Translate this page into:
Clinicopathological Spectrum of Glomerular Diseases in Adolescents: A Single-center Experience over 4 Years
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The spectrum of biopsy-proven glomerular disease was studied from a single center in Northwestern India, among adolescents aged 13–19 years. From January 2009 to December 2012, a total of 177 patients with biopsy-proven glomerular disease were studied. The same pathologist reported all the biopsy specimens after subjecting to light, immunofluorescence, and electron microscopy. The clinical profile and laboratory findings of the patients were correlated with the histopathological spectrum of glomerular diseases. Males formed 71.19% (n = 126) and the remaining 28.81% (n = 51) were females. Lupus nephritis had a strong female predominance, whereas minimal change disease (MCD) and focal segmental glomerulosclerosis (FSGS) had a male predominance. Nephrotic syndrome was the indication for biopsy in 65% of the cases. Rapidly progressive renal failure and acute nephritis were the next common indications accounting for 14% and 7%, respectively. FSGS was the most common glomerular disease in adolescents (n = 45, 25.4%). The next common were MCD and lupus nephritis each contributing 21.6% and 10.7%, respectively. Primary glomerular diseases accounted for 84.75% (n = 150) of the total. The remaining 15.25% (n = 27) were attributed to secondary glomerular diseases, of which lupus nephritis was the most common, i.e., in 70.4% patients (n = 19). FSGS was the most common histology in adolescent nephrotic participants (37%). MCD was the next common, found in 31% of nephrotic patients. Electron microscopy changed the diagnosis made by light microscopy and immunofluorescence in 5.6% cases only, and it confirmed the diagnosis in another 21.6%. Kidney biopsy in adolescents is a safe procedure. The spectrum of glomerular diseases in adolescents is different from that seen in adults and smaller children.
Keywords
adolescence
c1q nephropathy
C3 glomerulonephritis
electron microscopy
IgM nephropathy
kidney biopsy
Introduction
Glomerular disorders have histologic patterns and etiologies that vary according to the age group that is being analyzed. As age advances, the proportion of primary glomerular disorders decrease and disorders secondary to systemic diseases begin to rise. Deranged structure and function of glomeruli forms the pathophysiologic basis of these disorders.
Adolescents with glomerular disease commonly present as nephrotic syndrome (NS). The adolescent NS can be a continuation of a childhood-onset disease or may have its beginning in adolescence. There are some striking differences between glomerular diseases in adolescent and pediatric age group. The overall incidence of NS is less in adolescents as compared to children, but biopsy studies in adolescent NS have frequently reported more serious forms of glomerular disease (i.e., membranoproliferative glomerulonephritis [MPGN], membranous glomerulonephritis [MGN], and focal segmental glomerulosclerosis [FSGS]), higher frequency of hematuria, and a greater proportion of steroid-resistant NS.[12] The only biopsy series in adolescents with NS from India showed FSGS to be the most common histologic lesion.[1] This study by Gulati et al. looked at data from adolescents with NS alone. However, the literature on the entire spectrum of glomerular diseases in adolescent age group, especially from India, is scanty; hence, the present study was undertaken.
Materials and Methods
The study was undertaken in the Departments of Nephrology and Histopathology, Postgraduate Institute of Medical Education and Research, Chandigarh, over a period of 4 years, from January 2009 to January 2013 (From January 2009 to January 2011 data was retrospectively collected and from January 2011 till 2013 prospective data collection was undertaken) after approval by the Institute Ethical Committee.
Adolescents (defined as 13–19 years of age) with symptoms suggestive of glomerular disorder were subjected to a detailed history, physical examination. The clinical profile and all relevant hematological, biochemical, urine analyses and radiological investigations of adolescents with renal biopsy showing evidence of glomerular disease based on light microscopy, immunofluorescence, and electron microscopy were included in the study. Patients with incomplete clinical or investigation data, transplant kidney biopsy, and inadequate biopsies (<10 glomeruli on light microscopy) were excluded from the study. Incomplete biopsy reports, which lacked either one or more of the following, light/electron/immunofluorescence microscopy was also excluded from the study.
Patients were classified as having one of the following syndromes: NS, nephritic syndrome, rapidly progressive glomerulonephritis/rapidly progressive renal failure (RPRF), chronic glomerulonephritis (CGN), and asymptomatic urinary abnormalities. Descriptive statistics were used, and results were expressed as percentages, frequencies, mean ± standard deviation, and median. All statistical analyses were done using SPSS (Statistical Package for Social Sciences) for windows version 16 (SPSS Inc., Chicago, IL, USA). Hypothesis testing was done using Chi-square (or Fisher exact) test, P< 0.05 was considered significant.
