Translate this page into:
Effect of Distal Cephalic Vein Ligation on Primary Patency Rates and Proximal Flow Rates in Distal Radiocephalic Fistula
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
The Brescia-Cimino radiocephalic fistula, originally devised as a side-to-side anastomosis, is simple to perform and provides a smooth vein–artery interface but requires greater mobilization for vein–artery approximation than does the end-to-side approach. Distal cephalic vein ligation is performed to prevent venous hypertension. The study aims to assess primary patency at one month following distal side-to-side radiocephalic fistula creation with and without distal cephalic vein ligation, to assess the effect of distal cephalic vein ligation on flow rates at one month, and to document the occurrence of venous hypertension over one year follow up.
Method:
A total of 100 patients requiring vascular access for hemodialysis were assigned to side-to-side anastomosis with and without distal cephalic vein ligation. Follow up Doppler exam was performed at one month for assessment of patency and flow rates and after one year clinical exam to document venous hypertension and the need for revision surgery. The quantitative and qualitative variables were evaluated using student t test and chi square test, respectively.
Results:
The patency rates of distal ligation and no ligation groups were 86.4% and 85.4%, respectively. The proximal flow rates of distal ligation and no ligation groups were 1192+/−812 ml/min and 1217+/−796 ml/min, respectively. The difference was not statistically significant (P > 0.05). Only two cases (5%) with no ligation required revision ligation within one year of surgery.
Conclusion:
Distal cephalic vein ligation does not increase the proximal cephalic flow rates and primary patency rates after one month. However, venous hypertension was associated in 5% of nonligated cases at one year follow up.
Keywords
Brescia Cimino fistula
fistula flow rate
fistula patency
Introduction
The autogenous Brescia–Cimino distal radiocephalic arteriovenous fistula is the gold standard for vascular access among chronic hemodialysis patients. This provides the best access for longevity and is associated with lowest morbidity and mortality. According to the guidelines of National Kidney Foundation (NKF-K/DOQI), it is the primary site for surgical access for hemodialysis.
The initial paper by Brescia–Cimino in 1966 described a side-to-side radiocephalic anastomosis.[1] The side-to-side technique is technically simple and produces a uniform wall shear stress profile reducing the neointimal hyperplasia.[2] This reduces the development of juxta-anastomotic stenosis which is one of the key causes of primary fistula failure. Although the end-to-side technique is most prevalent and reduces the risk of venous hypertension, it requires greater technical skill. It also has inherent complications like necessity of vein mobilization resulting in stripping of adventitia and stenosis, matching of arteriotomy to vein angulation, endothelial cell damage from vein clamping and vein torque.[3]
The aim of this study was to study the effect of distal cephalic vein ligation in distal radiocephalic fistulae constructed using side-to-side anastomosis, on the primary patency rates and proximal flow rates at one month follow up, and to assess the occurrence of venous hypertension at one year.
Materials and Methods
A total of 100 patients were included in this study and organized into two groups of 50 each by random number table method. These patients were referred by nephrologists to a tertiary referral hospital for creation of peripheral vascular access for hemodialysis over a two-year period, 2015–2017. The study was approved by the institutional ethics committee. All surgeries were performed by the author himself.
Patient identification, contact data, and referral pathology were documented. The patient comorbidities such as diabetes mellitus, ischemic heart disease, peripheral vascular disease, and hypertension were noted. The dominance of arm, previous fistula surgery, hemodialysis cycles, and venipuncture of identified vein, and the presence of features of subclavian stenosis, arterial steal, atherosclerosis, venous stenosis, and lymphatic edema were examined. The clinical examination was performed to evaluate for engorged arm veins, trophic ulcers, or signs of Raynaud's phenomenon. Any history of arm swelling, numbness or coldness of hand, and weakness on exertion were also recorded. The Allen's test was conducted to identify a patent palmar arch and adequacy of ulnar artery flow. The cephalic vein was examined under tourniquet and a continuous segment of subcutaneous vein at least 15 cm in length was also marked.
