Translate this page into:
Prospective blood pressure measurement in renal transplant recipients
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Blood pressure (BP) control at home is difficult when managed only with office blood pressure monitoring (OBPM). In this prospective study, the reliability of BP measurements in renal transplant patients with OBPM and home blood pressure monitoring (HBPM) was compared with ambulatory blood pressure monitoring (ABPM) as the gold standard. Adult patients who had living-related renal transplantation from March 2007 to February 2008 had BP measured by two methods; OBPM and ABPM at pretransplantation, 2nd, 4th, 6th, and 9th months and all the three methods: OBPM, ABPM, and HBPM at 6 months after transplantation. A total of 49 patients, age 35 ± 11 years, on prednisolone, tacrolimus, and mycophenolate were evaluated. A total of 39 were males (79.6%). Systolic BP (SBP) and diastolic BP (DBP) measured by OBPM were higher than HBPM when compared with ABPM. When assessed using OBPM and awake ABPM, both SBP and DBP were significantly overestimated by OBPM with mean difference of 3-12 mm Hg by office SBP and 6-8 mm Hg for office DBP. When HBPM was compared with mean ABPM at 6 months both the SBP and DBP were overestimated by and 7 mm Hg respectively. At 6 months post transplantation, when compared with ABPM, OBPM was more specific than HBPM in diagnosing hypertension (98% specificity, Kappa: 0.88 vs. 89% specificity, Kappa: 0.71). HBPM was superior to OBPM in identifying patients achieving goal BP (89% specificity, Kappa: 0.71 vs. 50% specificity Kappa: 0.54). In the absence of a gold standard for comparison the latent class model analysis still showed that ABPM was the best tool for diagnosing hypertension and monitoring patients reaching targeted control. OBPM remains an important tool for the diagnosis and management of hypertension in renal transplant recipients. HBPM and ABPM could be used to achieve BP control.
Keywords
Ambulatory blood pressure monitoring
blood pressure
home blood pressure monitoring
office blood pressure monitoring
renal transplantation
Introduction
Office blood pressure monitoring (OBPM) as is usually practiced may not provide a representative measure of an individual's blood pressure (BP) outside the medical setting. Out-of-office BP assessment with home blood pressure monitoring (HBPM) and ambulatory blood pressure monitoring (ABPM) have the potential for a better classification of the hypertensive status compared with OBPM. HBPM devices are endorsed for repeated measurements outside the medical environment.[12]
ABPM is currently the gold standard for the correct diagnosis of hypertension as it provides extensive information on several BP parameters other than average BP, including BP variability, morning BP surge, BP load, and nocturnal drop in BP.[3] ABPM is not widely available in primary care practice and is considered most helpful, when HBPM values are borderline. HBPM is recommended as an initial step to screening out-of-office BP (1-3) leading to an ABPM, for confirmation. However, it is not well-known whether this strategy is appropriate because ABPM and HBPM may provide different and complementary information. Studies have shown that these two measures do not have a high correlation[4] or a good agreement.[5] The reliability of the three methods of BP measurement has been based on one or two time points following renal transplantation.[67] To assess the reliability of the three methods, prospective and longitudinal studies have been suggested. This study assess the reliability of OBPM and ABPM from the pretransplant period, 2nd, 4th 6th, and 9th months and all the three methods at 6th month after renal transplantation.
Patients and Methods
Patients receiving living-related renal transplantation from March 2007 to February 2008 at Christian Medical College, Vellore, India were prospectively followed-up with the study protocol till January 2009, after a written consent. The protocol was approved by the Clinical Investigation Ethics Committee and the Institutional Review Board.
Study subjects
Inclusion criteria included renal allograft recipients ≥18 years, treated with prednisolone, tacrolimus, and mycophenolate. The exclusion criteria included recipients <18 years, inability to complete a 9-month follow-up, death, or allograft failure during the study period.
Study protocol
Baseline evaluation prior to and at 9th month following transplantation included measurements of OBPM and ABPM and instructions for patients on the use of HBPM with a mercury sphygmomanometer. Further, at 2nd, 4th, 6th, and 9th months follow up period. OBPM and ABPM were done. All the three methods of BP measurement were performed at the 6th month.