Results
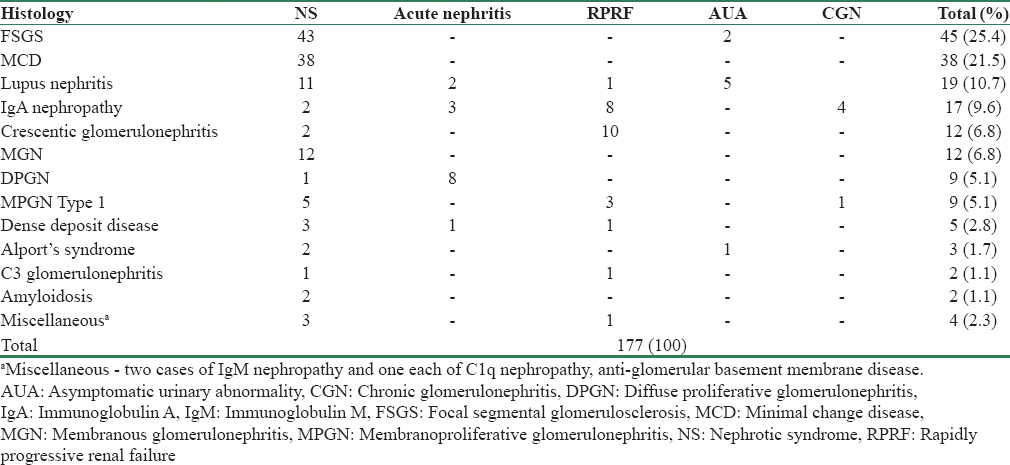
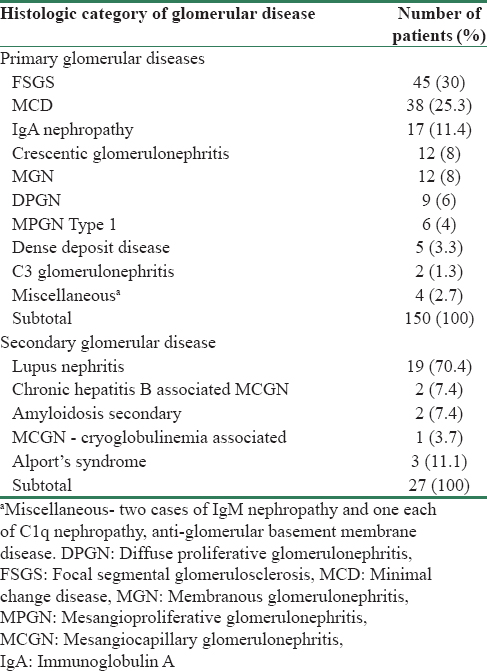
A total of 177 patients aged 13–19 years met our inclusion criteria and were analyzed. The mean age in our study was 16.2 ± 1.9 years (range, 13–19 years). The study included 126 (71.9%) male and 51 (28.1%) female patients. The most common histologic diagnosis among adolescents was FSGS, seen in 45 patients (25.4%), followed by minimal change disease (MCD) in 38 patients (21.6%), lupus nephritis in 19 cases (10.7%), and immunoglobulin A (IgA) nephropathy in 17 patients (9.6%) [Table 1]. Crescentic glomerulonephritis and MGN accounted for 12 patients each (6.8%). Diffuse proliferative glomerulonephritis (DPGN) and MPGN Type 1 were found in nine patients each (5.1%). Other miscellaneous causes (2.3%) constituted 2 patients of IgM nephropathy, one each of C1q nephropathy and anti-glomerular basement membrane disease.
Although males were more in absolute numbers, significant sexual predilection was observed only in three diseases, namely, lupus nephritis, MCD, and FSGS. In all other glomerular diseases, the differences in number of male and female patients were not statistically significant. A very strong female predisposition was noted in lupus nephritis (male:female ratio, 1:8.5). MCD (male:female, 6.6:1) and FSGS (male:female, 5.4:1), on the other hand, were more common in males than females [Figure 1].

- The proportion of male and female patients in each histological category. Absolute numbers of male and female in each category are given in the accompanying table.P values are also shown. DPGN: Diffuse proliferative glomerulonephritis, FSGS: Focal segmental glomerulosclerosis, IgA: Immunoglobulin A nephropathy, MCD: Minimal change disease, MGN: Membranous glomerulonephritis, MPGN: Membranoproliferative glomerulonephritis
There were three patients with Alport's syndrome and all of them were male. Only one among them had a positive family history along with abnormal vision and hearing. The diagnosis of Alport's syndrome in the other two patients was made on electron microscopy during evaluation for steroid-resistant NS.