Preoperative Doppler examination using 7 MHz probe identified the diameter of cephalic vein and radial artery at elbow and wrist and the peak systolic velocity of the radial artery. Atherosclerosis of radial artery and thrombosis and stenosis of cephalic vein were documented.
Inclusion criteria for the study were:
Minimum cephalic vein diameter of 2 mm with tourniquet, with no proximal thrombosis or stenosis,
No history of cephalic venipuncture in last six weeks
Radial artery codominant on Allen's test with palpable radial pulse at wrist
No signs of subclavian stenosis, venous insufficiency or arterial steal, or ischemia.
Exclusion criteria were:
Ipsilateral subclavian vein cannulation for dialysis
Pulmonary edema with orthopnoea preventing surgery under local anesthesia
Coagulopathy and Hypotension
Significant continuous atherosclerosis of radial artery in forearm
Cephalic vein thrombosis in proximal forearm.
Investigations included renal parameters specifically creatinine levels, bleeding time, clotting time, and hemoglobin levels. Blood pressure and pulse were recorded and pulmonary decompensation with dyspnea was ruled out. Hemodialysis was performed on the day prior to surgery if required and patients were operated with a minimum systolic BP of 100 mm Hg.
Under local anesthesia, a curvilinear incision on the dorsoradial wrist exposed the cephalic vein and a 5-cm segment was isolated by dividing the tributaries. The vein was not denuded but vasa vasora and adventititia were trimmed for a 10-mm length for venotomy. Vein flow was confirmed by milking test using jewellers' forceps. Valve segments were avoided and branch stumps were included in the venotomy as far as possible to avoid thrombogenic foci.
The radial artery was isolated and a nonatheromatous segment of 1 cm was freed of adventitia and venae comitantes. The two vessels were approximated by silicon loops. Instead of clamping the vessels, silicon loop noose ties were used. An 8–10 mm venotomy and arteriotomy were done and the lumina were flushed with heparinized saline (50 IU/ml). The proximal vein was cannulated and flushed with heparinized saline to confirm flow.
A backwall first anastomosis technique was performed, using double needle 6-0 prolene. In all no ligation cases, the distal cephalic vein had a palpable thrill only up to the first distal valve with no extension onto the dorsum of hand [Figures 1 and 2].

- Side-to-side distal radiocephalic fistula with no ligation of distal venous arm

- Side-to-side distal radiocephalic fistula with ligation of distal venous arm
On table proximal thrill was confirmed in all cases and closure was done after achieving hemostasis and keeping the anastomosis in a lignocaine wash for 5 minutes to relieve arterial spasm and observe for anastomotic bleeders. Patients were discharged after 24 hours observation and confirming patent fistula by palpable thrill. At 10 days postoperative, sutures were removed and any complications like hematoma, dehiscence, or local infection were documented and treated. At one month postoperative, a Doppler examination was done to see:
The diameter of the cephalic vein 10 cm proximal to anastomosis
The peak systolic velocity of blood flow through the cephalic vein 10 cm proximal to anastomosis
The presence of any pseudoaneurysm, thrombosis, or stenosis.
Primary patency was defined as:
Clinical palpation of a thrill over the fistula and auscultation of a machinery murmur
Color Doppler showing arterial flow through the fistula with no thrombosis or vein stenosis.
Primary failure was defined as failure of the fistula to demonstrate the above findings at the one month examination. These cases were offered redo fistula surgery due to nonavailability of endovascular or interventional radiology facilities.
Successful patients were referred back to the treating nephrologist after confirming the maturation of fistula. Criteria for mature fistula were:
Fistula flow rate of >500 ml/minute calculated as Q = V × A × 60 where Q; flow in ml/min, V: peak systolic velocity cm/sec, A: cross-sectional area of vein in cm2
Vein diameter of >4 mm at least 10 cm proximal to anastomosis allowing two needle dialysis
Straight segment of cephalic vein located <5 mm below skin surface allowing cannulation [Figure 3].

