Translate this page into:
Immunoglobulin G4-related tubulointerstitial nephritis associated with interstitial pulmonary disease: Report of a case with review of literature
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Immunoglobulin G4-related disease (IgG4-RD) is an emerging clinicopathological entity. Renal involvement is dominated by tubulointerstitial nephritis (TIN) with IgG4-positive plasma cells and fibrosis. IgG4-RD commonly affects middle-aged to elderly men with accompanying extra-renal lesions such as sialadenitis, lymphadenopathy, or type 1 autoimmune pancreatitis, all of which respond favorably to corticosteroid therapy. The disease burden of IgG4-related kidney disease (IgG4-RKD) in India remains largely underestimated. We report a case of IgG4-RKD manifesting as TIN associated with interstitial pulmonary disease, illustrating typical clinico-pathologic, serologic, immuno-histochemical, and ultrastructural features of this condition. In view of potential amelioration of renal dysfunction with appropriate therapy, the need for awareness of this condition and early diagnosis is highlighted.
Keywords
Corticosteroid therapy
immunoglobulin G4-related disease
immunoglobulin G4-related kidney disease
tubulointerstitial nephritis
Introduction
Immunoglobulin G4-related disease (IgG4-RD) is a systemic fibro-inflammatory immune-mediated disorder, first described in relation to the pancreas (as type 1 autoimmune pancreatitis [AIP]) and now recognized in almost every major organ, with tubulointerstitial nephritis (TIN) being the most common manifestation in IgG4-related kidney disease (IgG4-RKD).[1] IgG4-RD is characterized by abundant levels of IgG4-positive plasma cells and T-lymphocyte infiltration in various organs, variable degrees of fibrosis with characteristic “storiform” pattern, and high levels of serum IgG4 (60-70% of patients). Various glomerular pathologies, particularly membranous nephropathy, have been reported concurrent with TIN in IgG4-RKD. Common extra-renal associations include sialadenitis, lymphadenopathy, and AIP. We herein describe a rare case of IgG4-related TIN associated with interstitial pulmonary disease.
Case Report
A 56-year-old man presented with 3 month history of progressively increasing shortness of breath with minimally productive cough and weight loss of 7 kgs. There were no genitourinary symptoms. He did not provide any history suggestive of collagen vascular disorders, or vasculitis. There was no history of analgesic abuse or intake of nephrotoxic agents. He was empirically treated elsewhere with anti-tuberculous therapy 1 year ago for complaints of chronic productive cough. He did not have diabetes or hypertension. He was a nonsmoker. There was no history of atopy.
At presentation, his blood pressure was 112/80 mmHg, heart rate 88/min and respiratory rate 18/min. Physical examination revealed widespread bilateral expiratory rhonchi and coarse crepitations over the left interscapular region. Examination of other systems was unremarkable. The relevant laboratory investigations are summarized in Table 1. Transbronchial lung biopsy showed chronic interstitial pneumonia with lympho-histiocytic aggregates. Immunoglobulin G4 staining was not done in lung biopsy specimen. All cultures sent from the bronchial biopsy procedure were sterile.

Renal biopsy performed in view of renal dysfunction with proteinuria showed expansile, destructive interstitial fibrosis with dense plasma cell rich inflammatory infiltrates, tubular destruction, and atrophy [Figure 1a]. The IgG4 immunostain showed up to 25 IgG4-positive plasma cells per high-power field in the most concentrated areas [Figure 1b]. Electron microscopic examination confirmed the light microscopic findings of “bird's eye” interstitial fibrosis and demonstrated the presence of electron-dense deposits in few of the remnant tubular basement membranes (TBMs) [Figure 2a–c].

