoms in the subjects.
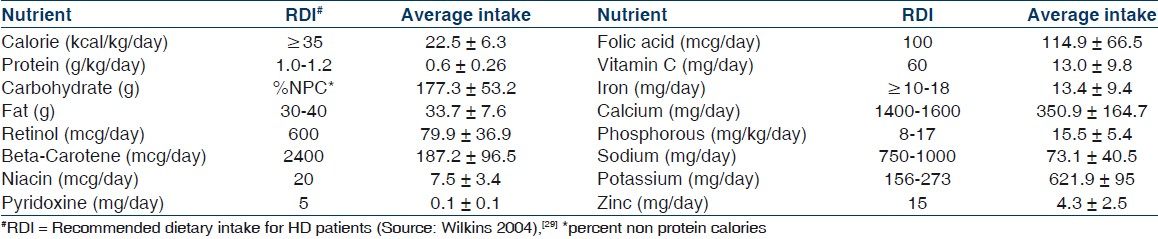
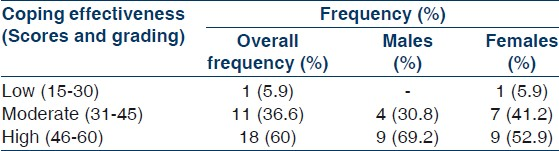
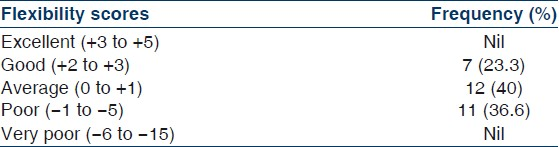
Nutrient intake showed a negative but non significant correlation with HHAT-D scores indicating that poor food intake in terms of both macronutrients as well as micronutrients lead to the high degree of malnutrition among the patients. However, potassium was consumed in much larger quantities through the diet than recommended [Table 5]. Psychological assessment revealed moderate (36.6%) to high (60%) coping effectiveness in the patients [Table 6] which showed significant negative correlation with HHAT-D scores (r=–0.418, P<0.05) indicating that poor ability to cope with stress was associated with severe malnutrition and/or vice versa. Simple Flexibility test (sit and reach) to assess functional capacity showed average (40%) to poor (36.6%) flexibility level [Table 7] and a positive correlation with the HHAT-D scores, though non-significant. The Cronbach's alpha score for HHAT-D (0.836) was found to be similar to that of DMS (0.832).
Discussion
The institution of appropriate medical and nutritional care for the patients could be delayed due to underestimation of the degree of malnutrition, giving rise to increased health risks.
The HHAT-D included measurement of the %UBW and %SBW of the patients as per guidelines of the National Kidney Foundation Kidney Disease Outcomes Quality Initiative[15] to help predict the level of malnutrition. The negative correlation between HHAT-D scores and most of the anthropometric parameters indicated compromised nutritional status among the patients [Table 4]. Similar observations have been made by Asgarani et al.[9] using the DMS. The determination of LBM and BFM values included in HHAT-D provided for more critical assessment of body composition and can serve as a reference when long term nutritional follow-up is desirable.[16]
Hypoalbuminemia, as observed in most subjects [Table 4], is highly predictive of future mortality risk when present during the course of MHD.[1718] Higher than normal BUN values and very low hemoglobin levels as noted in the HHAT-D helped to pay attention towards metabolic disturbances requiring immediate medical supervision. The NKF KDOQI workgroup have emphasized the importance of treating patients to hemoglobin of greater than 11 g%[19] and hence essential with analyze and monitor.
The frequency and duration of gastrointestinal and respiratory symptoms have an impact on the nutritional status. Poor respiratory function which is reflective of impact of malnutrition and inflammation on respiratory muscle performance influences clinical outcome[12] but was not part of the modified SGA tool and hence considered in the HHAT-D. In subjects who developed nausea, vomiting, cough, shortness of breath and pneumonia, poor respiratory functions persisted for >2 weeks further causing sleep disturbances and compromising physical activity functioning.
