Translate this page into:
Spontaneous retroperitoneal hemorrhage presenting as hemoperitoneum secondary to renal cyst rupture in a peritoneal dialysis patient with acquired cystic kidney disease
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Spontaneous retroperitoneal hemorrhage (SRH) is a rare and potentially fatal condition. Acquired cystic kidney disease (ACKD) may cause SRH in hemodialysis patients. However, presentation of retroperitoneal hematoma as hemoperitoneum in peritoneal dialysis (PD) patients is exceedingly rare. We report a 44-year-old male PD patient who presented with hemoperitoneum secondary to retroperitoneal hematoma. The reason of SRH was rupture of the cysts of ACKD. The patient underwent unilateral nephrectomy with subsequent disappearance of hemoperitoneum. The importance of this case lies in the fact that the patients who have been receiving dialysis for a long time should be under surveillance in terms of ACKD development and potential associated complications such as cyst hemorrhage and malignancy.
Keywords
Acquired cystic kidney disease
hemoperitoneum
peritoneal dialysis
renal cyst rupture
Introduction
Acquired cystic kidney disease (ACKD) occurs in patients who are on dialysis for end-stage renal disease (ESRD). The prevalence of ACKD is directly related to the duration of dialysis.[1] Hemorrhagic renal cysts are the most frequent complication of patients with ACKD.[2] Bleeding is usually confined within the cyst but occasionally extends into the renal collecting system leading to hematuria or into the perinephric space leading to perirenal hematoma, or retroperitoneal hemorrhage (RH). Perinephric hematomas have been reported in up to 13% of patients with ACKD.[13]
Hemoperitoneum is an unusual complication, and may present in up to 8.4% of cases in patients undergoing peritoneal dialysis (PD).[45] To the best of our knowledge, hemoperitoneum, as a complication of renal cyst rupture in autosomal dominant polycystic KD (ADPKD), has been described only twice in patients on PD.[67] On the other hand, there is only one reported case, in which hemoperitoneum was secondary to cyst rupture of ACKD in PD.[8] Presentation of retroperitoneal hematoma as hemoperitoneum is exceedingly rare.
We describe a PD patient with ACKD who developed hemoperitoneum secondary to retroperitoneal hematoma along with a discussion of the relevant literature.
Case Report
A 44-year-old man with ESRD caused by hypertensive nephropathy had been treated with hemodialysis for 3 years before being converted to PD. The patient presented with abdominal pain, left-sided loin pain and bloody peritoneal effluent during the 7th year of PD treatment. His blood pressure was 140/80 mmHg and heart rate was 82 bpm and rhythmic. He had low grade fever of 38.3°C. There was tenderness over abdomen and left loin. There was neither rigidity nor rebound tenderness over these areas. He denied diarrhea, vomiting, syncopal episode, and bloody stool. His peritoneal effluent seemed hemorrhagic, presented with red blood cells of 2000/mm3 and 0.1% of hematocrit. White cell count and differential of the peritoneal outflow fluid revealed a total count of 1540/mm3 (83% neutrophils). Laboratory values were as follows; white blood cells: 16.4 × 103, hemoglobin: 8 g/dl, C-reactive protein: 69 mg/L, erythrocyte sedimentation rate: 46 mm/h, and procalcitonin: 14.2 mg/dl. Coagulation profile and liver tests were within normal levels. Blood and peritoneal fluid were sent for culture and the patient was placed on ceftriaxone and vancomycin treatment with a presumptive diagnosis of continuous ambulatory PD-related peritonitis. Blood and peritoneal fluid cultures were negative for any bacterial and fungal infection. The hemoglobin value of the patient 2 days prior to current admission was 12.4 g/dl. The patient denied any rectal bleed or bloody vomiting. PD was halted and the patient underwent heparin-free hemodialysis with saline flushes. Abdominal ultrasound showed bilateral shrinked kidneys with multiple small-sized cysts. There was an exophytic cyst measuring 9 cm × 8 cm, filled with blood at the lower pole of the left kidney. Medical records showed that he had no cysts at the start of the renal replacement therapy. Abdominal computed tomography revealed that there was a lesion, which extends from the upper pole of the left kidney to the lower pole through which a hematoma was filling renal parenchyma, subcapsular space and perirenal area [Figure 1]. The patient was transfused with packed red blood cell suspensions and underwent left radical nephrectomy with presumptive diagnoses of renal cell cancer secondary to ACKD or cystic hematoma. Macroscopically, there was a cystic lesion, which was not demarcated from surrounding tissues and filled completely with necrotic bleeding tissues. Histopathologically, no focus of neoplasia was found [Figure 2]. After nephrectomy, hemoperitoneum disappeared and the patient recovered completely. He is still undergoing hemodialysis thrice weekly.