- (a) Expansile whorling interstitial fibrosis with dense lymphoplasmacytic infiltrate and few eosinophils. Note widening of intertubular spaces with tubular attenuation and relative sparing of glomeruli (hematoxylin and eosin, ×400). (b) Dense interstitial lymphoplasmacytic infiltrate composed of numerous immunoglobulin G4-positive plasma cells (black arrow) (anti - IgG4 immuno - histochemistry, ×400)
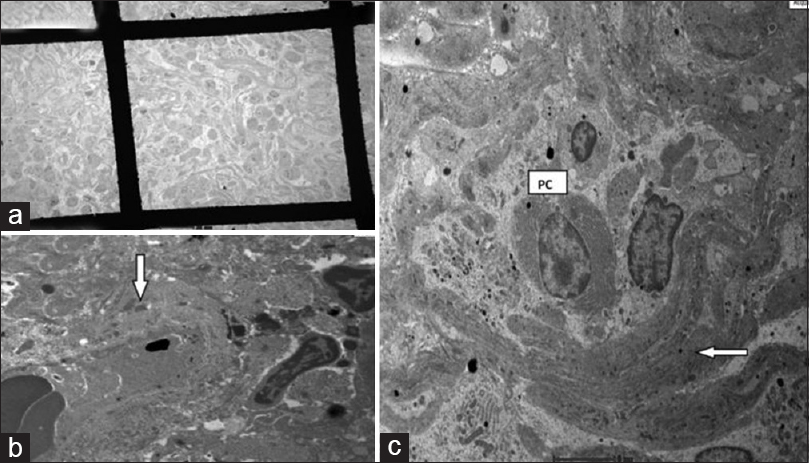
- (a) Extensive interstitial fibrous deposition encircling nests of lymphoplasmacytic cells, demonstrating bird's eye pattern of fibrosis (transmission electron microscopy, ×610). (b) Bird's eye fibrosis in immunoglobulin - G4 tubulointerstitial nephritis - fibrous bundles (white arrow) encircling nests of swollen inflammatory cells (transmission electron microscopy, ×2550) (plasma cell). (c) Scattered electron-dense deposits (white arrow) in thickened tubular basement membrane remnants (transmission electron microscopy, ×6000)
No other extra-renal involvement was detected through laboratory investigations or imaging. A diagnosis of IgG4 nephropathy was made based on elevated serum IgG4 levels, hypocomplementemia, polyclonal hypergammaglobulinemia, characteristic renal histology, immuno-histochemistry, and electron microscopy. He was started on high-dose oral steroids and showed marked improvement in serum creatinine from 3.39 to 2.3 mg/dl within 4 weeks of follow-up. Also, respiratory symptoms improved and lung lesion disappeared on further imaging studies.
As IgG4 staining has not been carried out in the lung biopsy specimen, interstitial pneumonia could represent either an independent pathology or IgG4-RD involving kidney and lung simultaneously as both have good response to steroid treatment. The serum IgG4 level was not repeated to monitor response in this patient as it is an expensive ancillary investigation and moreover the patient had good clinical response.
Discussion
Immunoglobulin G4-RKD is a comprehensive term for renal lesions associated with IgG4-RD, a novel clinico-pathological entity characterized by a dense lymphoplasmacytic infiltrate rich in IgG4-positive plasma cells with varying degrees of fibrosis affecting several organs. IgG4-RD has been known by other names in the past such as Mikulicz disease, Küttner's tumor, Reidel's thyroiditis, fibro sclerosing pancreatitis, etc., depending on the organs involved.[12]
First reported by Sarles et al.[3] in 1961 as a case of sclerotic pancreatitis accompanied by hypergammaglobulinemia, it was renamed as AIP by Yoshida et al.[4] in 1995. The main features are of organ enlargement or tumefaction due to massive infiltration by IgG4-positive plasma cells with ensuing fibrosclerosis.[5]
Among all the four subclasses of IgG, IgG4 is the least common and has weaker interchain bonds, thus making it incapable of fixing complements or activating immune responses.[6] The pathogenesis of IgG4-RD is not well understood with possible involvement of both autoimmune and allergic pathways.[789]
Key histopathological features include immunohistochemical demonstration of increased number of IgG4-positive plasma cells and storiform pattern of fibrosis with or without accompanying eosinophils. Unique to the kidney is the demonstration of “bird's eye” pattern of fibrosis composed of nests of inflammatory cells surrounded by irregular fibers, resembling “bird's eye” grain pattern of maple wood,[10111213] as seen in our case. Electron microscopic demonstration of immune deposits in TBMs is indicative of the renal antigenic stimulus in IgG4-related TIN and was identified in our case also. To the best of our knowledge, this is the first report from India of IgG4-related TIN associated with interstitial pulmonary disease, where ultrastructural examination of renal biopsy to identify TBM-immune deposits and serum IgG4 analysis were carried out.
Apart from TIN, various forms of glomerulonephritis[1415161718] and hydronephrosis secondary to IgG4-related retroperitoneal fibrosis[19] have been reported. There are two sets of criteria (Kawano et al.[20] and Raissian et al.[21]) proposed in the literature for diagnosing IgG4-related TIN. Kawano et al. from Japan initially proposed criteria from retrospective analysis of 41 patients with IgG4-related TIN.[20] Further, Raissian et al. from Mayo clinic, Minnesota, retrospectively analyzed the histopathology of 35 patients with IgG4-TIN and proposed modified diagnostic criteria based on combined histologic, immuno-phenotypic, clinical, radiographic, and laboratory features[21] [Table 2].

Our patient satisfies all the individual criteria of Raissian et al. with the presence of ≥10 IgG4-positive plasma cells per high-power field in renal biopsy and also had other features such as enlarged kidneys, hypergammaglobulinemia, elevated serum IgG4 level, hypocomplementemia, and extra-renal involvement. The cytoplasmic-antineutrophil cytoplasmic antibody (c-ANCA) elevation in this patient can be explained by IgG4-RD related autoimmune etiology as lung and renal biopsies did not show any evidence of vasculitis.
Our patient satisfies the recent consensus comprehensive diagnostic criteria for IG4-RD, 2011[22] viz. (a) serum IgG4 concentration >135 mg/dl, (b) >40% of IgG-positive plasma cells being IgG4 + ve, and (c) >10 IgG4 positive plasma cells/high-powered field of biopsy sample.
