Translate this page into:
Rare Case Report of De-novo Pauci-immune Necrotizing Crescentic Glomerulonephritis in 1st-week Post-kidney Transplantation
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Early post-transplant de-novo pauci-immune necrotizing crescentic glomerulonephritis occurring within the first week post transplantation has not been reported according to the literature search done by us. Here, we are reporting a 56 years male patient who underwent living spousal donor kidney transplantation for presumed diabetic nephropathy, and developed pauci-immune necrotizing crescentic glomerulonephritis (NCGN) on sixth day post-transplant. Post-renal transplant recurrence of disease in ANCA-associated vasculitis patients occurs within days to months. However, development of de-novo pauci-immune crescentic glomerulonephritis is a rare occurrence. We report this patient who developed probable pauci-immune de-novo NCGN which responded to treatment with plasmapheresis, steroids and cyclophosphamide.
Keywords
Cyclophosphamide
de-novo pauci-immune necrotizing crescentic glomerulonephritis
plasmapheresis
kidney transplant
Case Presentation
A 56-year-old gentleman, with a history of type 2 diabetes mellitus for 22 years, hypertension for 8 years, with evidence of moderate non-proliferative diabetic retinopathy and macular edema, needing laser therapy for the same, was diagnosed to have proteinuric chronic kidney disease in 2013. Since the patient had proteinuria of 1.6 g/day, retinal changes, diabetic peripheral neuropathy, and history of the long duration of diabetes mellitus, the patient was diagnosed as having diabetic nephropathy. He was on optimal medical management with a nephrology consultant. During follow-up, his serum creatinine showed increasing levels from 2 mg/dL in 2013 progressively to around 9 mg/dL in December 2016. The patient was initiated on maintenance hemodialysis, through left brachiocephalic arteriovenous (AV) fistula. The patient was referred to our nephrology services for renal transplantation with his wife as prospective donor, who had no comorbidities.
Since the patient had ravages of diabetic microvascular disease and long duration of diabetes, the native kidney disease was presumed to be diabetic nephropathy and native kidney biopsy was not done. He underwent ABO compatible allograft kidney transplantation on 14th November 2017, with anti-thymocyte globulin (ATG) induction (3 mg/kg), and standard triple immunosuppression with tacrolimus (0.075 mg/kg from pretransplant day minus 2), mycophenolate mofetil (2 g/day), and steroids as per institution protocol.
The patient had no significant intraoperative event and his urine output in the first hour was 500 mL. He continued to have good urine output with serum creatinine showing a decreasing trend in the first 2 days. After that, on postoperative day 3 the serum creatinine plateaued at 2.3 mg/dL. He underwent renal Tc-99m ethylenedicysteine (EC) scan the same day, which showed features of acute tubular injury. Tacrolimus levels were 7 ng/mL on the 3rd postoperative day. The patient was continued on triple-drug immunosuppression, but the serum creatinine remained at 2.3-2.4 mg/dl on postoperative days 3, 4, and 5 [Table 1].
| Headings | Pretransplant | POD1 | POD2 | POD3 | POD4 | POD5 | POD6 | POD7 | POD8 | POD9 | POD10 | POD11 | POD12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BUN | 31 | 25 | 31 | 35 | 37 | 43 | 50 | 50 | 46 | 44 | ||||
| S.Cr | 9.1 | 3.8 | 2.7 | 2.3 | 2.4 | 2.4 | 2.5 | 2.4 | 2.2 | 2.1 | 2.2 | 1.8 | 1.8 | |
| K+ | 4.4 | 4.6 | 4.9 | 4.3 | 4.5 | 4.5 | 4.3 | 3.8 | 3.3 | 4.1 | 3.8 | |||
