Translate this page into:
Eosinophilic granulomatosis with polyangiitis with severe pulmonary hemorrhage treated with rituximab
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Eosinophilic granulomatosis with polyangiitis (EGPA) is characterized by systemic vasculitis, asthma and eosinophilia. Severe pulmonary hemorrhage is rare. Renal involvement is seen in approximately 25% and can vary from isolated urinary abnormality to rapidly progressive glomerulonephritis. There is limited evidence to support the use of rituximab in this condition. We present a patient with EGPA who had severe pulmonary hemorrhage and rapidly progressive glomerulonephritis. He responded to standard treatment including prednisolone, cyclophosphamide, and plasma exchange. He subsequently had a relapse of pulmonary hemorrhage that was treated successfully with rituximab.
Keywords
Eosinophilic granulomatosis with polyangiitis
pulmonary hemorrhage
rituximab
Introduction
Eosinophilic granulomatosis with polyangiitis (EGPA), previously known as Churg-Strauss syndrome, is a multisystem disease characterized by chronic rhinosinusitis, asthma, and prominent peripheral blood eosinophilia. It is characterized by granulomatous inflammation of the respiratory tract and necrotizing vasculitis affecting small to medium sized vessels. The Lanham criteria for the diagnosis of EGPA require the presence of asthma, eosinophilia, and systemic vasculitis involving two or more extrapulmonary organs.[1]
Case Report
A 42-year-old male presented with fever, breathlessness, and hemoptysis of 1-week duration. He had evidence of significant bronchospasm and chest X-ray showed bilateral nonhomogenous opacities suggestive of pulmonary hemorrhage. He had nonblanching purpuric vasculitic rash in the lower limbs. Urinalysis showed microscopic hematuria and proteinuria. The hemoglobin was 10.6 g/dl, total leukocyte count 9,600/cumm with absolute eosinophil count of 2500 cells/cumm. He had elevated inflammatory markers. Urine protein/creatinine ratio showed evidence of significant proteinuria at 2.4:1. Serum creatinine was 1.1 mg/dl on admission that increased to 1.8 mg/dl over the next 3 days. Myeloperoxidase ANCA was strongly positive. He underwent a kidney biopsy that showed a partial cellular crescent formation possessing necrotizing lesion in the underlying glomerular capillary tuft in one of the glomeruli with rest of the glomeruli being unremarkable. Interstitium showed diffuse eosinophilic inflammation and few lymphocytes with focal collection of eosinophils [Figure 1]. There was no evidence of necrotizing arteritis or granuloma formation. Immunofluorescence was negative with a panel of antisera.
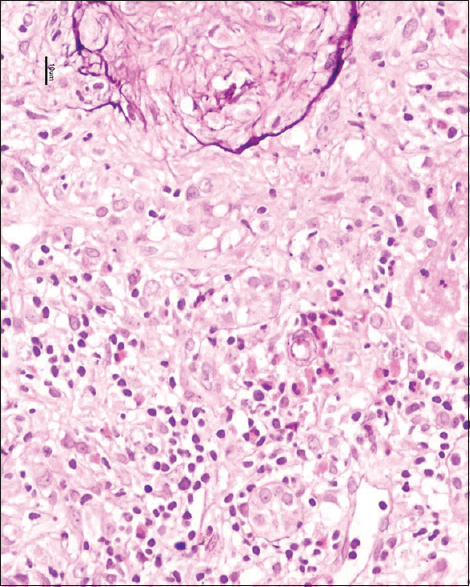
- Renal biopsy showing diffuse eosinophilic inflammation and few lymphocytes with focal collection of eosinophils
He had asthma, eosinophilia, skin vasculitis, and biopsy proven renal vasculitis, and hence he met the Lanham criteria for the diagnosis of EGPA. In view of the severe pulmonary hemorrhage, he was treated with plasma exchange in addition to standard immunosuppression including steroids at 1 mg/kg, and oral cyclophosphamide at 2 mg/kg/day. He showed complete resolution of pulmonary hemorrhage and normalization of creatinine. He was continued on cyclophosphamide for 6 months with reducing dose of prednisolone. The remission was maintained except for a few minor exacerbations of asthma needing increased dose of steroids and bronchodilators. After 6 months of his initial presentation, he was switched from cyclophosphamide to azathioprine at 2 mg/kg and was continued on 7.5 mg prednisolone.
He presented again 21 months later with history of fever, cough, breathlessness, and hemoptysis of 3 days duration. He had bilateral rhonchi on chest examination. Inflammatory markers were significantly elevated but he had no evidence of renal or skin involvement. ANCA was negative by ELISA. Computed tomography (CT) scan of his chest showed focal consolidation with a small cavity [Figure 2].