Anorexia and restriction of certain foods that are rich in water-soluble vitamins owing to their high potassium content[20] lead to poor food intake and thereby low nutrient intake among renal patients. In the present study also, the average dietary consumption of total calorie, protein, fiber and several micronutrients was found to be much lower than the recommended level while fat intake of the subjects was adequate [Table 5]. Anemia is a very common problem among CKD patients caused by the deficiency of erythropoietin and/or iron.[21] Ensuring sufficient iron intake through diet could be considered in the management of anemia, though intravenous infusion of iron is unavoidable in certain cases. Patients are also advised to consume micronutrient supplements to avoid deficiency. Hypercalcemia in hemodialysis patients resulting from excess calcium and phosphorous intake increases risk of calcification of soft tissues.[22] Hence, the calcium needs are individualized based on careful evaluation of serum calcium and phosphorous levels, use of supplements, phosphate binders, dialysate calcium concentration and sufficiency of dietary intake. Individualized attention to the calcium and iron needs of the patients is necessary due to the changes in mineral metabolism in order to plan suitable management strategies.
Taskapan et al.[23] opined that evaluation of psychological status should be part of the care provided to hemodialysis patients. This contention was supported by other experts who observed chronic depression among dialysis patients and other psychiatric disorders having an impact on overall quality of life.[24] Knowledge about the clinical condition can serve as a key element to overcome stress since patients gain a sense of control over their experiences and environment and helps reduce feelings of vulnerability,[25] whereas lack of awareness can lead to patients harboring wrong notions and faulty beliefs further hindering recovery. Current study recorded poor knowledge base and inadequate information about the disease condition and associated dietary changes among the patients. Interestingly, women were less vocal about their needs as compared to men and both the sexes showed high social and emotional needs which would help them tide over the stressful state more easily. The CEI tool has been found to be reliable (Cronbach's alpha 0.80) and valid for assessment of coping strategies among Indian population suffering from end stage renal disease.[13] In the present study, the total CEI scores revealed that better coping was associated with lower degree of malnutrition for both the sexes [Table 6] thereby highlighting the need to pay attention to this vital aspect of nutritional status. Ersoy-Kart and Guldu[26] reported lower coping scores and greater vulnerability to stress among 55 patients receiving HD in Turkey.
The reduced physical capacity and activity level in hemodialysis patients as assessed through the flexibility test [Table 7] may be responsible for the increased incidence of depression observed among them which reduces the patients’ ability to perform familiar pleasant activities.[27]
Steiber et al.[28] opined that establishing the validity and reliability of each version of nutritional assessment tool in different patient populations is very essential to facilitate correct application of the same by clinicians and researchers. The Cronbach's coefficient alpha-test showed a high degree of inter-item correlation indicating a high internal consistency of each item in the tool. The reliability scores signify that the items in the tool (anthropometry, body composition, etc) truly measured the construct (assessment of health status) they were aimed to measure. Also, the selected objective tests showed significant negative correlation with the HHAT-D scores (based on subjective evaluation) thereby enhancing the validity of the tool.
Thus, the Holistic Health Assessment Tool for Dialysis patients (HHAT-D) can be considered as a valid and reliable tool which throws light on the various crucial indicators of malnutrition associated with kidney dysfunction and hence can be used to improve the overall quality of life of these patients. However, there is a need to further assess the inter and intra-observer reliability as well as validity of the HHAT-D tool by administering it on larger subject population with the help of more comparative and longitudinal studies.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Cross-sectional comparison of malnutrition in continuous ambulatory peritoneal dialysis and hemodialysis patients. Am J Kidney Dis. 1995;26:475-86.
- [Google Scholar]
- The hemodialysis (HEMO) pilot study: Nutrition program and participant characteristics at baseline. J Ren Nutr. 1998;8:11-20.
- [Google Scholar]
- Nutritional status of patients on hemodialysis and peritoneal dialysis. Clin Nephrol. 1988;29:75-8.