BP monitoring
Data from the ABPM were used as the gold standard. BP was defined as controlled when both systolic BP (SBP) and diastolic blood pressure (DBP) were within the normal range, defined by The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC 7), for all the methods used. The normal values used were: OBPM (<140/90 mm Hg) and HBPM (<135/85 mm Hg) and hypertension was diagnosed when DBP and/or SBP were higher than the defined ranges. Similarly, BP <130/80 mm Hg with OBPM was considered “controlled” in this study.[8]
OBPM protocol
Three measurements were taken by physicians according to guidelines of the World Health Organization. BP was measured with a standard mercury sphygmomanometer, sitting, after 10 min of rest with the cuff size adjusted for the individual's arm circumference. Timed measurements of OBPM were taken during the initiation and termination of the ABPM on the nonfistula arm and an average of the three measurements were compared with ABPM.
ABPM protocol
BP was recorded with an ambulatory blood pressure monitor with software (Welch Allyn ABPM 6100, 2007, New York) over 24 hrs on a regular working day starting at 9 am at half hour intervals till 9 am the next day with a record of the time they went to bed and awoke. BP profiles were obtained at 1 week prior to transplantation and at 2nd, 4th, 6th, and 9th months after transplantation. The means of BP while awake, BP during sleep, and for 24 h BP as well as pulse rates were extracted from the data.
HBPM protocol
A relative staying continually with the patient (usually donors, spouse, parents, or siblings) was trained and supervised by a trained nurse to measure BP at home with a mercury sphygmomanometer in the clinic for consistency and accuracy. At the 6th month HBPM was done at 8 am, 12 pm, 4 pm, and 8 pm; four times on each occasion, for 7 consecutive days. The mean values of the DBP and SBP were used for comparison. OBPM and ABPM were done a week before HBPM.
Statistical methods
Descriptive statistics such as mean, standard deviation (SD), and proportions were used for demography, clinical, laboratory characteristics, and OBPM, HBPM and ABPM registries. Student's t-test was done to compare means of BP. Linear regression was used to estimate the change in BP per month. Bootstrap simulations were done 1000 times to compare two means and also for the regression estimation of change per month, assuming a normal distribution. Bland-Altman (mean difference) plot was created over time for ABPM (2nd, 4th, and 6th months post transplant) against a mean difference of OBPM-ABPM and HBPM (6th month) against a mean difference of OBPM-HBPM, for both SBP and DBP. Prevalence adjusted and bias adjusted kappa was used to study agreement. All analyses were performed using a SPSS 16.0.
Results
We prospectively evaluated 49 living-related renal allograft recipients, 39 males, during the period of 2006-2009 on tacrolimus, prednisolone, mycophenolate mofetil/sodium before transplantation, at 2nd, 4th, 6th, and 9th months after transplantation. The prevalence of pretransplant hypertension was 91% and 71.4%, had posttransplant hypertension with 45% of patients on ≤2 drugs. The average estimated glomerular filtration rateable and creatinine at each follow-up during the study period were approximately 70 mL/min and 1.2 mg% [Tables 1 and 2].


Table 3 presents the mean (SD) of SBP measured by awake ABPM and OBPM at the pretransplant, 2th, 4th, 6th, and 9th months and HBPM, awake ABPM and OBPM at the 6th month. The mean and 95% confidence interval (CI) of difference between these two methods and Bootstrap-based simulated mean difference and the 95% CI are also presented. At pretransplant assessment, the mean difference between the two methods was − 12.4 and 95% CI (−18.7, -6.2) implying that OBPM reading was significantly higher (P < 0.05). The difference was − 1.1 (-5.0, 2.8), −3.8 (−7.4, −0.2), −1.8 (-5.2, 1.6), and − 2.0 (-5.6, 1.6) mm Hg at 2th, 4th, 6th, and 9th months, respectively. The simulated 95% CI were similar to the 95% CI.