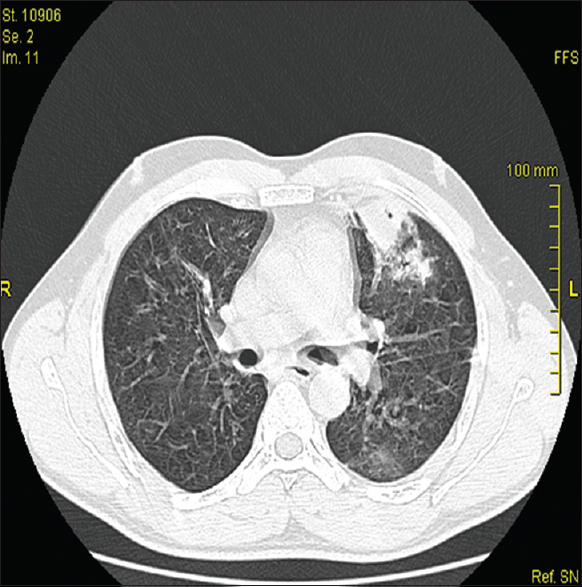
- Computed tomography scan thorax (lung windows) showing focal consolidation with a small cavity
He was treated empirically with intravenous antibiotics. In view of the ongoing pulmonary hemorrhage in spite of broad spectrum antibiotic cover and the CT findings, bronchoscopy, and bronchoalveolar lavage were carried out and the culture was negative. A diagnosis of relapse of EGPA was made. He was treated with three pulses of methyl prednisolone and rituximab infusion at 375 mg/m2. Within 48 h, his symptoms responded and he had three further doses of rituximab at weekly intervals and oral prednisolone at 1 mg/kg. A repeat CT scan done in 4 weeks showed complete resolution. He continues to be in remission 1-year after his relapse.
Discussion
Eosinophilic granulomatosis with polyangiitis presenting as pulmonary renal syndrome is rare. In the largest series with 383 patients, alveolar hemorrhage was diagnosed in 16 (4.2%), 6 of whom had both alveolar hemorrhage and renal manifestation.[2] In this study, renal manifestations were noted in 21.7% of the patients. In another study that examined the prevalence, clinicopathological features and prognosis of renal disease in 116 patients with EGPA, 26.7% had evidence of renal abnormality.[3] Totally, 16 patients underwent renal biopsy of which 11 showed necrotizing crescentic glomerulonephritis. Of these 11, 3 showed eosinophilic-rich interstitial infiltrates. One biopsy in a patient with acute renal impairment showed eosinophilic-rich interstitial infiltrates without glomerular involvement.
ANCA status in EGPA varies with clinical phenotype.[4] ANCA-positive patients are significantly more likely to have necrotizing glomerulonephritis, mononeuritis, and purpura, whereas ANCA-negative cases are significantly more likely to have cardiac and lung involvement. One of the largest retrospective studies on EGPA has demonstrated that ANCA positivity is associated with higher risk of relapse.[2] In our patient, myeloperoxidase-ANCA was strongly positive during the initial presentation and subsequently, the ANCA remained consistently negative. In spite of this, he had florid relapse of the pulmonary hemorrhage but his renal disease continued to be in remission.
The experience of using rituximab, a chimeric anti-CD20 monoclonal antibody that depletes B cells in EGPA is limited to case reports and case series.[567] The largest randomized controlled trial of rituximab in vasculitis has excluded patients with EGPA and patients who were ANCA negative.[8] To our knowledge, severe pulmonary hemorrhage in EGPA responding to rituximab has never been described before.
Conclusion
This is an unusual case of EGPA presenting with severe pulmonary renal syndrome initially and relapsing with pulmonary hemorrhage with excellent response to rituximab. Even though there is good evidence in favor of the use of rituximab in granulomatosis with polyangiitis (Wegener's granulomatosis) and microscopic polyangiitis, the successful use of rituximab in this case adds to the limited evidence base favoring the usefulness of this molecule in EGPA.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Systemic vasculitis with asthma and eosinophilia: A clinical approach to the Churg-Strauss syndrome. Medicine (Baltimore). 1984;63:65-81.
- [Google Scholar]
- Eosinophilic granulomatosis with polyangiitis (Churg-Strauss): Clinical characteristics and long-term followup of the 383 patients enrolled in the French Vasculitis Study Group cohort. Arthritis Rheum. 2013;65:270-81.
- [Google Scholar]
- Successful use of rituximab in a patient with Churg-Strauss syndrome and refractory central nervous system involvement. Ann Rheum Dis. 2010;69:1254-5.
- [Google Scholar]
- Rituximab is effective in the treatment of refractory Churg-Strauss syndrome and is associated with diminished T-cell interleukin-5 production. Rheumatology (Oxford). 2008;47:1104-5.
- [Google Scholar]
- Rituximab for the treatment of Churg-Strauss syndrome with renal involvement. Nephrol Dial Transplant. 2011;26:2865-71.
- [Google Scholar]
- Rituximab versus cyclophosphamide for ANCA-associated vasculitis. N Engl J Med. 2010;363:221-32.
- [Google Scholar]







