Translate this page into:
Is Twice-weekly Maintenance Hemodialysis Justified?
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
The benefits of twice-weekly dialysis at initiation are significant with respect to access longevity, preservation of residual renal function, economic factors, and patient quality of life. It is widely practiced in developing countries due to resource and financial constraints. We present a 3-year follow-up of patients on twice-weekly dialysis and their outcomes.
Material and Methods:
This was a 3-year observational follow-up study of patients initiated on twice-weekly hemodialysis. Adequacy and basic cost-effective hematological and biochemical parameters were studied monthly. In case of complications, the patient was shifted to thrice-weekly hemodialysis.
Results:
88 incident hemodialysis patients were followed up. Total sessions of hemodialysis (HD) studied were 16,406. The mean hemoglobin level was 9.53 g/dl with hyperphosphatemia in 74.88% patients. The mean residual renal function (RRF) at initiation was 5.71 +/- 3.70 ml/min. The mean interdialytic weight gain was 1.91 +/- 1.26 kg with a mean ultrafiltration of 2600 ± 410 ml. The spKt/V and eKt/V were adequate in 68.54% and 48.34% patients; however, the standard Kt/V of 2 was achieved in only 10.51% patients. Emergency HD was done in 41 sessions (0.24%). There were 24 deaths (27.27%) during this period with the mean time to mortality being 503.12 +/- 296.62 days.
Conclusion:
Initiation at twice-weekly schedules for patients on maintenance hemodialysis is a viable option with increments in case of requirement, more so in patients with good urine output and residual renal function. The biochemical and hematological parameters were stable and within KDOQI guidelines and do not worsen with time.
Keywords
Adequacy of dialysis
residual renal function
survival
twice-weekly hemodialysis
Introduction
Developing countries have limited resources and a formidable load of patients requiring dialysis. In a country like India with 17% of the world population, the majority do not have access to basic healthcare facilities.[12] At some point in clinical practice, most nephrologists question the concept of thrice-weekly hemodialysis at initiation. The primary goal of healthcare initiatives is to provide quality care and concurrently rationalize costs. In underdeveloped nations, nephrologists are well versed with the concept of twice-weekly hemodialysis, which is an unspoken accepted norm. Thrice-weekly hemodialysis was a concept introduced three decades ago and requires consideration in the present-day scenario of sophisticated dialysis machines, advanced dialysis membranes, and ultrapure water.[34] Twice-weekly maintenance hemodialysis is not an accepted form of renal replacement therapy (RRT) primarily because there are not enough studies to prove its sustainability. However, with the concept of incremental dialysis and residual renal function (RRF) gaining ground, this can prove to be a good option for initiation of hemodialysis. We report here, a 3-year follow-up of patients on twice-weekly dialysis and their outcomes.
Material and Methods
This was a 3-year observational cohort study of patients initiated on twice-weekly hemodialysis. All the patients regardless of their RRF were initiated on twice-weekly hemodialysis. Children, pregnant women, patients being worked up for renal transplant, and patients on peritoneal dialysis were excluded from the study. Adequacy of dialysis and basic cost-effective hematological and biochemical parameters were studied monthly in each patient. In case of complications in the form of recurrent fluid overload, uncontrolled hypertension, refractory anemia, hyperphosphatemia despite being on phosphate binders, and features of malnutrition, the patient was shifted to thrice-weekly hemodialysis. Low flux polysulphone dialyzers with a surface area of 1.7 m2 were used for most patients.
The primary outcomes studied were adequacy, hematological, basic biochemical parameters, and quality of life (QoL) index. The secondary outcomes considered were number of hospitalization episodes, death from time of initiation, and the cause of morbidity and mortality.