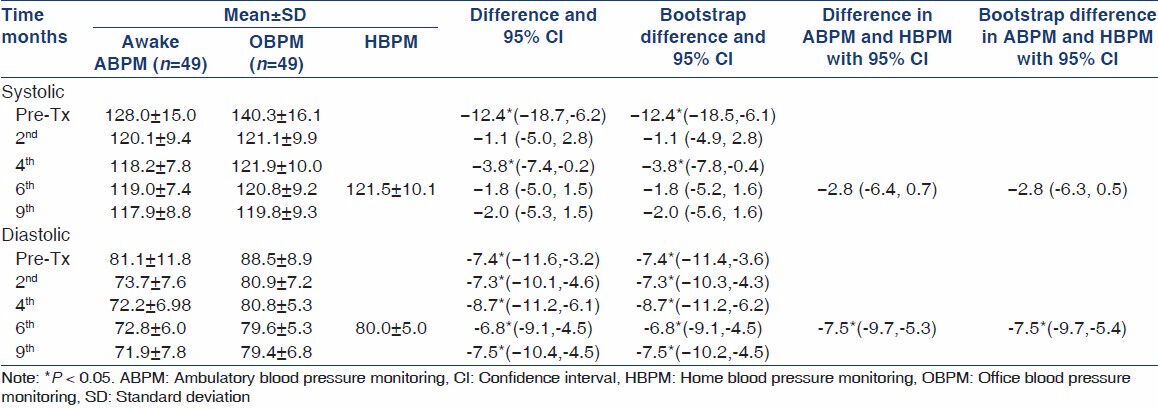
Similarly for DBP, the mean (SD) and 95% CI of difference between these two methods and Bootstrap-based simulated mean difference and the 95% CI are presented in Table 3. At pretransplant measurement, the mean difference between the two methods was -7.4 and 95% CI (−11.6, −3.2) implying that OBPM was significantly higher (P < 0.05). The difference and 95% CI was-7.3 (−10.3, −4.3), −8.7 (−11.2, −6.2), −6.8 (−9.1, −4.5) and −7.5 (−10.4, −4.5) mmHg at 2th, 4th, 6th, and 9th months, respectively. At all time points of measurement, the difference was statistically significant with average of an 8 mm Hg over estimation consistently by the OBPM. The simulated 95% CIs were similar to the 95% CI.
ABPM and HBPM at 6th month
The mean (SD) of SBP at 6th month was 118.6 (7.3) and 121.4 (10.1) by ABPM and HBPM, respectively. The difference between these was −2.8 mm Hg with 95% CI (−6.4, 0.7). However, the bootstrap 95% CI was (−6.3, 0.5). Similarly, the mean (SD) of DBP at 6th month was 72.4 (6.0) and 79.9 (4.9) mm Hg/h by ABPM and HBPM readings, respectively. The difference between these was −7.6 with 95% CI (−9.7, −5.3) and the bootstrap 95% CI was (−9.7, −5.3) mm Hg.
Mean difference plots in awake SBP of ABPM and office BP
The mean difference plot of SBP for different time points is shown in Figure 1. At the pretransplant phase, the scatter was evenly distributed over the range of SBP suggesting that there is an even estimation of SBP for the particular range of SBP. However, during the post transplant phase there was a systematic over estimation of SBP by OBPM at all points, with a good agreement.

- Awake systolic blood pressure in ambulatory blood pressure monitoring and office systolic blood pressure
The mean difference plot of DBP at various time points is given in Figure 2. The scatter showed an evenly distributed overestimation of 8 mm Hg at all-time points.
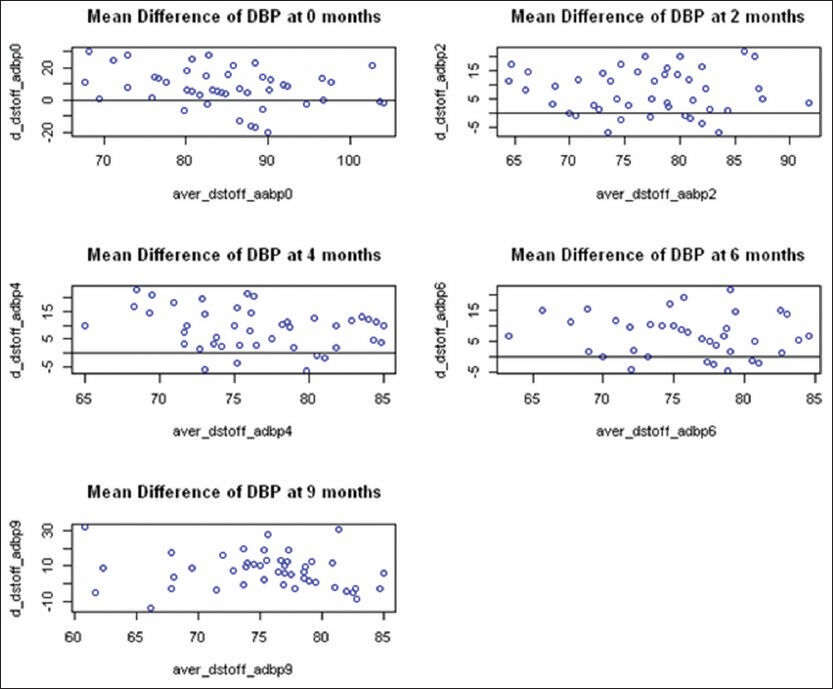
- Awake DBP in ambulatory blood pressure monitoring and office diastolic blood pressure
The mean difference plot of SBP and DBP at 6th month is given in Figure 3. At 6th month post transplantation, the scatters were evenly distributed showing overestimation of SBP of 2.8 mm Hg and DBP 7.6 mm Hg consistently.

