Translate this page into:
Warfarin related acute kidney injury: A case report
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Warfarin is an oral anticoagulant used extensively in clinical practice; However, its side-effect of causing renal damage has been recently detected. The mechanism leading to renal damage is glomerular hemorrhage and red blood cell tubular casts prothrombin time. Recently, it was found that warfarin causes renal damage in patients with chronic kidney disease and is also associated with progression of renal disease. Warfarin causing acute kidney injury in patients with normal renal function is a rare manifestation. It is important to be aware of this condition as its innocuous presence can lead to chronic kidney disease if not corrected in time. Further studies have also found that novel oral anticoagulants such as dabigatran also cause a similar syndrome and hence a new term called anticoagulant-related nephropathy is now in vogue.
Keywords
Acute kidney injury
anticoagulant-related nephropathy
warfarin
warfarin-related nephropathy
Introduction
Warfarin is an oral vitamin K antagonist, which inhibits γ-carboxylation of clotting factors II, VII, IX, and X. It is one of the most widely used drugs for treating and preventing thromboembolism. Although very cheap and effective, warfarin use is potentially complicated by bleeding manifestations and over-anticoagulation. Warfarin is mainly metabolized by CYP-2CP microsomal liver enzymes, which is affected by a multitude of different environmental factors, diet, drug interactions, and genetics, especially CYP2 complex mutations which can alter the pharmacokinetics and pharmacodynamics of warfarin metabolism leading to toxicity and prolonged international normalized ratio (INR).[1] The prothrombin time, standardized as the INR, is used to monitor warfarin anticoagulation. Warfarin-related nephropathy (WRN) is a recently reported clinical entity, secondary to a prolonged INR.[2] It can occur in patients with or without chronic kidney disease (CKD) and is associated with progression of CKD leading to a poor outcome.[3] Further studies also found that novel oral anticoagulants such as dabigatran also caused a similar syndrome and hence the term anticoagulant-related nephropathy is now used.[4]
Case Report
A 33-year-old male, recently de-inducted from a high altitude area with no known prior comorbidities, was admitted to our center with breathlessness, dry cough, hemoptysis, and left-sided pleuritic chest pain of sudden onset. Physical examination revealed tachypnea, tachycardia, and normal blood pressure. On systemic examination, the chest was clear and there were no cardiovascular localizing signs. His initial evaluation revealed normal hematological and biochemical parameters. The serum creatinine at admission was 0.9 mg/dl (normal range - 0.8–1.1 mg/dl), blood urea was 20 mg/dl (normal range - 20–40 mg/dl), and urine examination was normal. Chest X-ray, 2D echocardiography, and Doppler scan of lower limbs and pelvic vessels were normal. Electrocardiogram showed sinus tachycardia. Renal ultrasound demonstrated normal-sized kidneys with preserved cortical thickness and no obstruction. A computed tomography pulmonary angiogram revealed acute pulmonary thromboembolism in the descending branch of the left pulmonary artery and the 2nd order branch medial basal and superior segment of the right descending pulmonary artery (modified Well's score - 4). A serological workup including antineutrophil antibody, ds DNA, complement C3/C4 levels, antineutrophil cytoplasmic antibody, and procoagulant studies was essentially normal. He was thrombolyzed with recombinant tissue plasminogen activator and thereafter started on low molecular weight heparin and bridged onto warfarin. On day 22 of the warfarin therapy, he again developed increasing left-sided chest pain and hematuria. Repeat imaging revealed no fresh embolism. His INR was 5.3 and his serum creatinine had also progressively risen to 2.6 mg/dl. His urine routine examination revealed albumin of 2+, with numerous red blood cells (RBCs) and a 24 h urinary protein of 2292 mg/day. He however was nonoliguric. A pre- and post-renal cause for acute kidney injury (AKI) was excluded, and a thorough drug history was also not contributory toward a cause for suspicion of acute interstitial nephritis. A provisional diagnosis of WRN was made. His warfarin was withheld and the coagulation parameters corrected with adequate blood component support. Over the next few days, his azotemia showed a settling trend. As the INR normalized, a renal biopsy was done which showed the modest matrix expansion associated with vascular hyalinosis, glomerular congestion with RBCs [Figure 1], and diffuse tubular damage with large and occlusive RBC casts in the tubules associated with interstitial hemosiderin laden macrophages suggestive of interstitial hemorrhage [Figure 2]. Immunofluorescence studies were negative.