- [Google Scholar]
- Evaluating the accuracy of nutritional assessment techniques applied to hospitalized patients: Methodology and comparisons. JPEN J Parenter Enteral Nutr. 1984;8:153-9.
- [Google Scholar]
- Nutritional assessment: A comparison of clinical judgement and objective measurements. New Engl J Med. 1982;306:969-72.
- [Google Scholar]
- Prognostic significance of Subjective Global Assessment (SGA) in advanced colorectal cancer. Eur J Clin Nutr. 2005;59:35-40.
- [Google Scholar]
- Application of subjective global as a screening tool for malnutrition in pediatric surgical patients. J Med Assoc Thai. 2004;87:939-46.
- [Google Scholar]
- A modified quantitative subjective global assessment of nutrition for dialysis patients. Nephrol Dial Transplant. 1999;14:1732-8.
- [Google Scholar]
- Correlation between modified SGA with anthropometric measurements and laboratory parameters. Acta Med Iran. 2004;42:331-7.
- [Google Scholar]
- The association of SF-36 quality of life scales with patient mortality. Germany: CQI Memorandum, Fresenius Medical Care; 1997.
- Physical functioning in CKD; it's time to GET MOVING! Dialysis Times News and Views from Renal Research Institute. . 2010;17(2):2.
- [Google Scholar]
- Malnutrition and inflammation are associated with impaired pulmonary function in patients with chronic kidney disease. Nephrol Dial Transplant. 2004;19:1823-8.
- [Google Scholar]
- Stressors, Coping strategies and extent of coping in ESRD patients and their relatives. Indian J Nephrol. 2000;10:105.
- [Google Scholar]
- National Kidney Foundation Kidney Disease Outcomes Quality Initiative NKF: KDOQI clinical practice guidelines for nutrition in chronic renal failure. Appendix VII. Methods for Performing Anthropometry and Calculating Body Measurements and Reference Tables Am J Kidney Dis. 2000;35:s76-s77.
- [Google Scholar]
- Body fat mass and lean mass as predictors of survival in hemodialysis patients. Kidney Int. 2006;70:549-56.
- [Google Scholar]
- Predictors of mortality in hemodialysis patients. J Am Soc Nephrol. 1993;3:1613-22.
- [Google Scholar]
- The target hemoglobin in patients with chronic kidney disease. Nephrol News Issues. 2006;20:29-30.
- [Google Scholar]
- Food and Nutrition Board (FNB) National Research Council. In: Recommended Dietary allowances (10th ed). Washington DC: National Academy Press; 1989. p. :114-20.
- [Google Scholar]
- National Kidney Foundation K/DOQI Clinical Practice Guidelines for Bone Metabolism and Disease in CKD. Am J Kidney Dis. 2003;42(suppl 3):S1-201.
- [Google Scholar]
- Psychiatric disorders and large interdialytic weight gain in patients on chronic haemodialysis. Nephrology (Carlton). 2005;10:15-20.
- [Google Scholar]
- Multiple measurements of depression predict mortality in a longitudinal study of chronic hemodialysis patients. Kidney Int. 2000;57:2093-8.
- [Google Scholar]
- Coping strategies and stressors in patients with hemodialysis. Psychosom Med. 2007;69:182-90.
- [Google Scholar]
- Vulnerability to stress, perceived social support, and coping styles among chronic hemodialysis patients. Dial Transplant. 2005;34:662-71.
- [Google Scholar]
- The relationship between depression and aerobic capacity in hemodialysis patients. Psychosom Med. 1986;48:143-7.
- [Google Scholar]
- Subjective global assessment in chronic kidney disease: A review. J Ren Nutr. 2004;14:191-200.
- [Google Scholar]
- Mahan LK, Escott-Stump S, eds. Medical Nutrition Therapy for renal disorders in Krause's Food, Nutrition, and Diet Therapy (11th ed). Philadelphia PA: Saunders; 2004. p. :974.