- Home blood pressure monitoring and ambulatory blood pressure monitoring at 6th month
The concordance rate was 69% for the diagnosis of hypertension at baseline; however, this increased to 86% at 2nd month and remained above 90% subsequently. This was reflected in the kappa statistics showing similar agreement. The concordance rate for target goal of BP (<130/80 mm Hg) showed that HBPM specificity (83%) was higher at 6 months than OBPM (50%) when compared with ABPM [Table 4].
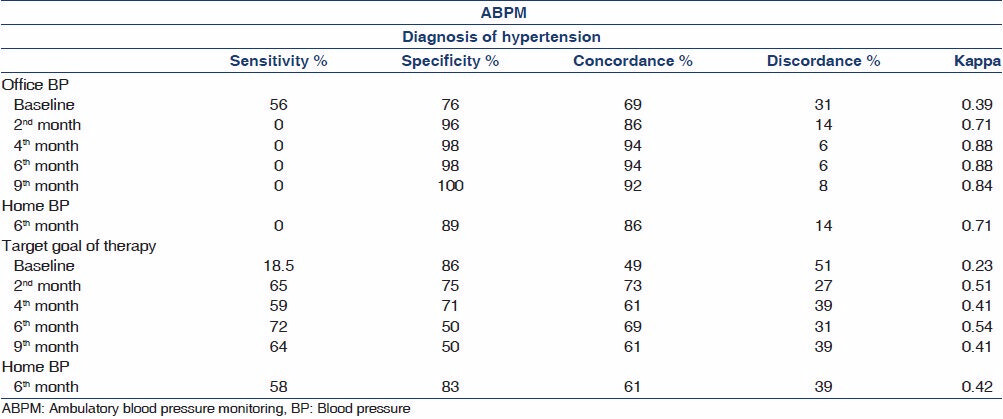
On comparing the three methods of BP measurements by latent class model analysis, ABPM had the best results both for the diagnosis of elevated BP (sensitivity 6.8%; specificity 100%) and measurement of reaching the targets of BP (sensitivity 99%; specificity 99%).
Discussion
The use of OBPM in the management of clinical hypertension is limited by fewer measurements and the white-coat effect.[9] Currently ABPM is recommended, over the OBPM.[910] This study suggests HBPM appears to be a valid and a simple alternative to OBPM and ABPM. It has the advantages of convenience and cost savings while representing BP readings in the ambient environment. HBPM needs further validation in clinical practice.[11]
The study shows that although both OBPM and HBPM presented a fair correlation with ABPM, the HBPM is superior with less error. HBPM was more specific in the assessment of the targets of therapy of BP (<130/80 mm Hg). A recent study concluded that despite their methodological differences, there seems to be considerable similarity between morning home BP and morning ambulatory BP and thus these methods appear to be interchangeable in the assessment of hypertension.[12]
This study have taken multiple measurements for HBPM, OBPM, and ABPM to produce the maximum reliability among the three methods of BP measurements as in other studies[3467] in literature, where the measurements have been few. We have used ABPM as a “gold standard”[13] for comparing with HBPM using the average daytime BP for comparison as in another report by Agena et al.[6] With HBPM, there is no consensus regarding the frequency of readings or the days needed for observation. Studies are based on reproducibility and consistency of BP with HBPM.[14]
During this study, with OBPM and HBPM most of the BP measurements obtained at the same time were similar. The Bootstrap simulations were similar to the observations from the 49 patients with normal distribution indicating the results with a sample size though small are valid.