Clinical presentation
The most common clinical presentation was NS, which was seen in 125 patients (71%), followed by RPRF in 25 (14%), acute nephritic syndrome in 14 (8%), asymptomatic urinary abnormality in 8 (4%), and CGN in 5 (3%) cases.
Among NS patients with renal insufficiency, MCD was present in 4 patients (19%) as opposed to FSGS in 12 patients (47%). However, none of the histologic pattern showed a significant association with renal insufficiency. More importantly, three out of four patients of MCD with renal insufficiency had either acute tubular necrosis (66%) or acute interstitial nephritis (34%) that explained the renal insufficiency.
Primary and secondary glomerular diseases
Primary and secondary glomerular diseases were found in 150 (84.75%) and 27 patients (15.25%), respectively [Table 2]. Three patients diagnosed with FSGS had family history of NS and/or end-stage renal disease (ESRD). Lupus nephritis was the most common secondary glomerular disease seen in 19 patients (70.4%). The most common histologic pattern observed was Class IV seen in nine patients (47.3%) followed by Class V in four cases (21.1%). Renal insufficiency was noted in 4 (21.1%) patients with lupus nephritis. Renal insufficiency in lupus nephritis was associated with male gender, presence of hypertension, and Class IV lupus nephritis on histology, though these differences were not statistically significant. A summary of distribution of various histologic patterns according to the clinical presentation is provided in Table 1.
Eight patients underwent renal biopsy for asymptomatic urinary abnormalities. Among the eight, 5 (62.5%) were patients diagnosed with systemic lupus erythematosus (SLE) (based on autoantibody profile and systemic features) who were being evaluated for active urinary sediments. These patients had systemic features suggestive of SLE, but lacked symptoms such as edema or hematuria. FSGS was diagnosed in a patient with asymptomatic urinary abnormality and family history of renal transplantation in two of his first-degree relatives for end-stage kidney disease (12.5%). Perihilar FSGS in a young hypertensive with proteinuria and Alport's syndrome in a male with reduced hearing were the other histologic diagnosis in this group of asymptomatic patients (12.5% each).
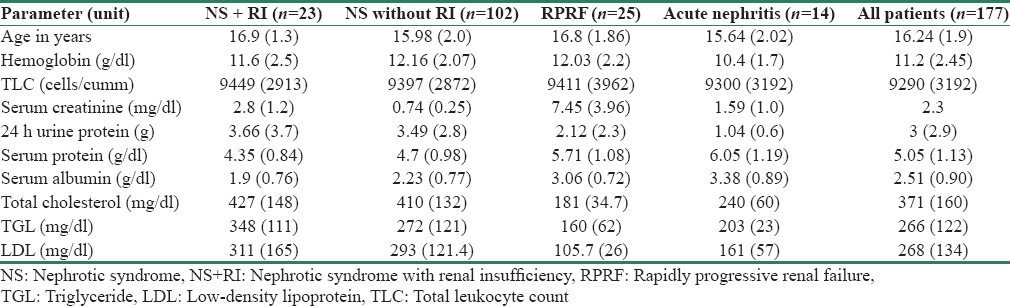
A comparison of laboratory parameters among various clinical presentations is enumerated in Table 3. The mean serum creatinine value was the highest in adolescents presenting as RPRF followed by subset of NS cases with renal insufficiency. The serum protein and albumin levels were lowest in patients with NS. Electron microscopy changed the diagnosis obtained by light microscopy in ten patients (5.6%) [Table 4]. It played a role in diagnosing basement membrane diseases and in characterizing immune complexes.

Discussion
Adolescents as a group are different from adults and children. This holds true in glomerular diseases as well. Data about glomerular diseases in adolescents are virtually absent, unlike in children and adults. To the best of our knowledge, this is the first study describing the clinicopathologic features of all kinds of glomerular diseases in the adolescent age group.