- (a) Sagittal reformatted computed tomography images showing hematoma next to inferior pole of the left kidney (arrow). (b) Hematoma comprising air - fluid level in the renal cyst (arrow)
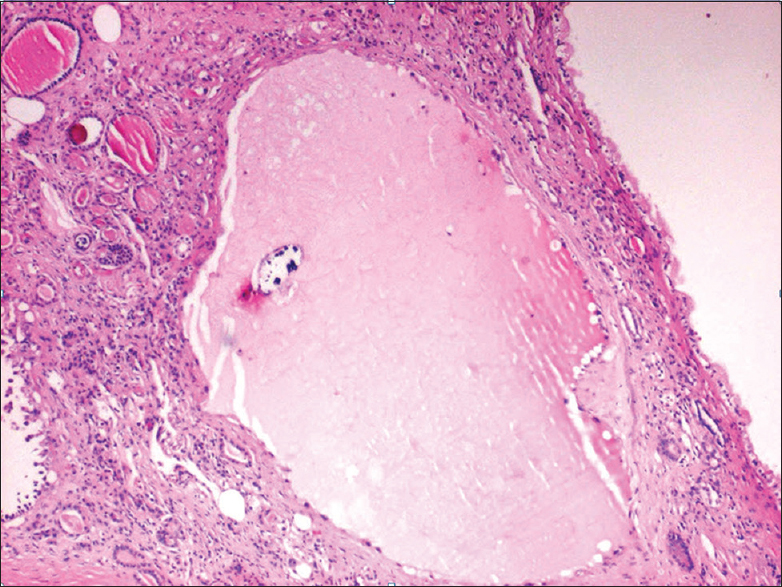
- Cystic structures whose walls are layered with cuboidal epithelium (H and E, ×40)
Discussion
The usual definition of ACKD requires three or more cysts per kidney in a patient on dialysis who does not have a hereditary cause of cystic disease such as ADPKD or tuberous sclerosis. Within the first 3 years of dialysis, approximately 10–20% of patients develop ACKD. By 5 years, 40–60% of patients have ACKD and by 10 years more than 90% of patients exhibit ACKD.[9] There is no difference in prevalence and severity of ACKD between hemodialysis and PD patients.[3]
Our patient had risk factors for development of ACKD, including male gender and long duration of renal replacement therapy. The patient had no family history of ADPKD; moreover, he did not have any cysts in the kidney at the start of the dialysis. Nephrectomy material also histologically confirmed the diagnosis of ACKD [Figure 2].