| Hb | 10.6 | 9 | 8.7 | 7.7 | 8 | 7.8 | 7.3 | 7 | 9.4 | 8.7 | 9 | |||
| TC | 10600 | 8300 | 6070 | 5300 | 5160 | 5320 | 7720 | 9840 | 13410 | 10090 | 13240 | |||
| Platelets | 3.32 lakh | 2.4 | 2.3 | 2.4 | 2.8 | 2.5 | 2.7 | 2.7 | 2.2 | 2.5 | ||||
| LFT | normal | |||||||||||||
| LDH | ||||||||||||||
| Urine PCR | 1.9 | |||||||||||||
| Urine microscopy | albumin 2+, occ RBC, 1-2 WBC | albumin 2+, numerous RBC, 6-8 WBC | 3+ albumin, numerous RBC, 20-30 WBC | |||||||||||
| Urine output | 200ML | 10 L | 6.7 L | 6.8 L | 6.2 L | 5.4 L | 5.3 L | 4.8 L | 4.0 L | 3.9 L | 3.3 L | 2.4 L | 3.4 L | 5.4 L |
| Intervention | Tac 4mg/day | tac 4mg/day | EC renal scan showed ATN | Doppler showed increased RI | Kidney biopsy | Plasmapheresis started | 2nd Plasmapheresis | 3rd PP | 4th PLEX | 5th PLEX | Cyclophosphamide 500mg | |||
| Tacrolimus reduced 2mg/day | Tacrolimus stopped | C3 complement, ANA, ANCA, anti-GBM | PRBC | Tacrolimus 2mg/day | Tacrolimus 4mg/day | Tacrolimus continued | ||||||||
| tacrolimus level sent | tacrolimus level 7 ng/ml | ATG 50 mg plus 500mg Solumedrol | 20 GM iv Ig | 2nd Kidney biopsy | ||||||||||
| DSA sent |
BUN: Blood urea nitrogen; s.cr: Creatinine; K+: Potassium; POD: Postoperative day; EC renal scan: Ethylenedicysteine renal scan; PLEX: Plasmapheresis
The patient underwent renal allograft biopsy on day 5 and one core was sent for a histopathology examination. The patient received an extra dose of pulse methylprednisolone 500 mg and 50 mg of ATG was given and tacrolimus was stopped. The immunofluorescence core was not taken since the suspicion was of acute rejection. Donor specific antibodies were repeated which returned negative. The provisional report suggested crescentic glomerulonephritis, so the patient was taken up for plasmapheresis with 3.4 L (1.5 plasma volume) plasma exchange. Serum for C3, anti-GBM, and ANA and ANCA (both by indirect immunofluorescence and ELISA) were sent prior to starting the plasma exchanges, all of which returned negative. He was given five plasma exchanges from postoperative day 6 and 20 g of IV immunoglobulin over the next 6 days. Final report of kidney biopsy was available on postoperative day 7, which showed necrotizing partially oriented active cellular crescents in 6/7 glomeruli, [Figures 1 and 2] with no features suggestive of rejection, there was a severe acute tubular injury, immunofluorescence with Pronase digestion of the core was negative for a panel of antisera including anti-GBM. His serum creatinine started showing a downward trend from day 8 onwards and reached 1.8 mg/dL at discharge on day 13. He was re-started on tacrolimus from postoperative day 10, and increased upwards on day 11, with a plan to achieve a target level of 10-12 ng/ml. The tacrolimus dose was increased to 6 mg/day on day 14 and achieved a tacrolimus level of 10.8 on day 16 postoperative day [Table 1].
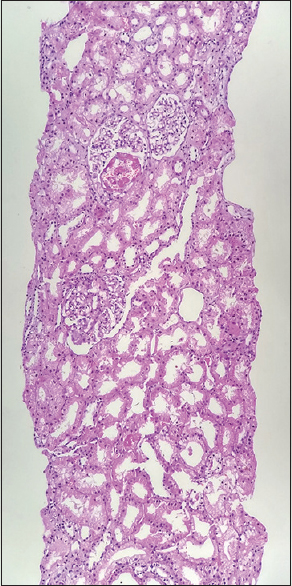
- Low-power view showing glomeruli with tuft necrosis in the first kidney biopsy
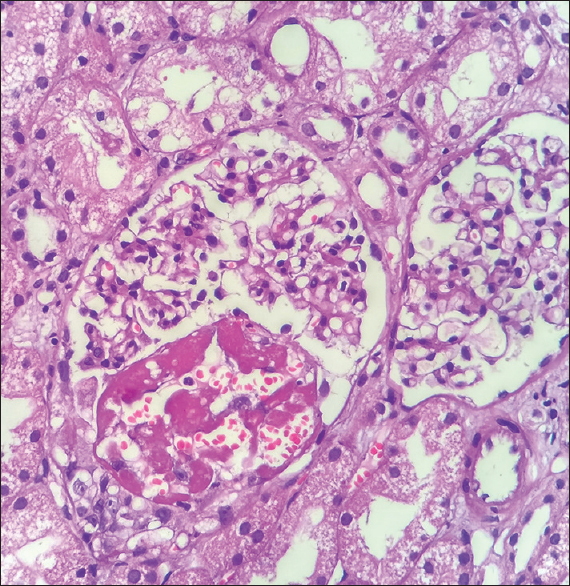
- High-power view showing partial cellular crescents and tuft necrosis in the first kidney biopsy
He underwent a repeat allograft kidney on day 12 and received 500 mg of IV cyclophosphamide. The repeat kidney biopsy showed a decrease in the crescents and improvement in histology [Figures 3 and 4]. The immunofluorescence staining of the repeat allograft kidney biopsy did not reveal staining for a panel of anti-sera including for anti-GBM [Figure 5]. The patient in the meanwhile developed mild fluid overload which improved with the diuretic infusion.