- Functional fistula with no distal ligation at one year followup with no venous hypertension changes
During dialysis, 16 and 17 G needles were used and the flow rates used were 180–250 ml/min.
At one year, the patients were called up for review of fistula functionality and presence of any complication. Venous hypertension was identified as the inability to flex the thumb or fingers due to swelling, venous ulcers, or presence of dilated veins on dorsum of hand. These patients were offered distal vein ligation under local anesthesia.
The data gathered was entered in a proforma and reviewed after the study period for statistical analysis. Quantitative and qualitative data were expressed in means and percentages, respectively, and analyzed using Student T test and Pearson Chi square test using Statistical package for Social Sciences ver. 25. The quantitative data were assessed using Levene's test for equality of variances for independent samples test with 95% Confidence Interval.
Results
A total of 100 patients fulfilling the inclusion criteria were allotted into two groups of 50 each with group A undergoing distal ligation and group B undergoing no ligation. The randomization resulted in matching for age, gender, comorbidities, and patient characteristics as shown in Table 1. The preoperative Doppler findings between the two groups did not have significant statistical difference (P > 0.05).
| Parameter | Distal ligation—Group A | No ligation—Group B | ||
|---|---|---|---|---|
| Male | 39 | 39 | ||
| Female | 11 | 11 | ||
| Average age (years) | 51.7 (+/−13.2) | 51.7 (+/−13) | ||
| Previous dialysis | 4.9 (+/−7) | 4.1 (+/−7.3) | ||
| Nondominant arm | 43 | 47 | ||
| Diabetes | 23 | 28 | ||
| Smoking | 8 | 12 | ||
| Hypertension | 41 | 45 | ||
| Doppler finding | Group A | Group B | ||
| Mean | SD | Mean | SD | |
| Preoperative cephalic vein diameter (mm) | 2.6 | 0.7 | 2.5 | 0.8 |
| Preoperative radial artery PSV (cm/s) | 62.7 | 24.4 | 56.4 | 21.8 |
| Preoperative radial artery diameter (mm) | 2.2 | 0.4 | 2.3 | 0.5 |
The patients were followed up after surgery at 10 days, one month, and one year. Out of 100, 85 patients attended the one-month Doppler and one year follow-up [Figure 4].
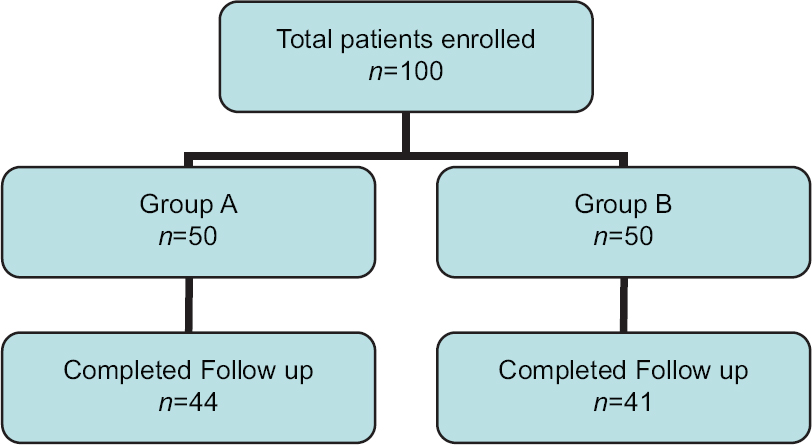
- Patient allotment and followup flowchart
The postoperative period was assessed for early fistula bleed, hematoma below skin flap and skin necrosis causing dehiscence. The Doppler at one month documented that fistula failure was caused either by thrombus formation or vein stenosis as shown in Table 2. A total of five cases of stenosis were due to juxta-anastomotic stenosis and one case was due to proximal cephalic vein stenosis. No cases of pseudo aneurysm were identified.