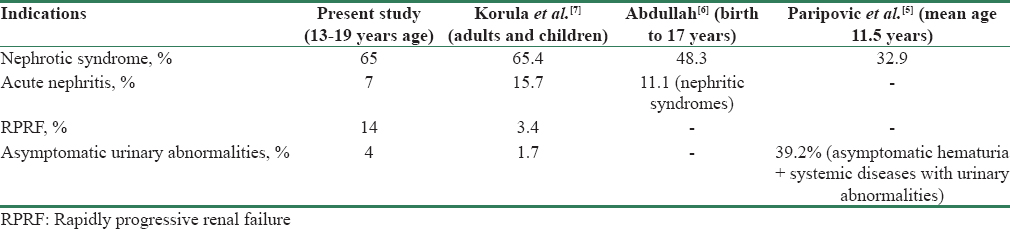
The most common indication for biopsy in our series was NS. It was the most common indication for biopsy in most other series as well, with the percentage ranging anywhere between 60% and 83% in adults from Morocco and Saudi Arabia, respectively.[34] The next common indication was RPRF, followed by acute nephritis in 14% and 8% patients, respectively. Table 5 provides the comparison of indications for biopsy in our study to similar studies done in pediatric patients[56] and adults.[7] NS was the most common indication of kidney biopsy across different age groups. However, RPRF accounted for only 3.4% of the cases in the study from Vellore,[7] whereas it was the second most common indication for biopsy in our series accounting for 14%. Gulati et al. analyzed NS in patients aged 1–18 years and tried to identify differences between patients <12 and >12 years of age. MCD was the most common cause of NS among children <12 years of age (42.9%), and FSGS was the most common cause (46.3%) in those >12 years. In our series which is comparable to the >12-year group of the above study, FSGS was the most common histologic pattern both among nephrotics (37%) as well as in the entire spectrum of glomerular diseases (25.4%). FSGS as a separate clinicopathological entity arose in 1970s, after a report published by International Study of Kidney Diseases in Children[8] and is now the most common cause of NS in adults as well.
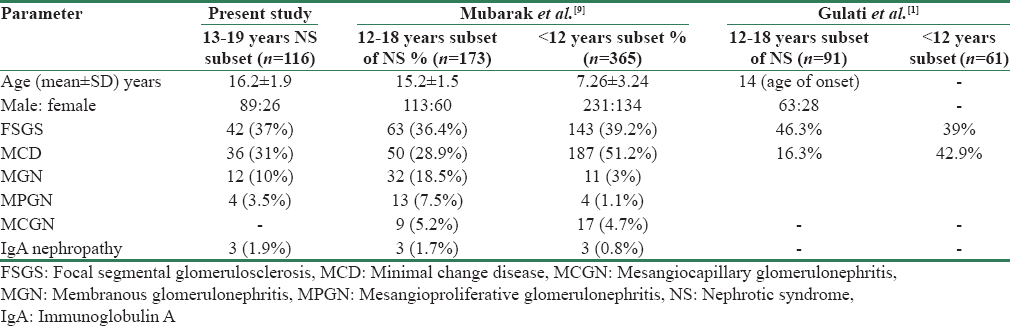
MCD accounted for 21.6% of all glomerular diseases and 31% of NS in our series of adolescent glomerular diseases. Mubarak et al. noted MCD in 51% of NS in <12 years and only 28.9% in adolescents, a finding which is similar to ours.[9] This reduction in MCD and increase in FSGS as age increases have been noted in other studies as well.[7] A trend towards change in histologic spectrum in adults with NS has also been observed recently.[10] The pathology of glomerular diseases differs between adolescents and children.[911] In Table 6, we have compared the subset of NS patients in our study with the studies from Karachi[9] and Lucknow.[1] FSGS was the most common cause of adolescent NS in all three studies. In contrast to these data from India and Pakistan, Hogg et al. noted a different scenario in a study of 65 adolescent nephrotic patients from Dallas in 1993.[12] MCD was the most common histologic diagnosis, accounting for 53%, whereas FSGS and MGN each were present in 18.5% of the adolescents with NS. It is unclear whether the above difference in prevalence is due to the geographical and racial differences or the changing pattern of diseases over time.[71112]
MGN was previously the most common cause of glomerular disease in adults. However, recently FSGS has surpassed MGN.[13] In adults, secondary causes[13] including drugs, malignancies, hepatitis B, and hepatitis C virus infection account for up to 25% of the MGN cases. Adolescents with MGN in our series, however, lacked evidence for these secondary causes.
Acute nephritic picture was present in 7% of the adolescents with glomerular disease. National registry of Italy[14] noted that acute nephritic syndrome was present in 4.4% of their children undergoing biopsy. IgA nephropathy was the most common cause in their series,[14] whereas DPGN was the most common in our adolescent population. Higher percentage of DPGN in the current series may be explained by increased incidence of infection-associated glomerulonephritis in India.