- A congested glomerulus with red blood cells in the capillary vessels. The glomerular architecture is maintained other than mild vascular hyalinosis (H and E, ×40)
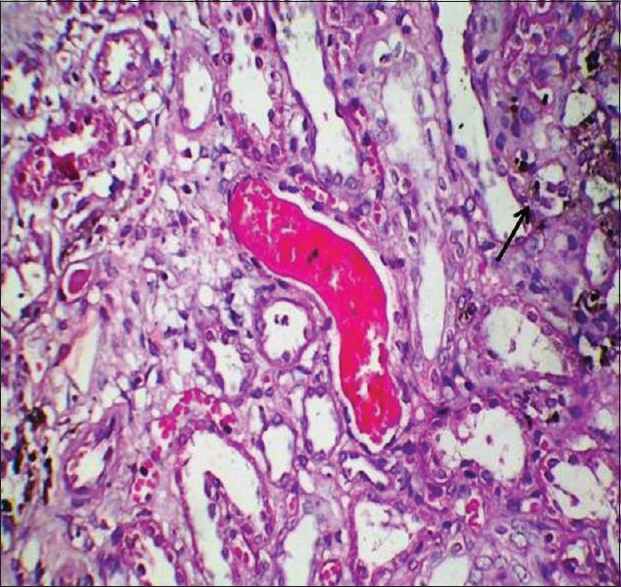
- Extensive and diffuse tubular damage. Also seen are large occlusive red blood cell casts in the tubular lumina. The interstitium shows focal areas of hemosiderin-laden macrophages suggestive of interstitial hemorrhage (arrow) PAS stain (×40)
The patient was restarted on warfarin in escalating doses till a therapeutic INR was attained. At present, his renal functions have settled back to normal.
Discussion
Warfarin can cause nephropathy by several mechanisms, namely acute interstitial nephritis, atheroembolism, direct mesangial damage, and the recently described WRN. WRN is defined as an acute increase in serum creatinine of >0.3 mg/dl within 1 week of an INR >3.0.[5] The cause of renal damage is glomerular hemorrhage and tubular RBC casts causing obstruction and inflammatory and oxidative damage to the tubular epithelial cells. Warfarin is mainly metabolized by CYP-2CP microsomal liver enzymes, which is affected by a multitude of different environmental factors, diet, drug interactions, and genetics, especially CYP2 complex mutations which can alter the pharmacokinetics and pharmacodynamics of warfarin metabolism leading to toxicity and increase in the INR. In the pioneering study by Brodsky et al., WRN developed in 37.0% of patients with CKD, who had an INR >3 and 20.5% of patients without CKD.[6] There was no correlation between the INR increase and the rise in serum creatinine and the mean INR at which it occurred was around 4.[6] The major mechanisms for WRN are glomerular hemorrhage and tubular dysfunction by obstruction due to RBC casts. Hematuria is not a consistent feature but can occur in 50% of patients.[7] Subnephrotic proteinuria is common, but its extent has not been studied. Awareness of WRN is important because the subtle renal impairment can lead to long-term kidney damage and reduced GFR as seen in the study by Brodsky SV et al., where an episode of WRN-accelerated progression of CKD studied. Studies revealed that this entity is also caused by other oral anticoagulants; hence, the new term anticoagulant-related nephropathy.[8] We suggest that WRN should always be considered a possible cause of AKI occurring during episodes of over-anticoagulation and hence monitor the INR meticulously.[9] It is usually a clinical diagnosis as biopsy is difficult due to the risk of bleeding; however, a transvenous renal biopsy can be attempted in cases where it is felt obligatory by the treating nephrologist to rule out or confirm a diagnosis.
Conclusion
WRN in patients with normal renal functions is very rare. Early detection and timely intervention can go a long way in preventing renal damage leading to chronic kidney disease.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Dicoumarol: A drug which hits at least two very different targets in Vitamin K metabolism. Curr Drug Targets 2015 [Epub ahead of print]
- [Google Scholar]
- Warfarin-related nephropathy: Another newly recognized complication of an old drug. Kidney Int. 2011;80:131-3.
- [Google Scholar]
- Warfarin therapy that results in an International Normalization Ratio above the therapeutic range is associated with accelerated progression of chronic kidney disease. Nephron Clin Pract. 2010;115:c142-6.
- [Google Scholar]
- Warfarin-related nephropathy is the tip of the iceberg: Direct thrombin inhibitor dabigatran induces glomerular hemorrhage with acute kidney injury in rats. Nephrol Dial Transplant. 2014;29:2228-34.
- [Google Scholar]
- Warfarin-related nephropathy occurs in patients with and without chronic kidney disease and is associated with an increased mortality rate. Kidney Int. 2011;80:181-9.
- [Google Scholar]
- Acute kidney injury during warfarin therapy associated with obstructive tubular red blood cell casts: A report of 9 cases. Am J Kidney Dis. 2009;54:1121-6.
- [Google Scholar]
- Warfarin-related nephropathy modeled by nephron reduction and excessive anticoagulation. J Am Soc Nephrol. 2011;22:1856-62.
- [Google Scholar]
- Anticoagulation in chronic kidney disease patients-the practical aspects. Clin Kidney J. 2014;7:442-9.
- [Google Scholar]







