Translate this page into:
Two consecutive recurrences of crescentic immunoglobulin A nephropathy in a renal transplant recipient
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
We report a 21-year-old male who developed end-stage renal disease, probably due to immunoglobulin A nephropathy (IgAN), received a renal transplant from his mother, which was lost due to crescentic IgAN after 18 months. Two years later, he received a second transplant from a deceased donor. He developed rapidly progressive graft dysfunction 3 years later. Allograft biopsy revealed crescentic IgAN, which was successfully treated with intravenous steroids and cyclophosphamide. Recurrence of IgAN in two successive allografts in one patient has not been reported previously.
Keywords
Allograft biopsy
crescentic immunoglobulin A
graft loss
recurrence
Introduction
Immunoglobulin A nephropathy (IgAN) is the most common primary glomerulonephritis, characterized by dominant or co-dominant diffuse mesangial deposition of IgA.[1] Progression to end-stage renal disease (ESRD) occurs in 30–50% of patients after 25 years of follow-up.[2] The incidence of posttransplant recurrence of IgAN varied between 20% and 60% at 5 years follow-up in various studies.[3] We describe here a young male who developed crescentic IgAN in two consecutive renal transplantation.
Case Report
A young male developed ESRD at the age of 17 years. His history was remarkable for an episode of macroscopic hematuria during early childhood. He had not undergone kidney biopsy. In 2008, he underwent living – donor renal transplant from his mother elsewhere. He had not received induction immunosuppression and his maintenance immunosuppression included prednisolone, mycophenolate mofetil, and cyclosporine. After a year of normal graft function, he developed macroscopic hematuria, proteinuria, and graft dysfunction. Allograft biopsy revealed crescentic glomerulonephritis with crescents [Figure 1] in four out of eight glomeruli and 3+ mesangial deposits of IgA. No modification of immunosuppression was done. There was a rapid loss of graft function, and he became dialysis dependent within few months and he was on maintenance hemodialysis for next 2 years.

- Renal biopsy of first allograft showing cellular crescents (H and E, ×40)
In 2012, he received a second renal transplant from a deceased donor in our institution. Although anti-thymocyte globulin (ATG) was the preferred induction agent, we could not give due to logistic reason, and he received two doses of basiliximab. He was on prednisolone, mycophenolate mofetil, and tacrolimus. He attained normal graft function on the 15th posttransplant day. Graft function remained stable over the next 3 years with a serum creatinine of 1.3 mg/dl.
Three years after the second transplant, he presented with macroscopic hematuria, nephrotic proteinuria (urine protein creatinine ratio: 5.1) and severe graft dysfunction (serum creatinine 5.2 mg/dl). Serological tests for antinuclear antibody and anti-neutrophil cytoplasmic antibodies were negative. Graft biopsy revealed crescents in nine out of 16 glomeruli [Figure 2]. Viable glomeruli showed mild mesangial matrix expansion and mesangial hypercellularity. Immunofluorescence showed 3+ positivity for IgA [Figure 3] in the mesangium consistent with the diagnosis of crescentic IgAN. He was given pulse methyl prednisolone (1 g × 3 doses) and his serum creatinine declined to 2.4 mg/dl. He was continued with intravenous cyclophosphamide 500/m2 for 6 monthly doses. His serum creatinine during the last visit was 1.8 mg/dl. Timeline of events is given in Table 1.

- Renal biopsy of second allograft showing cellular crescents (PAS, ×40)
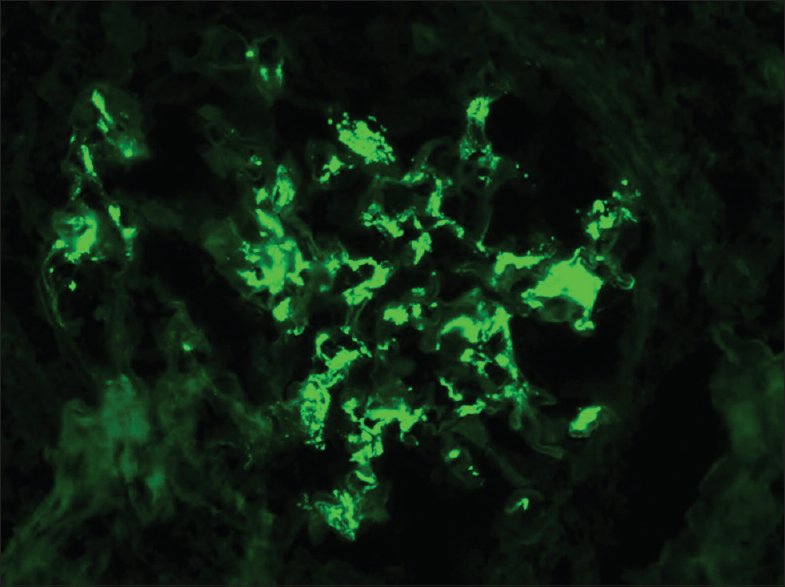
- Immunofluorescence showing intense staining of immunoglobulin A deposits