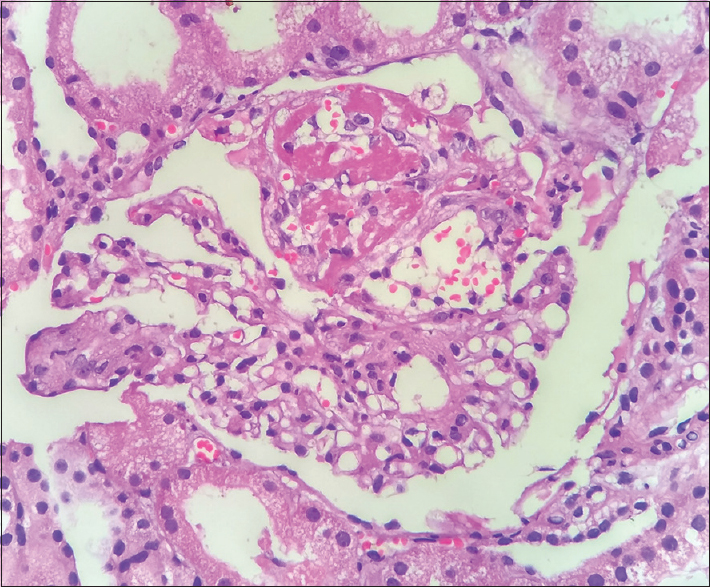
- High-power view of second kidney biopsy showing tuft necrosis at 12 O' clock position
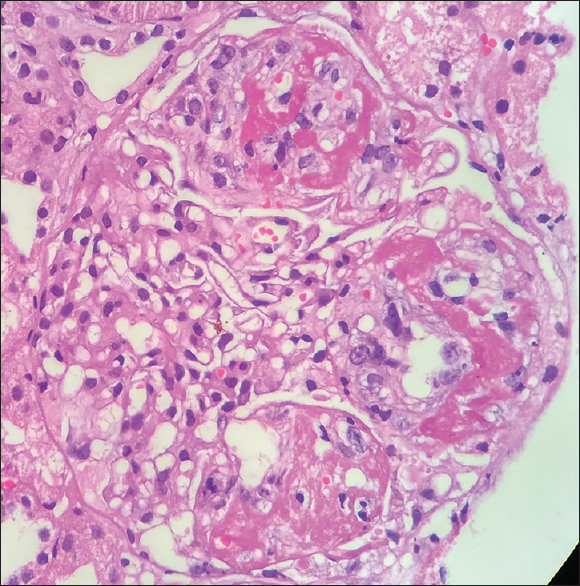
- High-power view of crescentic GN at 9 O' clock position seen on the 2nd kidney biopsy
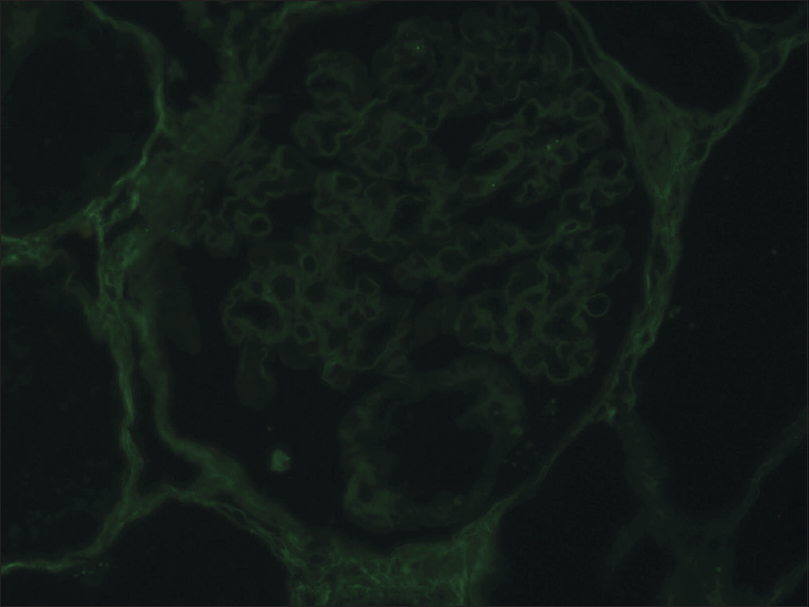
- Immunofluorescence showing negative staining of IgG on second kidney biopsy
The patient was discharged with a serum creatinine of 2 mg/dL and was on tacrolimus, steroid, antiviral, antibacterial and antifungal prophylaxis, with a plan to introduce mycophenolate mofetil after 6 doses of cyclophosphamide. The patient was followed up on an outpatient basis, and he received a 3 g cumulative dose of cyclophosphamide. The patient was continued on triple immunosuppression with the nadir serum creatinine reaching 1.3 mg/dL after 3 months of follow-up. He remains on follow-up with no significant problems, with a serum creatinine of 1.8 mg/dL after more than 22 months. The patient underwent a repeat ANCA testing by ELISA in September 2019, which is showing weak positive for MPO-ANCA.