Our transplant clinic adequately controlled BP in 91% of patients compared with 5% in the study by Paoletti et al.,[13] and 36% at the last follow-up in Agena's study.[6] The large difference is partly due to the variation in the definition of normotension in the setting of ABPM, 130/80 mmHg in Paoletti's study, and 135/85 mmHg in our patients who had a better allograft function.
The present study showed SBP with OBPM were significantly higher at all time points as compared with ABPM similar to other report.[13] However in contrast to two studies[615] where the DBP measurements with OBPM did not show much variation with the awake ABPM, this study demonstrated that OBPM and HBPM overestimated BP when compared with awake ABPM. The degree of overestimation by HBPM was lower than OBPM in our study has also shown by Agena et al.[6] The manual sphygmomanometer readings could be replaced by automated OBPM reducing errors and are similar to mean awake ABPM.[12]
ABPM reflect the mean measurements of BP taking into the consideration the nocturnal dipping, the timing of antihypertensive medications without the influence of white-coat effect, unlike OBPM. No algorithm or regression equation can be determined from comparative studies, because ABPM is both underestimated and overestimated by OBPM. Overestimation may be attributable to white-coat hypertension, whereas underestimation could be explained by the fact that the studied patients take their antihypertensive medication shortly before the OBPM or because they have a high nocturnal BP.[16]
The latent class model analysis showed that ABPM is the best modality for the diagnosis and assessment of the target of ≤135/85 mm Hg in hypertensive renal transplant recipients. ABPM is expensive and center limited; while HBPM is relevant, reliable, and is easier to incorporate into the home care of renal transplant patients.
Conclusion
ABPM is the best modality in diagnosis and treatment of hypertension in renal transplant recipients. However, in resource-limited situations multiple measurements of HBPM would be a valid alternative, while OBPM would facilitate the diagnosis of hypertension. The care of a hypertensive renal transplant recipient should shift home with a greater patient involvement.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC).J. Hypertens. 2007;25:1105-87.
- [Google Scholar]
- Recommendations for blood pressure measurement in humans and experimental animals: Part 1: Blood pressure measurement in humans: A statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension. 2005;45:142-61.
- [Google Scholar]
- ASH Position Paper: Home and ambulatory blood pressure monitoring. When and how to use self (home) and ambulatory blood pressure monitoring. J Clin Hypertens (Greenwich). 2008;10:850-5.
- [Google Scholar]
- Relative effectiveness of clinic and home blood pressure monitoring compared with ambulatory blood pressure monitoring in diagnosis of hypertension: Systematic review. BMJ. 2011;342:d3621.
- [Google Scholar]
- Masked hypertension assessed by ambulatory blood pressure versus home blood pressure monitoring: Is it the same phenomenon? Am J Hypertens. 2005;18:772-8.
- [Google Scholar]
- Home blood pressure (BP) monitoring in kidney transplant recipients is more adequate to monitor BP than office BP. Nephrol Dial Transplant. 2011;26:3745-9.
- [Google Scholar]
- Home and office blood pressure monitoring in renal transplant recipients. J Transplant. 2012;2012:702316.
- [Google Scholar]
- Ambulatory blood-pressure monitoring in clinical practice. N Engl J Med. 2003;348:2377-8.
- [Google Scholar]
- Ambulatory blood pressure monitoring and cardiovascular risk in resistant hypertensive women. Arq Bras Cardiol. 2009;92:448.
- [Google Scholar]
- Comparison of agreement between clinic and home-measured blood pressure in the Finnish population: The Finn-HOME Study. J Hypertens. 2006;24:1549-55.
- [Google Scholar]
- Automated office versus home measurement of blood pressure in the assessment of morning hypertension. Blood Press Monit. 2012;17:24-34.
- [Google Scholar]
- Association of arterial hypertension with renal target organ damage in kidney transplant recipients: The predictive role of ambulatory blood pressure monitoring. Transplantation. 2009;87:1864-9.
- [Google Scholar]
- How many times should blood pressure be measured at home for better prediction of stroke risk. Ten-year follow-up results from the Ohasama study? J Hypertens. 2004;22:1099-104.
- [Google Scholar]
- Evaluating the utility of ambulatory blood pressure monitoring in kidney transplant recipients. Clin Transplant. 2012;26:E465-70.
- [Google Scholar]
- Ambulatory blood pressure monitoring in renal transplantation: Should ABPM be routinely performed in renal transplant patients? Transplantation. 2003;76:1640-2.
- [Google Scholar]