Primary glomerular disease still forms the major proportion in adults, but the proportion of secondary diseases is more than what is observed in children and adolescents.[15] Secondary glomerular diseases accounted for 15.25% in our series, of which lupus nephritis was the most common (70.4%). A Korean study of 1818 adults with glomerular diseases had 11.8% with secondary glomerular diseases, and the most common cause of secondary disease was lupus nephritis forming 8.7% of the secondary causes.[16] A high degree of suspicion is needed to identify and treat this condition, as a significant proportion of these patients are asymptomatic and may have proteinuria on evaluation. Progression to ESRD is well known in the absence of treatment.[17] Similar to our series, a recent study of lupus nephritis from Spain also noted that renal failure was more common in lupus patients with male gender, hypertension, proteinuria, histology showing Class III or IV, and advancing age.[18]
Electron microscopy was employed in all the patients included in the study. It had modified the diagnosis in only 6% and aided the diagnosis of MCD in 21% of cases. Contribution of electron microscopy for diagnosis was reported in a study to be 31%, which is comparable to our data (27%).[19] Electron microscopy can answer diagnostic dilemmas and pave way for better diagnosis.
Conclusion
Adolescents with glomerular disease present commonly as NS and FSGS is the most common cause. Adolescents form a distinct group, and data are grossly inadequate. It is high time; a national kidney biopsy registry is established. By establishing a common registry, uniform form of reporting would be possible. Apart from maintaining a uniform record, it can give information about geographical differences and changes in trend over time.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Spectrum of adolescent-onset nephrotic syndrome in Indian children. Pediatr Nephrol. 2001;16:1045-8.
- [Google Scholar]
- Time trends and ethnic patterns of childhood nephrotic syndrome in Yorkshire, UK. Pediatr Nephrol. 2001;16:1040-4.
- [Google Scholar]
- Glomerular diseases in the Military Hospital of Morocco: Review of a single centre renal biopsy database on adults. Indian J Nephrol. 2012;22:257-63.
- [Google Scholar]
- Percutaneous renal biopsy and its findings in children and adolescents in saudi arabia: A single center experience. Saudi J Kidney Dis Transpl. 1997;8:289-93.
- [Google Scholar]
- Indications and results of renal biopsy in children: A 10-year review from a single center in Serbia. J Nephrol. 2012;25:1054-9.
- [Google Scholar]
- Histopathological pattern of pediatric renal diseases: A study from a university hospital in western Saudi Arabia. Saudi J Kidney Dis Transpl. 2012;23:377-84.
- [Google Scholar]
- Spectrum of biopsy proven renal disease and changing trends at a tropical tertiary care centre 1990-2001. Indian J Nephrol. 2003;13:29-35.
- [Google Scholar]
- Pathology of the nephrotic syndrome in children: A report for the International Study of Kidney Disease in Children. Lancet. 1970;760:1299-302.
- [Google Scholar]
- Pathology of idiopathic nephrotic syndrome in children: Are the adolescents different from young children? Nephrol Dial Transplant. 2012;27:722-6.
- [Google Scholar]
- Changing etiologies of unexplained adult nephrotic syndrome: A comparison of renal biopsy findings from 1976-1979 and 1995-1997. Am J Kidney Dis. 1997;30:621-31.
- [Google Scholar]
- The paucity of minimal change disease in adolescents with primary nephrotic syndrome. Pediatr Nephrol. 1998;12:105-7.
- [Google Scholar]
- Glomerular lesions in adolescents with gross hematuria or the nephrotic syndrome. Report of the Southwest Pediatric Nephrology Study Group. Pediatr Nephrol. 1993;7:27-31.
- [Google Scholar]
- Frequency of renal diseases and clinical indications for renal biopsy in children (Report of the Italian National Registry of Renal Biopsies in Children). Group of Renal Immunopathology of the Italian Society of Pediatric Nephrology and Group of Renal Immunopathology of the Italian Society of Nephrology. Nephrol Dial Transplant. 1998;13:293-7.
- [Google Scholar]
- The spectrum of glomerular diseases in a single center: A clinicopathological correlation. Indian J Nephrol. 2013;23:168-75.
- [Google Scholar]
- Changing prevalence of glomerular diseases in Korean adults: A review of 20 years of experience. Nephrol Dial Transplant. 2009;24:2406-10.
- [Google Scholar]
- Review: Lupus nephritis: Pathologic features, epidemiology and a guide to therapeutic decisions. Lupus. 2010;19:557-74.
- [Google Scholar]
- Risk factors for renal failure in patients with lupus nephritis: Data from the spanish registry of glomerulonephritis. Nephron Extra. 2012;2:269-77.
- [Google Scholar]
- Current position of electron microscopy in the diagnosis of glomerular diseases. Pol J Pathol. 2007;58:87-92.
- [Google Scholar]







