Translate this page into:
Partially Reversible Acute Renal Cortical Necrosis Secondary to Hyperhomocysteinemia – A Case Report and Literature Review
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Acute renal cortical necrosis (ACN) is a potentially fatal renal condition. Our objective is to report a case of ACN in a young man who had developed premature atherosclerotic vascular disease and required intermittent hemodialysis support. His renal biopsy showed diffuse cortical necrosis. Subsequently, 2 weeks after the renal insult, he developed a cardioembolic stroke and was anticoagulated with low-molecular-weight heparin. Thrombophilia screen revealed elevated serum homocystein and he was treated with folate supplement and vitamin B12 injection. With these treatments, he had partial renal recovery and became dialysis independent. In conclusion, this is a rare case of ACN, which may have occurred as a complication of hyperhomocysteinemia.
Keywords
Acute cortical necrosis
acute kidney injury
hyperhomocysteinemia
Introduction
Acute cortical necrosis (ACN) is an uncommon manifestation of acute kidney injury with its frequency ranging from 1.9% in western countries to 7% in developing countries.[12] It is commonly caused by obstetric complications in 50–70% of the cases. Non-obstetric causes accounts for 20–30% of the cases[34] and it is usually due to extensive burns, sepsis, pancreatitis, diabetic ketoacidosis, hemolytic uremic syndrome, and snake bite.[56]
Case History
A 30-year-old Indian gentleman presented to the emergency department complaining of left loin pain for 3 days. It was associated with persistent vomiting for 2 days. Otherwise, he denied dysuria, oliguria, hematuria, and fever. He had a previous history of angina at the age of 21 years, which was due to coronary artery vasospasm with normal coronary angiogram and echocardiogram finding of ejection fraction (EF) 49% with mild septal hypokinesia. On examination, he was alert, mildly dehydrated, with blood pressure (BP) 152/95 mm Hg, heart rate (HR) 60 bpm, and temperature 37°C. Abdominal examination revealed tenderness over left lower quadrant with positive renal punch over left side. Complete blood count showed hemoglobin 15.3 g/dl, total white cell 17.3 × 109, and platelet 169 × 109. Initially serum biochemistry results were urea 50 mg/dl, Na 137 meq/L, K 4.8 meq/L, creatinine 4.6 mg/dl, creatine kinase 945 U/L (30–200), alanine transaminase 103 U/L, aspartate transaminase 155 U/L, albumin 4.0 g%. lactate dehydrogenase (LDH) was 1921 U/L (125–220). Urinalysis revealed protein 3+, blood 1+, leukocyte, nitrite, and urine myoglobin was negative. Findings of renal ultrasonography, abdominal radiography, chest radiography, and non-contrast computed tomography–urography were unremarkable.
While in the ward, he remained clinically well, afebrile, with a good urine output and persistent hypertension. His liver enzymes and creatine kinase normalized in the ward. However, his renal function continued to deteriorate and he became dialysis dependent despite supportive care (peak urea 140 mg/dl and creatinine 10.8 mg/dl). A renal biopsy was performed on day 6 of admission. Light microscopy showed extensive ischemic necrosis involving the glomeruli, tubules, interstitium, and blood vessels affecting 90–100% of the cortex. The minimal non-necrotic tubules and interstitium showed acute tubular injury and interstitial nephritis without evidence of thrombosis [Figures 1 and 2]. His renal profile remained static after three cycles of intermittent hemodialysis and he was discharged with urea of 122mg/dl and creatinine 10 mg/dl.

- An abrupt transition between the area of cortical necrosis and the viable region (H and E, original magnification ×10)
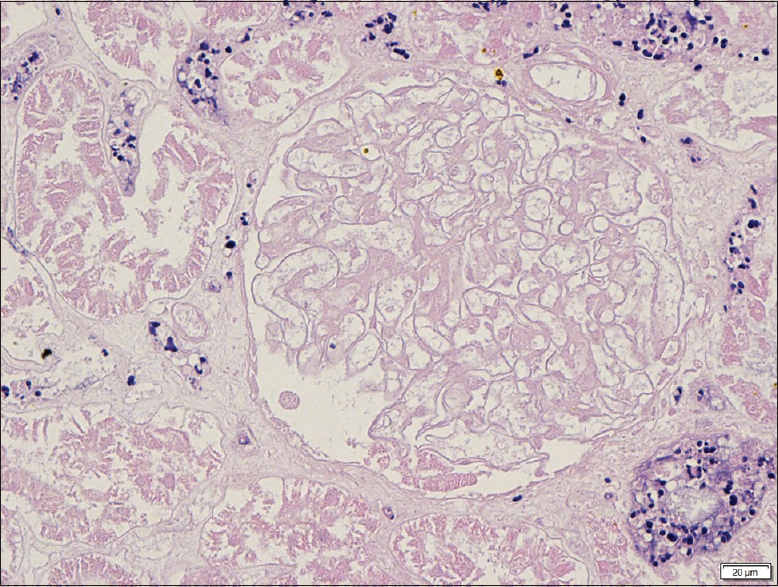
- Diffuse area of cortical coagulative necrosis of glomeruli and tubules. Arterioles show no evidence of thrombus or vasculitis. (H and E, original magnification ×40)
Two weeks post discharge, he presented to the emergency department for sudden onset of cerebellar signs. Computer tomography scan of the brain found left cerebellum acute infarct. At the same time an echocardiogram was performed and he was found to have an apical thrombus measuring 1.9–2 cm, with poor left ventricle systolic function (EF 36%). He also had complaint of intermittent claudication of the lower limbs. However, he had good urine output and had no symptoms of uremia and fluid overload. Subsequently immunology screen: antinuclear antibody (ANA), anti-cardiolipin, lupus anticoagulant, p-ANCA and c-ANCA were normal. Thrombophilia screen protein C, protein S, and antithrombin 3 were normal as well. Further blood test revealed elevated serum homocystein of 3.79 mg/L (normal range 0.68 – 1.8). Due to the cost and limited resources, we were unable to send urine for homocystein. He was anticoagulated with enoxaparin 60 mg BD and started with S/C vitamin B12 1 mg injection and folic acid as the treatment for hyperhomocystenemia. There was a partial renal recovery in this patient whereby his creatinine decreased to 3.8 mg/dl after 2 months from initial insult.