Discussion
Crescentic glomerulonephritis can be seen in three broad categories, viz, a) anti-GBM associated glomerulonephritis, b) immune complex-mediated glomerulonephritis—ICGN (may be due to Henoch Schonlein GN, LN (classes III and IV), IgA nephropathy, acute postinfectious GN, fibrillary glomerulonephritis, type I MPGN, and membranous glomerulonephritis) and c) pauci-immune crescentic glomerulonephritis (ANCA associated, renal limited).
The patients with ANCA-associated vasculitis (AAV) with renal failure who underwent renal transplantation have a recurrence rate of 17%, with histology and clinical recurrence occurring within days to many years1. In our patient, the serum profile for autoimmune antibodies and complement C3 was negative, and the immunofluorescence done on the second biopsy was negative for a panel of antisera. So, the likelihood of a patient having ICGN, pauci-immune GN, or anti-GBM glomerulonephritis due to recurrence of the disease is unlikely. The possibility of de-novo anti-GBM due to Alport disease is also unlikely in this patient as he had no family history of kidney disease and did not have any hearing loss or eye changes suggestive of the same. There have been reports of allograft kidney failure by anti-GBM disease, but not pauci-immune disease, in patients with Alport disease, which recurred post-transplantation, first transplant occurring after several months, with the second transplantation showing early crescentic GN.[2] There is a case reported whose native kidney disease was chronic interstitial nephritis, who showed early crescentic glomerulonephritis around the 7th day of transplantation, which also showed the presence of anti-GBM antibody in the graft kidney.[3] There was a case report from Chandigarh, India where a patient with ESRD due to Pauciimmune Crescentic Glomerulonephritis developed recurrence around 8th-month post-transplant, but this did not respond to treatment and the patient developed graft failure in 11th month needing initiation of renal replacement therapy.[4] Tabeta et al described two cases of anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis (ANCA-V) which occurred in the transplanted kidney. One was a relapse of necrotizing crescentic glomerulonephritis occurring after 1 year of transplantation, which progressed to ESRD around 3 years post-transplantation, and the second case whose native kidney disease was IgA nephropathy developed de novo onset of necrotizing crescentic glomerulonephritis occurred at 14 years 10 months after transplantation with positive serum reaction for MPO-ANCA which was very late compared to our case and that patient was initiated on hemodialysis five years after the onset of ANCA-V.[5]
There was a recent retrospective case series of 10 de-novo pauci-immune crescentic glomerulonephritis, but the earliest occurrence of de-novo appearance was at 4 months, though all of them were renal limited variant as in our case which however appeared within the first week of transplantation.[6]
The available literature shows the presence of NCGN in the presence of anti-GBM antibodies in case of early occurrence of denovo crescentic glomerulonephritis and was not pauci-immune GN, and the case series that reported de-novo pauci-immune GN, the earliest diagnosis was at 4 months post-transplantation. The reason for the appearance of pauci-immune necrotizing crescentic glomerulonephritis in the graft kidney within the 1st-week post-transplantation is baffling. But, it underlines the importance of keeping a low threshold for allograft kidney biopsy, which enabled us to initiate plasmapheresis and cyclophosphamide preserving the renal allograft function.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The long-term outcomes of systemic vasculitis. Nephrol Dial Transplant. 2015;30(Suppl 1):i60-6.
- [Google Scholar]
- Failure of two subsequent renal grafts by anti-GBM glomerulonephritis in Alport's syndrome: Case report and review of the literature. Transplant Int. 1990;3:82-5.
- [Google Scholar]
- De novo crescentic glomerulonephritis in a renal transplant. Am J Kidney Dis. 1990;16:501-3.
- [Google Scholar]
- Recurrence of ANCA-negative renal-limited pauci-immune glomerulonephritis in the renal allograft. Clin Kidney J. 2013;6:519-22.
- [Google Scholar]
- Two cases of ANCA associated vasculitis in post-transplant kidney: Relapse and denovo. Clin Transplant. 2009;23(Suppl. 20):49-53.
- [Google Scholar]
- De novo pauci-immune glomerulonephritis in renal allografts. Mod Pathol. 2020;33:440-7.
- [Google Scholar]