We used the slow blood flow sampling technique[5] for analyzing post hemodialysis samples for adequacy. The spKt/V and eqKt/V were estimated from the pre and post dialysis blood urea nitrogen, post dialysis weight, and ultrafiltrate volume using the web-based calculator at http://www.davita.com/tools/ktvcalculator. Standard Kt/V was calculated from the spKt/V, average session length, and number of sessions of dialysis per week using the HDCN web calculator at http://www.hdcn.com/calcf/ley.html.
Quality of life data based on the WHO QOL questionnaire was recorded in all patients. The Institute Ethics Committee approved our study protocol (IEC BHDC/36, 06 July 2018). Patients' written informed consent was taken in a language that they understand. Single pool Kt/V was calculated with the software present in the machine, eKt/V was calculated with the Daugirdas equation,[5] and standard Kt/V was calculated using the Hypertension Dialysis and Clinical Nephrology (HDCN) web calculator.[6] Statistical analysis was done using SPSS 20 software.
Results
Over a period of 3 years, 88 incident hemodialysis patients were followed up at our center. The gender ratio was comparable with 51% males and 49% females. The mean age of the patients was 47.09 +/- 14.93 years (range 16–67). Table 1 enumerates the various causes of end-stage kidney disease. AVF was present at initiation of dialysis in 38.6% patients and 61.4% patients had no access at presentation, being initiated on dialysis with catheters [Figure 1]. This was in spite of the fact that the majority of patients were on regular