Discussion
Renal cortical necrosis is a condition leading to irreversible kidney injury. It results from severe reduction in the renal artery perfusion due to vascular spasm and microvascular injury. A retrospective study in India had found that most of the patients with ACN were critically ill patients, where 61% of them died during the course of the hospital stay.[7]
In this paper we describe an otherwise healthy young man who came in with the presentation of left loin pain and vomiting for 3 days. Infection and obstructive uropathy was ruled out by an urgent renal ultrasound and urinalysis. A similar case was described in a healthy 18-year-old girl who was diagnosed with acute unilateral ACN following skipping rope. She too presented with the right flank pain and vomiting, with leukocytosis, raised liver enzymes, and LDH. She was mistakenly diagnosed with appendicitis and was subjected to an explorative laparotomy.[8] Though rare, these two cases showed that acute ACN could present as a disguise to an acute abdomen in an otherwise healthy young patient.
ACN is characterized histologically into diffuse or patchy cortical necrosis. Diffuse type is more common with incidence ranging from 62.8–80% according to a few Indian studies.[234567] From previous data, we understood that the diffuse pattern inevitably leads to the progression of end-stage renal disease.[9] This case is rather peculiar as compared to previous studies of ACN. First of all, as compared to the common presentation of anuria in patients with ACN, this patient did not have anuria. In fact, he had stable vital signs and had a very good urine output of at least 1 cc/kg/h. Secondly, his renal biopsy findings are consistent of diffuse cortical necrosis involving 90–100% of the cortex. However, he had a partial but meaningful renal recovery and he was able to wean off dialysis. His initial estimated glomerular filtration rate (eGFR) was 9.8 mL/min, which improved to 30 mL/min after 2 months from the initial insult.
This patient had developed premature atherosclerotic vascular disease as well as thromboembolic events as evidence of stroke, peripheral vascular disease, and ischemic heart disease with cardiac thrombus. With the immunology and thrombophilia screen being negative, we attribute it to the diagnosis of hyperhomocysteinemia. Hyperhomocysteinemia may be due to genetic causes e.g., deficiency of enzyme cystathionine B-synthase, which convert homocysteine to cystathionine and acquired causes such as folate/vitamin B12, B6 deficiency, and renal insufficiency.[10] Hyperhomocysteinemia is known to be an independent risk factor for premature vascular disease including cerebrovascular disease, peripheral vascular disease, and coronary vascular disease when a cut-off homocysteine level of 3.2 mg/L was used.[11] Other studies have shown that even mild hyperhomocysteinemia (2.02–4.0 mg/L) may have similar clinical consequences.[1213] Homocysteine is toxic to vascular endothelium and can promote thrombosis,[1415] hence theoretically it could also cause microvascular renal injury leading to ACN. In conclusion, we have presented case of ACN in a young and fit patient as a complication of hyperhomocysteinemia with favorable partial renal recovery. A high index of suspicion with early renal biopsy is the key to the diagnosis and timely management of this rare condition.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Spectrum of renal cortical necrosis in acute renal failure in eastern India. Postgrand Med J. 1995;71:208-10.
- [Google Scholar]
- Acute cortical necrosis: Case report and review of the literature. Am J Med. 1974;56:110-8.
- [Google Scholar]
- Diagnostic procedures and long term progress in bilateral cortical necrosis. Kidney Int. 1973;4:390-400.
- [Google Scholar]
- Prolonged oliguria with survival in acute bilateral cortical necrosis. BMJ. 1968;4:220-2.
- [Google Scholar]
- Unilateral acute renal cortical necrosis (ACN) following skipping with a rope. Nephrol Dial Transplant. 2000;15:415-8.
- [Google Scholar]
- Changing picture of renal cortical necrosis in acute kidney injury in developing country. World J Nephrol. 2015;4:480-6.
- [Google Scholar]
- Homocysteine and venous thromboembolism—Is there any link.? Cor Et Vasa. 2013;55:e248-58.
- [Google Scholar]
- Hyperhomocysteinemia: An independent risk factor for vascular disease. N Engl J Med. 1991;324:1149-55.
- [Google Scholar]
- Facts and recommendations about total homocysteine determinations: An expert opinion. Clin Chem. 2004;50:3-32.
- [Google Scholar]
- Consequences of moderate hyperhomocysteinemia ininternal medicine. Casopislekaruceskych. 2004;143:367-74.
- [Google Scholar]
- Homocystine induced arteriosclerosis: The role of endothelial cell injury and platelet response in its genesis. J Clin Invest. 1976;58:731-41.
- [Google Scholar]
- Homocysteine-induced endothelial cell injury in vitro: A model for the study of vascular injury. Thromb Res. 1980;18:113-21.
- [Google Scholar]