Approximately 50% of patients with ACKD develop hemorrhagic renal cysts.[12] On the other hand, this rate is much lower in patients with ADPKD (18% in a cohort of 158 patients during a 7-year follow-up).[10] Spontaneous retroperitoneal hemorrhage (SRH) is rare but potentially life-threatening condition.[11] Causes of SRH includes myriad etiologies but the most common cause is kidney neoplasm, angiomyolipoma being predominant.[12] The frequency of SRH is not known in patients undergoing renal replacement therapies, because many studies excluded these patients. Malek-Marín et al.[13] reported a single center incidence of SRH in hemodialysis patients as 0.86 cases/100 patients. When SRH was of renal origin in dialysis patients, the most common cause was cyst rupture in patients with ACKD.[14]
Most patients with SRH secondary to cyst rupture were undergoing hemodialysis compared with PD. This observation has been explained by longer duration of RRT and consequently more severe cystic disease, and heparin anticoagulation.[1]
Another notable observation in SRH secondary to cyst rupture is that there is a remarkable difference in frequencies between SRH due to ACKD and ADPKD. Most of the described patients in the literature had underlying ACKD rather than ADPKD. Some putative factors have been put forward to explain this disparity. The more medullary location of cysts in ADPKD compared with cortically residing cysts of ACKD and differences in the speed of cyst growth might account for differences in observed prevalence of SRH.[13] Among hemodialysis patients, perirenal or retroperitoneal bleeding due to acquired cyst rupture tends to occur after the dialysis session, possibly as a consequence of heparinization.[3]
One of the interesting aspects of the present case is the manifesting as hemoperitoneum instead of RH. A review of the causes of hemoperitoneum by Nace et al.[15] mentioned mostly intraperitoneal pathologies although it does include some extraperitoneal sources. Peritoneal dialysis is a window to the peritoneum and is thus a sensitizer revealing peritoneal pathologies which might otherwise go undiagnosed.[16] To our knowledge, hemoperitoneum, as a complication of renal cyst rupture in ADPKD, has been described only twice in patients on PD. On the other hand, hemoperitoneum secondary to cysts rupture in a PD patient has only been reported once to date.[8] This is not surprising because of retroperitoneal hemorrhage, in theory, should not find its way through the peritoneal membrane. A possible explanation is an adhesion between the cyst's wall and the peritoneum, favored by their anatomical proximity and inflammation secondary to intracystic hemorrhage. These adjoining structures could then rupture as a result of the rising intracystic pressure. Among the more common causes of hemoperitoneum, SRH should also be kept in mind.
Since most of the clinically overt SRH cases in dialysis patients are secondary to rupture of acquired cysts, especially after 5 years of renal replacement therapy, patients should be screened for the presence of ACKD. In patients who had ACKD, this surveillance should be continued because of risk of cyst enlargement and malignancy risk.
Conclusion
Our case report exemplifies a rare PD patient who developed RH presented as hemoperitoneum. The reason of SRH was rupture of cysts of ACKD. SRH is an important and potentially fatal complication. Patients who have a long duration on dialysis should be under surveillance related to ACKD development and associated bleeding risks.
Acknowledgments
Dr. A. G. received grant support from the ERA-EDTA fellowship program. No sources of funding were used to conduct this study or prepare this manuscript.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Natural history of acquired renal cystic disease in dialysis patients: A prospective longitudinal CT study. AJR Am J Roentgenol. 1991;156:501-6.
- [Google Scholar]
- Acquired renal cystic disease and its complications in continuous ambulatory peritoneal dialysis patients. Perit Dial Int. 1992;12:292-7.
- [Google Scholar]
- Hemoperitoneum complicating chronic peritoneal dialysis: Single-center experience and literature review. Am J Kidney Dis. 1992;19:252-6.
- [Google Scholar]
- Recurrent hemoperitoneum complicating continuous ambulatory peritoneal dialysis. Perit Dial Int. 2002;22:488-91.
- [Google Scholar]
- Haemoperitoneum: A frequent complication of CAPD. Perit Dial Bull. 1984;4:S44. [abstract]
- [Google Scholar]
- Bloody effluent during CAPD in a patient with polycystic kidneys. Perit Dial Int. 1988;8:167.
- [Google Scholar]
- Haemoperitoneum caused by bilateral renal cyst rupture in an ACKD peritoneal dialysis patient. Nephrol Dial Transplant. 2006;21:789-91.
- [Google Scholar]
- Epidemiology and investigation of acute abdominal presentations in autosomal dominant polycystic kidney disease. Nephrol Dial Transplant. 2007;22:1483-4.
- [Google Scholar]
- Life-threatening spontaneous retroperitoneal bleeding: A rare complication of oral anticoagulation. Urol Int. 1999;63:247-8.
- [Google Scholar]
- Etiology of spontaneous perirenal hemorrhage: A meta-analysis. J Urol. 2002;167:1593-6.
- [Google Scholar]
- Spontaneous retroperitoneal hemorrhage in dialysis: A presentation of 5 cases and review of the literature. Clin Nephrol. 2010;74:229-44.
- [Google Scholar]
- Spontaneous renal bleeding in a dialysis patient with acquired cystic disease of the kidney: Case report and review of the literature. G Chir. 2007;28:377-9.
- [Google Scholar]
- The risks of laparoscopic cholecystectomy in CAPD compared with hemodialysis patients: A study of ten patients. Perit Dial Int. 1994;14:395-6.
- [Google Scholar]