follow-up, as the treatment is free and easily available. The demographic characteristics of the study population are described in Table 2. Total sessions of hemodialysis (HD) studied were 16,406 with a mean of 188.57 +/- 163 sessions. The mean time on HD during the 3-year period was 765.69 +/- 694.38 days.
| Basic disease | Frequency (n) | Percent |
|---|---|---|
| Autosomal dominant polycystic Kidney disease | 3 | 3.4 |
| Chronic glomerulonephritis | 12 | 13.6 |
| Chronic interstitial nephritis | 28 | 31.8 |
| Diabetes mellitus | 11 | 12.5 |
| Diabetes/Hypertension | 11 | 12.5 |
| Hypertension | 6 | 6.8 |
| IgA Nephropathy | 7 | 8 |
| Obstructive uropathy | 3 | 3.4 |
| Focal segmental glomerulonephritis | 3 | 3.4 |
| Cortical necrosis | 3 | 3.4 |
| Calculous renal disease | 1 | 1.1 |
| Total | 88 | 100 |
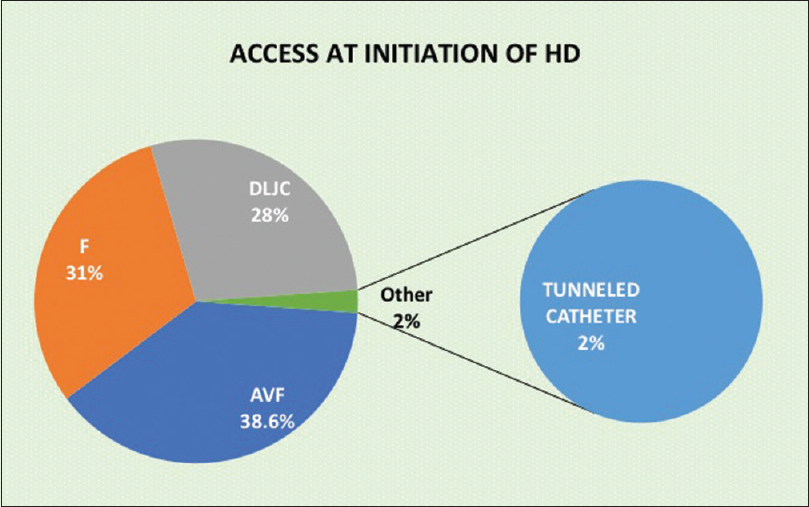
- Access at initiation of hemodialysis. Footnote: DLJC: Double lumen Jugular Catheter, AVF: Arterio venous Fistula
| VARIABLE | VALUES |
|---|---|
| Age | 47.09±14.93 years |
| Gender | Males 45 (51.10%) |
| BMI | 22.89±3.80 kg/m2 |
| Vascular Access | AVF 38.6% |
| Urine output at commencement | 979.54±454.58 ml |
| Hemoglobin | 9.53±1.66 g/dl |
| Type of anemia | Microcytic hypochromic -43.2% |
| Macrocytic- 24.3% | |
| Normocytic normochromic- 28.3% | |
| Serum albumin | 3.64±0.77 g/dl |
| Serum cholesterol | 128.88±32.06 mg/dl |
| Serum uric acid | 5.43±1.76 mg/dl |
| Calcium | 8.6±1.20 mg/dl |
| Phosphate | 6.34±1.7 mg/dl |
| Alkaline phosphatase | 121.82±103.67 IU/L |
| Residual renal function at initiation | 5.71 +/- 3.70 ml/min |
