Translate this page into:
Colonic Ulcerations in a Patient on Hemodialysis
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Platelet dysfunction, the use of heparin and antiplatelets increase the risk of gastrointestinal (GI) bleeding in chronic kidney disease (CKD) patients on dialysis.[1] We report an unusual cause of GI bleeding in a patient on hemodialysis.
A 66-year-old female, a known case of type 2 diabetes mellitus, hypertension, ischemic heart disease, and CKD presented to us with a history of fall 2 weeks back. During this fall, she sustained an injury to her back and left hand. Her evaluation revealed a normotensive afebrile woman with pedal edema and swelling in the left forearm. Her initial investigations [Table 1] revealed the presence of severe renal failure, mild hypocalcemia, severe hyperphosphatemia, normal Vitamin D, and elevated serum parathormone levels. Her radiological investigations revealed a fracture of the left distal radius and 12th thoracic vertebral fracture for which she underwent surgery. She was initiated on hemodialysis through a right internal jugular catheter, and for her hyperphosphatemia, she was started on sevelamer carbonate 800 mg three times a day with food.
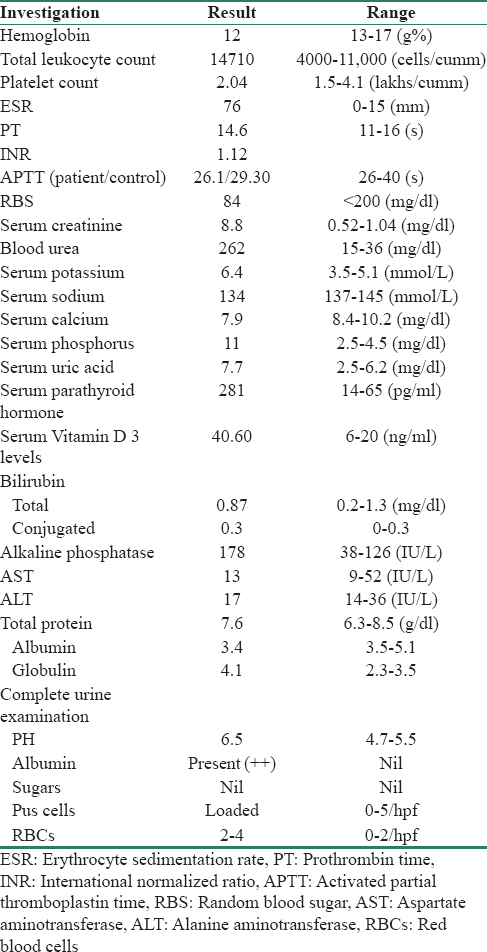
On the 5th postoperative day, she had melena with a significant drop in hemoglobin (12.0 g/dl to 8.6 g/dl). There was no history of abdominal pain vomiting or constipation. Her bleeding parameters were normal. An upper GI endoscopy showed mild gastric erosions. Her aspirin and clopidogrel were stopped. Next day, she had large quantity of maroon colored rectal bleed with further drop in hemoglobin (6.5 g/dl). A colonoscopy this time showed an ileocecal valve ulcer with active ooze. There were multiple erosions all over the colon. Colonic biopsies were taken and the active ulcer was photocoagulated. She received blood transfusions during dialysis. Her GI bleeding settled subsequently. At discharge, her hemoglobin was 9.8 g/dl.
Her colonic biopsy report came as extensive mucosal ulceration with areas of the organization and crystalloid structures [Figure 1]. These rusty yellow colored crystals had slightly curved fish scale structure suggestive of sevelamer crystals. Her clinical and laboratory investigations for common causes of GI bleeding (infective, inflammatory, and neoplastic) were noncontributory. It was felt that sevelamer carbonate was responsible for the GI bleeding aggravated by the concomitant use of antiplatelet medications. Sevelamer carbonate was withdrawn, and calcium acetate was started. At discharge she is stable, and there was no recurrence of bleeding even after the reinstitution of aspirin and clopidogrel.
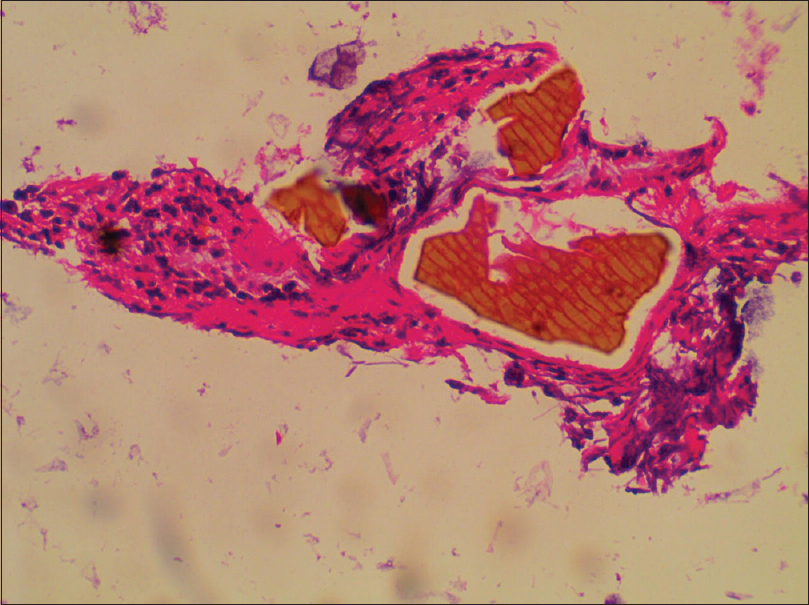
- Sevelamer crystals embedded in the colonic mucosa
Recently, the use sevelamer carbonate is implicated in various gastrointestinal symptoms in CKD patients.[2] GI bleeding secondary to the tablet has been reported in association with stercoral ulcerations[3] and in patients without constipation also.[45]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Upper gastrointestinal bleeding in patients with CKD. Clin J Am Soc Nephrol. 2014;9:1354-9.
- [Google Scholar]
- Update and critical appraisal of sevelamer in the management of chronic renal failure. Open Access J Urol. 2010;2:161-70.
- [Google Scholar]
- Lower gastrointestinal bleeding: Association with sevelamer use. World J Gastroenterol. 2008;14:2615-6.
- [Google Scholar]
- Hematochezia associated with sevalamer-induced mucosal injury. ACG Case Rep J. 2014;1:145-7.
- [Google Scholar]
- A case report of sevelamer-associated recto-sigmoid ulcers. BMC Gastroenterol. 2016;16:20.
- [Google Scholar]






