Translate this page into:
Over-immunosuppression can be life threatening in minimal change disease
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
A 32-year-old male developed pedal edema, facial puffiness and frothing of urine. Urine examination showed 3+ protein, 3-4 red blood cells per high power field, normal hemogram, high serum cholesterol (290 mg/dl), serum creatinine 1.14 mg/dl, serum albumin 1.9 g g/dl, proteinuria of 12 g/day with normal kidneys on ultrasonogram of abdomen. Kidney biopsy showed normal glomeruli with normal tubules, interstitium and blood vessels. If was negative for IgG, IgM, IgA, C3, C1q; the biopsy was reported as minimal change disease (MCD). He was given three doses of methyl prednisolone (1 g daily for 3 days), along with mycophenolate mofetil (MMF) (3 g daily) and tacrolimus (4 mg daily). After 3 days of therapy, he was discharged on tablet prednisolone (80 mg/day), MMF (3 g daily) and tacrolimus (4 mg daily) in divided doses. Proteinuria decreased (588 mg/day) and edema subsided in 2-week time and he was advised to continue the same medications.
After 1 month, he developed loose stools, cough with expectoration and fever and came to our center. He was dehydrated, febrile, and hypotensive. On auscultation, he had crepitations over right infraclavicular and mammary areas. He had anemia, leukocytosis, thrombocytopenia with high C-reactive protein and blood sugars. Creatinine was 1.84 mg/dl, and albumin 3.76 g/dl. Urine protein was negative. He was on prednisolone 80 mg daily, MMF 1.5 g bd and tacrolimus 2 mg bd.
X-ray chest showed non-homogenous opacities with air and fluid level over right mid zone and left mid and lower zones [Figure 1a], suggestive of multiple lung abscesses. Sputum culture grew Klebsiella (extended spectrum beta lactamase negative). He was started on piperacillin tazobactam and levofloxacin. All immunosuppressive medications were stopped. Bronchoscopy showed purulent discharge from the bronchial orifice of the left lower lobe. He was given active chest physiotherapy and postural drainage. S. creatinine came down to normal.
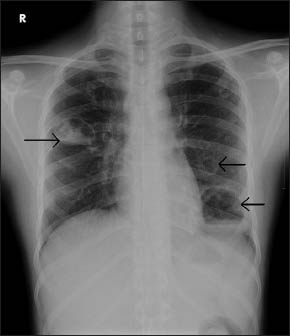
- X-ray chest showing non homogenous opacities with air and fluid level over right mid zone and left mid and lower zones (arrows)
He continued to have fever despite 10 days of antibiotics, repeat chest X-ray showed persistence of lung cavities. He was started on injection meropenem (1 g TID), which was continued for a total 21 days. He responded very well; repeat X-ray chest after four weeks showed normal lung fields [Figure 1b]. He remained edema free without any immunosuppressive medications; he is asymptomatic, has normal blood sugars and is in remission six months later.
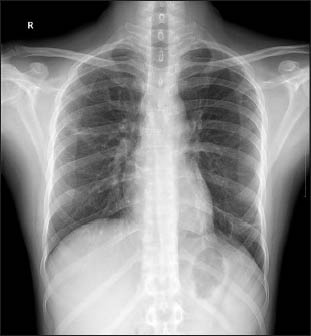
- X-ray chest after 4 weeks of antibiotics showing normal lung fields
MCD accounts for 10-15% of nephrotic syndrome in adults.[1] As per the KDIGO 2012 guidelines the treatment of MCD in adults would be oral prednisolone (1 mg/kg) for four to eight weeks; then taper slowly once remission is achieved.[2] Studies have shown that more than 80% adult patients respond to steroids.[34] Second line agents should be used only in steroid dependent or resistant cases.[5]
This patient was started on treatment with three immunosuppressive drugs in high doses, which was inappropriate and not evidence based. Combining multiple immunosuppressive drugs for a patient with MCD can lead to over immunosuppression and can cause potentially lethal infections, as happened in this patient. The specialists need to be aware of the latest updates and guidelines on treatment of diseases so that excessive immunosuppression does not cause harm to patients.
References
- KDIGO clinical practice guideline for glomerulonephritis. Kidney Int Suppl. 2012;2:177-80.
- [Google Scholar]
- Adult-onset minimal change nephrotic syndrome: A long-term follow-up. Kidney Int. 1986;29:1215-23.
- [Google Scholar]
- Steroid responsiveness and frequency of relapse in adult-onset minimal change nephrotic syndrome. Am J Kidney Dis. 2002;39:503-12.
- [Google Scholar]
- Adult minimal-change disease: Clinical characteristics, treatment, and outcomes. Clin J Am Soc Nephrol. 2007;2:445-53.
- [Google Scholar]