The mean hemoglobin was 9.53 ± 1.66 g/dl and 64.88% patients were anemic with a hemoglobin less than 10 g/dl. Microcytic hypochromic anemia was the commonest. Iron studies were being done every 3 months with 87.5% patients being iron replete. The mean dosage of erythropoietin was 220 units/kg/week. Macrocytic anemia was seen in 24.3% of our patients. Over a period of 3 years, the hemoglobin levels remained stable as shown in Figure 5. There was no correlation between residual renal function and hemoglobin levels.
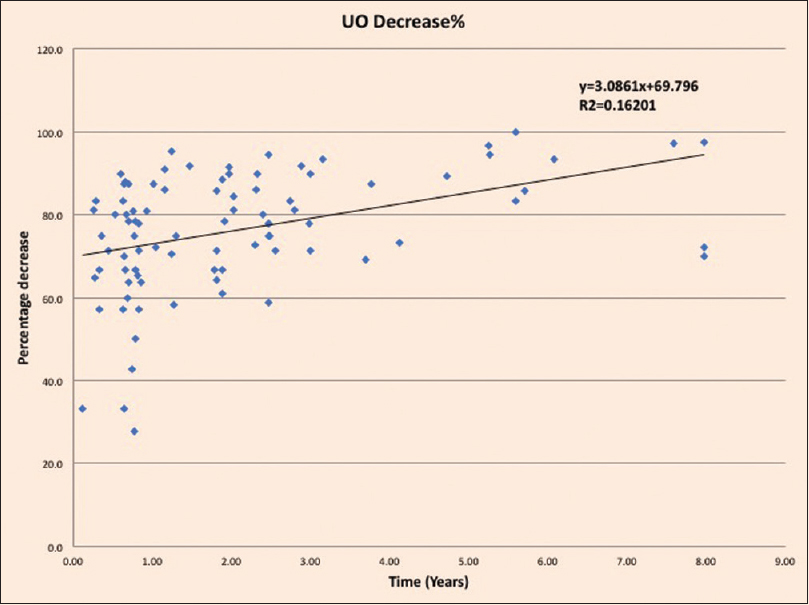
- Regression analysis showing the percentage decrease of urine output over time
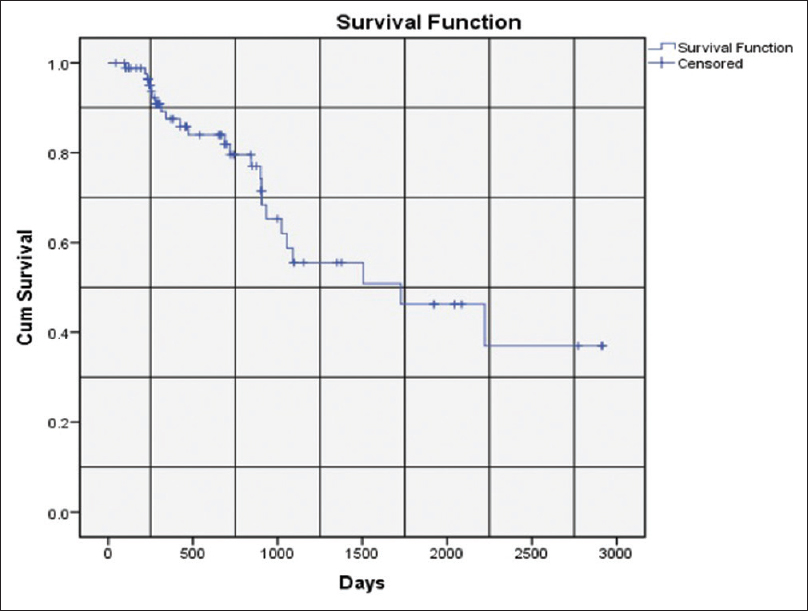
- Kaplan-Meier survival curve for 88 patients for all cause mortality
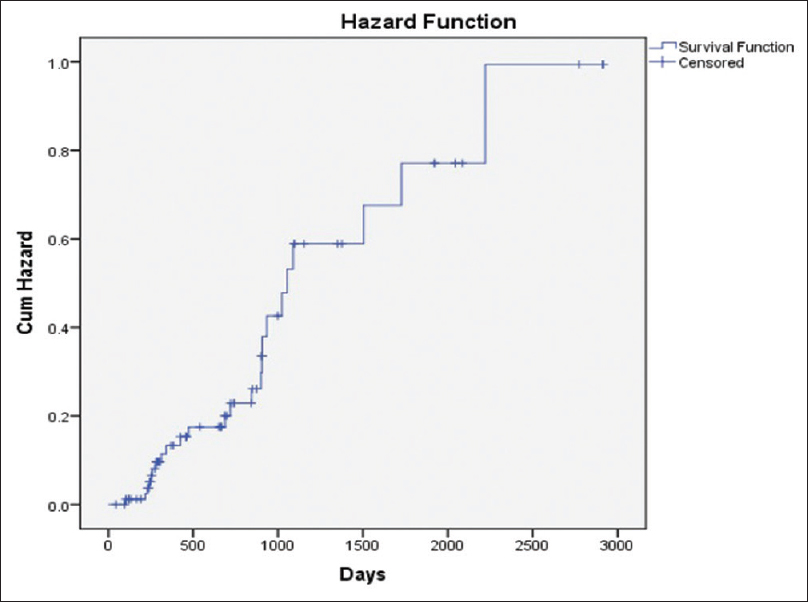
- Hazard function for all cause mortality for 88 patients on twice weekly hemodialysis
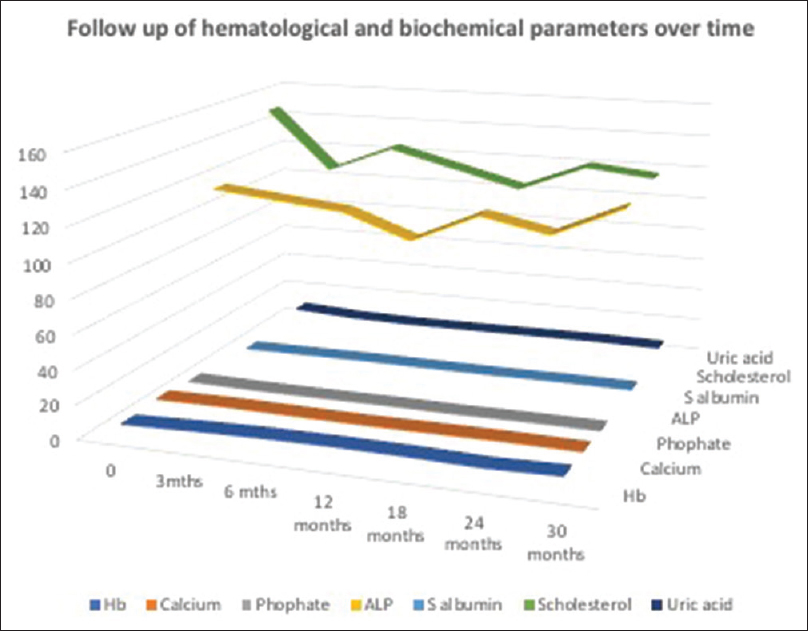
- Temporal profile of hematological and biochemical parameters over time. (X axis denotes time of follow up whereas Y axis shows that numerical value of laboratory parameters is sustained over time)
Biochemical parameters studied are described in Table 2. Hyperphosphatemia was observed in 73.86% patients. Serial follow-up of patients revealed that the biochemical parameters in the form of calcium, phosphate, and alkaline phosphatase were stable during the follow-up on dialysis [Figure 5]. The DEXA scan done revealed osteoporosis of the radius in 55.68%, spine in 42.04%, and hip in 23.86% of patients. However, there was no incidence of fracture.