| Parameter | Group A | Group B |
|---|---|---|
| Patency (primary success/total follow up) | 38/44 (86.4%) | 35/41 (85.4%) |
| Maturity (functional fistula/total follow up) | 34/44 (77.3%) | 33/41 (80.5%) |
| Venous hypertension at one year | 0 | 2/41 (5%) |
| Complication | Group A | Group B |
| Hematoma | 2 | 2 |
| Bleed | 1 | 1 |
| Skin necrosis | 1 | 1 |
| Thrombosis | 3 | 3 |
| Stenosis | 3 | 3 |
The results of one-month postop Doppler were analyzed as fistula patency, peak systolic velocity in vein, and increase in diameter of cephalic vein and flow rates in proximal cephalic vein as shown in Table 3. Venous hypertension was noted at one-year follow up in 2/41 cases (5%) of the no ligation group. The difference between mean flow rates achieved between Groups A and B, shown in Table 3, were not statistically significant on student T test (P > 0.05). The patency rates of Groups A and B were 86.4% and 85.4%, respectively. The difference is not statistically significant.
| Parameter | Group A | Group B | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Flow rate (ml/min) | 1192 | 812 | 1217 | 796 |
| Peak velocity (cm/sec) | 136 | 85 | 123 | 64 |
| Inc in diameter (mm) | 1.49 | 1.1 | 1.96 | 1.2 |
| Postoperative cephalic vein diameter (mm) | 4.2 | 1.1 | 4.3 | 0.8 |
The difference in preoperative cephalic vein diameter was not statistically significant between Groups A and B. However, the increase in diameter of cephalic vein at one month Doppler was 1.96+/−1.2 mm for nonligation group and 1.49+/−1.1 mm for ligation group. A statistically insignificant difference was observed in unpaired student T test (P = 0.085).
Among all the documented risk factors, female gender had the highest incidence of failure with a failure percentage of 31.6%. The fistula patency rate showed no significant correlation with gender (P = 0.801), diabetes mellitus (P = 0.401), history of smoking (P = 0.257), hypertension (P = 0.255), ischemic heart disease (P = 0.605), previous hemodialysis (P = 0.132), and use of nondominant arm (P = 0.702). No incidence of failure was associated with peripheral vascular disease.
Discussion
Hemodialysis, initially performed for young adults with acute and reversible renal failure, has now become routine for end-stage renal. Brescia et al. performed the first internal arteriovenous fistula for hemodialysis access in 1966.[1] The Brescia–Cimino radiocephalic fistula is the most suitable method of access in developing countries, thus avoiding the costs and risks of graft infections with indwelling shunts.[4] According to the NKF-DOQI guidelines, the site order for the surgical intervention of AVF for HD is the following: Forearm (radiocephalic or distal AVF), elbow (brachiocephalic or proximal AVF), arm (brachiobasilic with transposition or proximal AVF).[5]
Distal radiocephalic fistulae are associated with lower patency rates than the proximal brachiocephalic fistulae. Hong[6]et al. observed a patency rate of 96% for the first month, 93% for the first year, and 90% for the second year for the radiocephalic AVF (side-to-side anastomosis with distal vein ligation and division) at the wrist. Rooijens[7] recorded high primary failure rate for distal radiocephalic fistulae, either because of early thrombosis or failure to mature. The pooled primary patency rate at one year for retrospective as well as prospective studies analyzed by Rooijens was 62.5%. Rooijens defined primary patency as the interval from the time of RCAVF creation until any intervention designed to maintain or re-establish patency, fistula thrombosis, or the time of measurement of patency. Primary failure was defined as fistula thrombosis or failure to mature resulting in inadequate functioning for hemodialysis at 6 weeks. Manne et al.[8], while analyzing the factors influencing the patency of Brescia–Cimino fistulae, observed a primary patency rate of 84.8%. They identified vessels of small caliber and damage to the vessel wall due to frequent venipunctures, complicated by poor flow due to hypotension as the factors causing early thrombosis in fistulae.