Discussion
This case exemplifies the rare phenomenon of IgAN recurrence as crescentic glomerulonephritis in two successive renal allografts, one from a living related donor and the other a cadaveric donor. Even though, native kidney biopsy had not been done in our patient, history of macrohematuria during childhood strongly suggests the possibility of IgAN as the cause for renal failure.
The incidence of posttransplant recurrence of IgAN varied between 20% and 60% at 5 years follow-up in various studies.[3] The variation in incidence may be related to differences in indications for allograft biopsy in different centers. The predictors for recurrence of IgAN after transplantation are crescentic glomerulonephritis in native kidney, rapid progression of original disease, younger age at transplantation, zero human leukocyte antigen (HLA) mismatch and use of <3 immunosuppressive medications.[4] Latent IgA deposits in the donor's kidney are associated with high recurrence rate.[5] Recurrence of IgAN has declined progressively from 1980 to 2010, probably due to the use of more potent immunosuppressives.[6] In an analysis of 116 cadaveric donor renal transplant recipients, 10 years cumulative recurrence rate of IgAN was 9% in those who had received ATG induction, whereas it was 41% in the patients who had not received ATG.[7]
In a study of 487 patients with IgAN in the Indian subcontinent, the renal survival rate was 84, 55 and 33% at 1, 5 and 10 years, respectively. Graft loss due to recurrence of IgAN range from 1.3% to 16%.[8] Moroni et al.[9] have reported a recurrence rate of 22% and graft loss of 8.4% in a 10 years follow-up study of 190 renal transplant recipients. If previous graft loss had been due to recurrent IgAN, the risk of subsequent graft loss rose to 25%. Graft failure was not different with various maintenance immunosuppressive combinations. The presence of HLA B8 and DR3 in the recipient is associated with 66% increased the risk of graft loss due to recurrent IgAN.[10] Oxford classification of histopathology predicts poor prognostic factors in recurrent IgAN also.
IgAN is a common cause for posttransplant recurrent glomerulonephritis presenting as crescentic glomerulonephritis. Posttransplant crescentic IgAN portends a poor graft survival. In a study by Kowalewska et al.,[11] de novo or recurrent IgAN was detected in 10 out of 48 patients with crescents in posttransplant graft biopsy. Of them, nine patients progressed to end-stage renal failure at 3 years. Posttransplant recurrent crescentic IgAN has been treated with different regimens including pulse steroids, plasmapheresis followed by high-dose oral steroids and cyclophosphamide.[12]
Our patient is unique in that he had crescentic IgAN in two consecutive allografts – one each from a living related donor and a cadaveric donor. The second graft could be salvaged with intensive immunosuppressants. To the best of our knowledge, there has not been a similar scenario reported in literature.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- IgA glycosylation and IgA immune complexes in the pathogenesis of IgA nephropathy. Semin Nephrol. 2008;28:78-87.
- [Google Scholar]
- Recurrent IgA nephropathy after renal transplantation. Semin Nephrol. 2004;24:287-91.
- [Google Scholar]
- Posttransplant recurrence of primary glomerulonephritis. Clin J Am Soc Nephrol. 2010;5:2363-72.
- [Google Scholar]
- Recurrent and de novo disease after renal transplantation: A report from the renal allograft disease registry. Pediatr Transplant. 2004;8:349-50.
- [Google Scholar]
- Impact of immunosuppressive medication on the risk of renal allograft failure due to recurrent glomerulonephritis. Am J Transplant. 2009;9:804-11.
- [Google Scholar]
- Antithymocyte globulin (ATG) induction therapy and disease recurrence in renal transplant recipients with primary IgA nephropathy. Transplantation. 2008;85:1505-7.
- [Google Scholar]
- Presentation, prognosis and outcome of IgA nephropathy in Indian adults. Nephrology (Carlton). 2005;10:496-503.
- [Google Scholar]
- The long-term outcome of renal transplantation of IgA nephropathy and the impact of recurrence on graft survival. Nephrol Dial Transplant. 2013;28:1305-14.
- [Google Scholar]
- Exclusive characteristics of graft survival and risk factors in recipients with immunoglobulin A nephropathy: A retrospective analysis of registry data. Transplantation. 2005;80:1012-8.
- [Google Scholar]
- IgA nephropathy with crescents in kidney transplant recipients. Am J Kidney Dis. 2005;45:167-75.
- [Google Scholar]
- Steroids and recurrent IgA nephropathy after kidney transplantation. Am J Transplant. 2011;11:1645-9.
- [Google Scholar]