Nutritional parameters measured included body mass index (BMI), serum albumin, and serum cholesterol. They were all found to be within the acceptable range over the period of follow-up as seen in Figure 5. WHO-QOL score was studied only once after 6 months on hemodialysis. The mean WHO-QOL score of 52.92 +/- 10.42 and the scores were low in all domains. The score had a negative impact with increasing time on dialysis. Younger patients had a very low score in the physical domain, while elderly patients had a uniformly low score in all domains. Socioeconomic factors played a major role in the QOL scores with patients from the higher socioeconomic strata having better scores.
Another fundamental point observed was that majority of the patients had adequate urine output at initiation of dialysis with a mean of 979.54 ± 454.58 ml. 19.31% of patients had a urine output less than 500 ml and the mean RRF at initiation was 5.71 +/- 3.70 ml/min. 18.18% patients had an RRF less than 2 ml/min at initiation of dialysis [Figure 2]. Measurement of RRF was only calculated at initiation of hemodialysis and at the end of the study. RRF had no correlation with hemoglobin levels; however, it had a negative impact on phosphate levels. Patients with higher RRF had lower hospitalization rates, better blood pressure control, and higher QOL scores.
Hypertension was present in 90.91% of patients with mean systolic BP of 153.52 mmHg and diastolic BP of 84.38 mmHg. Majority of patients (30.68%) were on two drugs, whereas 27.27% patients were prescribed one drug for hypertension. Left ventricular hypertrophy was seen in 37.2% patients with a mean ejection fraction of 56.44%. 24.3% patients had mild pulmonary hypertension though the pre and post dialysis status of 2D Echo was not assessed.
The mean duration of dialysis during the study was 220.84 +/- 26.12 min. The spKt/V and eKt/V were adequate in 68.54% and 48.34% patients; however, the standard Kt/V of 2 was achieved in only 10.51% patients [Table 3]. The mean interdialytic weight gain was 1.91 +/- 1.26 kg with a mean ultrafiltration of 2600 ± 410 ml. Emergency HD was carried out in 41 sessions (0.24%), the main cause being complications in the form of fluid overload and pulmonary edema (87.80%). There were 68 episodes of hospitalization with a rate of 0.77 hospitalizations per patient with a mean hospitalization stay of 6.8 +/- 2.1 days [Table 4].