The closest mimics of this disease are Sjogren's syndrome and other autoimmune diseases like sarcoidosis. In our case, we have ruled out both because the serology of Sjogren's diseases (anti-SSA and anti-SSB) was negative and angiotensin converting enzyme level was normal.
The natural history and prognosis are not well described. The disease shows good response to treatment, mainly steroids[2324] as evident in the present case. Relapses are common after discontinuation of steroids.[2324] Other drugs such as azathioprine, mycophenolate mofetil, and methotrexate can be tried as glucocorticoid-sparing agents or as maintenance drugs after glucocorticoid-induced remissions, but their efficacy warrants to be proven in clinical trials. Anecdotal reports of B-cell depletion with rituximab appear to be helpful in those with recurrent or refractory disease.[25]
Conclusion
Immunoglobulin G4-RD is a novel autoimmune disease that involves multiple organs including the kidneys characterized by hypergammaglobulinemia, hypocomplementemia, and elevated serum levels of IgG4/IgG with distinctive histological findings. Appropriate institution of corticosteroid therapy in IgG4-RKD leads to rewarding amelioration of the renal dysfunction and also to the resolution of radiological and serological abnormalities. However, as any delay in treatment may result in irreversible renal failure, prompt and correct diagnosis is critical to the management. This illustrative case is presented not only for its rarity, but also to highlight the need for increased awareness in the medical fraternity regarding this potentially treatable disorder, in order to facilitate early diagnosis.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- A novel clinical entity, IgG4-related disease (IgG4RD): General concept and details. Mod Rheumatol. 2012;22:1-14.
- [Google Scholar]
- Chronic inflammatory sclerosis of the pancreas - An autonomous pancreatic disease? Am J Dig Dis. 1961;6:688-98.
- [Google Scholar]
- Chronic pancreatitis caused by an autoimmune abnormality. Proposal of the concept of autoimmune pancreatitis. Dig Dis Sci. 1995;40:1561-8.
- [Google Scholar]
- Clinicopathological characteristics of patients with IgG4-related tubulointerstitial nephritis. Kidney Int. 2010;78:1016-23.
- [Google Scholar]
- Two critical genes (HLA-DRB1 and ABCF1) in the HLA region are associated with the susceptibility to autoimmune pancreatitis. Immunogenetics. 2007;59:45-52.
- [Google Scholar]
- Autoimmune pancreatitis: A systemic immune complex mediated disease. Am J Surg Pathol. 2006;30:1537-45.
- [Google Scholar]
- Th2 and regulatory immune reactions are increased in immunoglobin G4-related sclerosing pancreatitis and cholangitis. Hepatology. 2007;45:1538-46.
- [Google Scholar]
- Light-microscopic characteristics of IgG4-related tubulointerstitial nephritis: Distinction from non-IgG4-related tubulointerstitial nephritis. Nephrol Dial Transplant. 2012;27:2755-61.
- [Google Scholar]
- Characteristic tubulointerstitial nephritis in IgG4-related disease. Hum Pathol. 2012;43:536-49.
- [Google Scholar]
- Immunohistochemical characteristics of IgG4-related tubulointerstitial nephritis: Detailed analysis of 20 Japanese cases. Int J Rheumatol. 2012;2012:609795.
- [Google Scholar]
- Consensus statement on the pathology of IgG4-related disease. Mod Pathol. 2012;25:1181-92.
- [Google Scholar]
- IgG4: A tantalizing link between causes of membranous glomerulonephritis and systemic disease. Kidney Int. 2013;83:348-50.
- [Google Scholar]
- Membranoproliferative glomerulonephritis-like glomerular disease and concurrent tubulointerstitial nephritis complicating IgG4-related autoimmune pancreatitis. Intern Med. 2009;48:157-62.
- [Google Scholar]
- A case of IgG4-related tubulointerstitial nephritis concurrent with Henoch-Schönlein purpura nephritis. Allergy Asthma Clin Immunol. 2011;7:5.
- [Google Scholar]
- Hydronephrosis associated with retroperitoneal fibrosis and sclerosing pancreatitis. Lancet. 2002;359:1403-4.
- [Google Scholar]
- Proposal for diagnostic criteria for IgG4-related kidney disease. Clin Exp Nephrol. 2011;15:615-26.
- [Google Scholar]
- Diagnosis of IgG4-related tubulointerstitial nephritis. J Am Soc Nephrol. 2011;22:1343-52.
- [Google Scholar]
- Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Mod Rheumatol. 2012;22:21-30.
- [Google Scholar]
- The clinical course of patients with IgG4-related kidney disease. Kidney Int. 2013;84:826-33.
- [Google Scholar]
- Treatment approaches to IgG4-related systemic disease. Curr Opin Rheumatol. 2011;23:67-71.
- [Google Scholar]
- Rituximab for the treatment of IgG4-related disease: Lessons from 10 consecutive patients. Medicine (Baltimore). 2012;91:57-66.
- [Google Scholar]