In our study, we observed a patency rate of 86.4% in Group A and 85.4% in Group, thus giving a cumulative patency rate of 85.9% at one month. This correlates well with the work of Manne et al. The primary failure was caused in six cases by thrombosis and six cases by vein stenosis. We did not use heparin as anticoagulation for thromboprophylaxis and only continued aspirin in prophylactic dosing to prevent vein thrombosis.
Males as subjects for fistula surgery in our study accounted for 78% of the enrolled cases. Of the 19 female cases that completed one-month assessment, we had six failures resulting in a high (31.6%) failure rate compared to males who had six failures out of 66 completed follow up cases (9.1%). However, due to the smaller number of female cases studied, this result was not statistically significant. The study by Monroy-Cuadros et al. reported no significant association between gender and AVF failure[9] after adjusting for age, hypertension, diabetes mellitus, peripheral vascular disease, smoking history, and the type of procedure.
A study by Dixon et al.[10] reported that 65–100% of angiographically evaluated fistulas failed due to vein stenosis. More than 50% of vein stenosis is just downstream of the fistula or involving the anastomosis (juxtaanastomotic). In our series, of the six cases of stenosis, five were due to juxtaanastomotic stenosis, and one due to proximal cephalic stenosis. As the technique of anastomosis was similar, no significant difference can be attributed between the two groups.
Other causes of failure are impaired arterial and venous dilation and presence of accessory veins. Failure of arterial dilation is due to structural or functional causes. Structurally, increased intima-media thickness has been correlated with fistula failure.[11] Endothelial dysfunction is associated with impaired release of nitric oxide. The early rapid phase of arterial dilation is likely mediated by smooth muscle relaxation in response to endothelial release of nitric oxide.[12] In our study, preoperative Doppler identified presence of atherosclerosis and an extensile incision allowed us to place the fistula in a nonatheromatous segment of radial artery.
Venous hypertension can occur as a complication of side–to-side arteriovenous fistula, with technical fault resulting in stenosis of the central discharge vein, proximal to the site of the anastomosis, thus causing blood flow into the peripheral vein. This causes filling of the veins of the distal upper extremity with hand and digit edema, limited mobility, and livid discoloration progressing to venous gangrene.[13] In our study, we confirmed preoperative patency of cephalic vein clinically under tourniquet and by Doppler examination at wrist, mid forearm, and elbow levels. In six cases of vein stenosis at one month Doppler, five were juxtaanastomotic and one was central combined with thrombosis of the fistula. In the six cases of thrombosis, thrombus involved the fistula and the vein proximally and distally. All cases were primary fistula failures and were offered redo fistula on the other hand. The two cases of venous hypertension were associated with unsightly veins on the thumb and painful flexion of thumb and were treated by ligation of the distal vein, before they could progress to venous insufficiency.
The retrograde flow[14] from the distal artery occurs in about 75% of forearm fistulas and accounts for an average of 25% of blood flow into the venous limb of the fistula. Corpataux et al.,[15] analyzing Brescia-Cimino fistulas, found that increased venous pressure accounts for the rapid early vein dilation, while subsequent venous dilation over weeks is to normalize the flow-induced increase in wall shear stress. We postulate that reverse flow in the distal limb of cephalic vein may increase venous pressure and maintain flow in the proximal venous limb of the fistula. We identified distal thrill in the cephalic vein upto the first distal valve only, in all cases with no ligation, and only two of these cases progressed to thumb swelling and pain requiring distal vein ligation after one year. We postulate that maintaining the distal continuity may allow filling of the cephalic vein upto the first distal valve, allowing increased vein pressures to act on the proximal vein and enabling vein dilation. The average increase in cephalic vein diameter in our study was 1.96+/−1.2 mm for no ligation group versus 1.49+/−1.1 mm for distal ligation group. This was tending to statistical significance (P = 0.085) but did not fulfill 95% confidence interval limits due to paucity of study subjects. The further study of increase in diameter and its correlation with flow rates at six months and one-year duration in a larger cohort with no distal vein ligation would clarify this point and provide a reason to preserve the distal continuity of the cephalic vein.