| PARAMETERS | MEAN±SD |
|---|---|
| Interdialytic weight gain | 1.91±1.26 kg |
| Ultrafiltration | 2600±410 ml |
| Time on dialysis | 796±732.19 days |
| Urine output | 979.54±454.58 ml |
| spKT/V | 1.38±0.51 |
| eKT/V | 1.1±0.22 |
| Std KT/V | 1.57±1.21 |
| CAUSE | n(%) |
|---|---|
| Fluid overload | 36 (52.94%) |
| Hyperkalemia | 2 (2.94%) |
| CRBSI | 4 (5.88%) |
| Respiratory tract infection | 8 (11.76%) |
| Accelerated hypertension | 4 (5.88%) |
| Cerebrovascular accidents | 4 (5.88%) |
| Others | 10 (14.70%) |
During our study period, there were 24 deaths (27.27%) with the mean time to mortality being 503.12 +/- 296.62 days. Seven deaths (7.95%) occurred during the first year, whereas nine (10.22%) deaths took place in the second year [Figure 3,4]. At the end of 2 years of follow-up, 72 (81.81%) patients survived. The commonest cause of death was a cardiovascular event in 41.66% of patients [Table 5]. Six patients (6.81%) had to be shifted to thrice-weekly dialysis during this period for uncontrolled hypertension, fluid overload, refractory ascites, anemia not responding to high doses of ESA, refractory hyperphosphatemia, and malnutrition.
| CAUSE | n(%) |
|---|---|
| Cardiovascular | 10 (41.66%) |
| Cerebrovascular | 2 (8.33%) |
| Disseminated Tuberculosis | 2 (8.33%) |
| Sepsis | 8 (33.33%) |
| Others | 2 (8.33%) |
The mean distance from place of residence to the dialysis center was 30.25 kilometers with an average time of travel being 60.34 min. The mean cost to reach the dialysis center was $2.8, where the average daily wage is about $5.5.
Discussion
In our study, we found a preponderance of patients with a favorable RRF at initiation of dialysis. Twice-weekly dialysis provided acceptable adequacy in a majority of patients. The nutritional, hematological, and biochemical parameters were in an admissible range and were sustained over a period of time. The mortality rates were comparable to thrice-weekly hemodialysis.
Most nephrologists in India are well versed with the concept of twice-weekly hemodialysis to the extent that it is an unwritten norm in government hospitals. Due to an acute shortage of resources in the form of equipment, consumables, and manpower, compounded by the burgeoning number of patients who require hemodialysis, this is a survival necessity.[7] The majority of patients do not have access to basic medical facilities, whereas 90% ESKD patients do not have access to hemodialysis and succumb to their disease.[8] Out of this necessity, originated the concept of incremental dialysis.[910].
The National Cooperative Dialysis Study (NCDS) established that a thrice-weekly hemodialysis schedule provided adequate clearance of small molecules to achieve a spKt/V of 1.2.[3] This was published 30 years ago; however, with the advancement of machines and availability of better quality dialyzers and ultrapure water, the one rule for all thrice-weekly hemodialysis requires a thought.
Cross-sectional data from China under Dialysis Outcomes and Practice Patterns Study (DOPPS) found that 26% of patients in China were dialyzing twice a week. Female sex, shorter dialysis vintage, lower socioeconomic status, low health insurance coverage, and absence of diabetes and hypertension were associated with dialyzing twice a week.[11] In a study by Lin et al., RRF in patients undergoing twice-weekly dialysis had a slower decline in RRF than in those on thrice-weekly dialysis with less episodes of hospitalization rates. Results showed that the clinical outcomes in twice-weekly hemodialysis were comparable to thrice-weekly hemodialysis. Twice-weekly HD patients had significantly longer HD session time and higher single-pool Kt/V (spKt/V).[12].
Kalantar-Zadeh et al., in USA in their encouraging study, reported a slower decline in RRF over time, better access preservation, comparable survival rates, reduced cost, and better QoL scores in patients undergoing twice-weekly hemodialysis; however, there is a lack of adequate studies to strengthen the concept.[13] A number of Indian studies also focus on the importance of twice-weekly HD in our country. The study by Chauhan and Mendonca highlighted the adequacy of twice-weekly hemodialysis with increasing duration of dialysis session time and has shown comparable levels of hemoglobin, albumin, Qol scores, and results to thrice-weekly hemodialysis.[7] A retrospective analysis done by Mukherjee et al. comparing twice and thrice-weekly hemodialysis revealed better biochemical, hematological, and Qol scores in patients undergoing thrice-weekly hemodialysis; however, the morbidity and mortality were similar in both groups.[14].
Observations from our study revealed that the majority of patients of ESKD are in the age group 40–50 years, a time when the pressures of life and responsibilities are utmost. Hence, providing them with lifesaving treatment in the form of hemodialysis is an absolute requirement. Studies done in other developing countries also had patients of the same age group, thus the increasing pressure to practice twice-weekly hemodialysis to reach out to a maximum.[1011].
Vascular access is another thorn in the flesh of dialysis care providers with only 34.6% patients having an AVF despite our organization providing free, easy access guaranteed medical treatment. In a Japanese study, AVF was the vascular access for incident hemodialysis in 72.7% of patients, whereas in North America the use of AVF as the initial vascular access was 47%. In another study from Ireland, the use of AVF in incident hemodialysis patients was 39.3%.[151617].
A study from Taiwan revealed that patients on twice-weekly hemodialysis achieved adequacy in the form of spKt/v 1.19 and a Std Kt/v of 3.34 on twice-weekly hemodialysis. Over a period of 1 year, the mean hemoglobin was 11.1 g/dl, calcium and phosphorus levels were within normal limits, and the serum albumin and serum cholesterol levels were near normal.[10] Data from the Chinese arm of the Dialysis Outcomes and Practice Patterns Study (DOPPS) revealed an adequacy of spKt/V 1.19 and Standard Kt/V of 1.38. The mean hemoglobin was 10.1 g/dl and the nutritional and biochemical parameters were within acceptable range with a marginally high phosphate level.[12] Our study had similar findings with an adequate spKt/V and eKt/v. The hematological, nutritional, and biochemical parameters were within the prescribed range with slightly high phosphate levels.
The concept of adequacy based on Kt/V requires a relook. Adequacy of dialysis in the form of Kt/V is not accurate in twice-weekly hemodialysis as Kt/V is dependent on ultrafiltration which is high in these patients because of the longer gap in dialysis sessions and also lower body weight of Indian patients in comparison to the western population. It has been proved that urea as surrogate marker of small molecule clearance is fallacious. Newer small molecules like indoxyl sulphate, adenine dimethyl arginine, and MDMA levels have no correlation with urea levels and neither is there any correlation with dialysis clearance and time, thus prompting a review in the dialysis adequacy parameters.[18] Taking this into consideration, newer parameters to assess adequacy of hemodialysis in the form of Hemodialysis Product requires a thought.[19].
An interesting aspect of our study was that most patients had adequate urine output and RRF at initiation of dialysis, thus increasing the scope of twice-weekly dialysis schedules. Data from China under Dialysis Outcomes and Practice Patterns Study (DOPPS) showed that around 48% patients had significant urine output at initiation of dialysis though the RRF was not measured.[12] Another study from Taiwan revealed that more than 85% of patients had a urine output more than 500 ml at initiation of dialysis.[10] Our study demonstrated that more than 82% patients had a RRF above 2 ml/min. This is a very significant dimension because most centers do not assess the residual renal function at initiation of dialysis, the awareness of which can increase the frequency and acceptability of twice-weekly hemodialysis.
The survival rate of 81.81% at 2 years is comparable to thrice-weekly hemodialysis and in a developing country is an acceptable outcome.[20] The mortality was 7% in the first year and 9% in the second year. The commonest causes of mortality were cardiovascular diseases and sepsis, both of which are reversible and treatable. Increased weight gain and high ultrafiltration contribute to cardiovascular mortality and this was increasingly seen in patients who were anuric. Catheter-related infections and respiratory tract infections were another cause of high mortality and are potentially treatable aspects.
Socioeconomic factors are one of the principal hindrances in the provision of dialysis to ESKD patients. As our center provided free hemodialysis, this was not a major hurdle to overcome; however, the story in developing countries is different with the recurrent and high cost of dialysis which is unaffordable to majority of patient population who are not covered by insurance or government-sponsored programs.[212223].