The distal radiocephalic fistula allows the use of proximal veins in forearm for dialysis and preserves the future fistula options for the chronic hemodialysis patient. The side-to-side fistula is a time-tested simple anastomotic technique, which can be routinely employed for radiocephalic anastomosis as they can be easily approximated. Ligation of the distal cephalic vein has been routinely done to prevent venous hypertension, however in our follow up we had a small incidence of this complication. In nonligated patients, we documented an improvement in proximal vein dilation.
Owing to poor patient follow-up at one year for imaging studies, we were unable to objectively analyze one-year flow rates and vein diameters. Patency at one year was assessed subjectively by a single operator and objective data would be preferable. Further data for solute clearance (urea reduction ratio) would provide objective result-oriented dialysis outcomes.
In conclusion, we have identified no difference in the flow rates and primary patency with or without distal vein ligation at one month postoperative. We thus postulate that distal radiocephalic side-to-side fistula may be performed without per primum distal vein ligation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Chronic hemodialysis using venipuncture and a surgically created arteriovenous fistula. NEngl J Med. 1966;275:1089-92.
- [Google Scholar]
- Arteriovenous fistulas constructed using side to side anastomosis with ligation and division of distal venous arm; a tertiary care hospital experience. J Vasc Access. 2010;11:26-30.
- [Google Scholar]
- Angio access for hemodialysis in renal failure: An analysis of the role of the Brescia –Cimino fistula. MJAFI. 1999;55:310-2.
- [Google Scholar]
- National Kidney Foundation, Inc. 2001. K/DOQI Guidelines – Updates 2006. New York: National Kidney Foundation, Inc; Available from: http://www.kidney.org/PROFESSIONALS/kdoqi/guideline_upHD_PD_VA/index.htm
- [Google Scholar]
- Clinical analysis of radiocephalic fistula using side-to-side anastomosis with distal cephalic vein ligation. Korean J Thorac Cardiovasc Surg. 2013;46:439-43.
- [Google Scholar]
- Radiocephalic wrist arteriovenous fistula for hemodialysis: Metaanalysis indicates a high primary failure rate. Eur J Vasc Endovasc Surg. 2004;28:583-9.
- [Google Scholar]
- Factors influencing patency of brescia-cimino arteriovenous fistulas in hemodialysis patients. Saudi J Kidney Dis Transpl. 2017;28:313-7.
- [Google Scholar]
- Risk factors associated with patency loss of hemodialysis vascular access within 6 months. Clin J Am Soc Nephrol. 2010;5:1787-92.
- [Google Scholar]
- The impact of intima-media thickness of radial artery on early failure of radiocephalic arteriovenous fistula in hemodialysis patients. J Korean Med Sci. 2006;21:284-9.
- [Google Scholar]
- Arterial expansive remodeling induced by high flow rates. Am J Physiol. 1997;272:H851-8.
- [Google Scholar]
- Peripheral venous hypertension after the creation of arteriovenous fistula for hemodialysis. Biomed Papers. 2004;148:85-7.
- [Google Scholar]
- Characterizing flow distributions in AV fistulae for haemodialysis access. Nephrol Dial Transplant. 1998;13:3108-10.
- [Google Scholar]
- Low-pressure environment and remodelling of the forearm vein in Brescia-Cimino haemodialysis access. Nephrol Dial Transplant. 2002;17:1057-62.
- [Google Scholar]