Conclusion
The study reveals that most patients having favorable residual renal function at initiation of maintenance hemodialysis justifies a twice weekly hemodialysis schedule. It further allays the fear of inadequate dialysis dosage and adds economic benefits which is advantageous to the patient and healthcare services.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Prevalence of chronic renal failure in adults in Delhi, India. Nephrol Dial Transplant. 2005;20:1638-42.
- [Google Scholar]
- A mechanistic analysis of the national cooperative dialysis study (NCDS) Kidney Int. 1985;28:526-34.
- [Google Scholar]
- Hemodialysis (HEMO) study group: Effect of dialysis dose and membrane flux in maintenance hemodialysis. N Engl J Med. 2002;347:2010-9.
- [Google Scholar]
- Simplified equations for monitoring Kt/V, PCRn, eKt/V and ePCRn. Adv Ren Replace Ther. 1995;2:295-304.
- [Google Scholar]
- Mathematical representation of standard Kt/V including ultrafiltration and residual renal function. ASAIO J. 2018;64:e88-93.
- [Google Scholar]
- Adequacy of twice weekly hemodialysis in end stage renal disease patients at a tertiary care dialysis centre. Indian J Nephrol. 2015;25:329-33.
- [Google Scholar]
- What do we know about chronic kidney disease in India:First report of the Indian CKD registry. BMC Nephrol. 2012;13:10.
- [Google Scholar]
- Incremental dialysis: Review of recent literature. Curr Opin Nephrol Hypertens. 2017;26:543-7.
- [Google Scholar]
- Association of initial twice-weekly hemodialysis treatment with preservation of residual kidney function in ESRD patients. Am J Nephrol. 2014;40:140-50.
- [Google Scholar]
- Two-times weekly hemodialysis in China: Frequency, associated patient and treatment characteristics and Quality of Life in the China Dialysis Outcomes and Practice Patterns study. Nephrol Dial Transplant. 2014;29:1770-7.
- [Google Scholar]
- Comparison of residual renal function in patients undergoing twice-weekly versus three-times-weekly haemodialysis. Nephrology. 2009;14:59-64.
- [Google Scholar]
- Twice-weekly and incremental hemodialysis treatment for initiation of kidney replacement therapy. Am J Kidney Dis. 2014;64:181-6.
- [Google Scholar]
- A comparison of practice pattern and outcome of twice-weekly and thrice-weekly hemodialysis patients. Indian J Nephrol. 2017;27:185-9.
- [Google Scholar]
- The type of vascular access and the incidence of mortality in Japanese dialysis patients. Intern Med. 2017;56:481-5.
- [Google Scholar]
- Vascular access use and outcomes: An international perspective from the Dialysis Outcomes and Practice Patterns Study. Nephrol Dial Transplant. 2008;23:3219-26.
- [Google Scholar]
- Patients referred for arteriovenous fistula construction: A retrospective outcome analysis. Ir J Med Sci 2019 doi: 101007/s11845-019-02090-9
- [Google Scholar]
- Results of the HEMO Study suggest that p-cresolsulfate and indoxyl sulfate are not associated with cardiovascular outcomes. Kidney Int. 2017;92:1484-92.
- [Google Scholar]
- Measuring residual renal function for hemodialysis adequacy: Is there an easier option? Hemodial Int. 2017;21(Suppl 2):S41-6.
- [Google Scholar]
- Association of dose and frequency on the survival of patients on maintenance of hemodialysis in China: A Kaplan-Meier and Cox-Proportional Hazard Model Analysis. Med Sci Monit. 2018;24:5329-37.
- [Google Scholar]
- Referral pattern of patients with end-stage renal disease at a public sector hospital and its impact on outcome. Natl Med J India. 2011;24:208-13.
- [Google Scholar]
- Indians Pay 78% of Medical Expenses From Their Own Pocket. New Delhi: The Times of India 2011
- [Google Scholar]







