Translate this page into:
Tacrolimus-induced Epidermoid Cysts in the Renal Transplant Patient
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Epidermal cysts are common benign cystic lesions that occur mostly sporadically. Common sites involved are arms, face, and trunk. The cyst may progress slowly and remain for years. These cysts arise as a result of the plugging of the follicular orifice. Etiology has largely remained unknown although local trauma, ultraviolet rays, and human papilloma virus (HPV) have been implicated in a few cases. Calcineurin inhibitors (CNIs) especially cyclosporine has been discredited for cutaneous side effects such as hirsutism and gingival hyperplasia. Epidermoid cysts have been also associated with patients with solid organ transplant recipients on cyclosporine. Tacrolimus is considered to be free of dermatological side effects. Herein, we report a case of 56-year-old renal allograft recipient on tacrolimus, who develop more than >100 epidermoid cysts over the face, trunk, back, and extremities. The lesions ceased to progress once the tacrolimus was stopped.
Keywords
Epidermal cyst
epidermoid cyst
immunosuppression
tacrolimus
transplant
Introduction
Epidermal cyst also known as an epidermoid cyst or epidermal inclusion cyst is one of the most common cutaneous cysts and is generally found over the face, base of the ear, and trunk. It is characterized by skin-colored dermal nodules ranging from few millimeters to several centimeters with a characteristic central punctum. Although epidermoid cyst most commonly results from plugging of the follicular orifice, it may also occur due to trauma or penetrating injury.[1] Ultraviolet rays and human papilloma virus (HPV) have also been implicated as its etiology.[2] Most of the cysts resolve spontaneously but they tend to recur. For cosmetic purposes, a surgical excision is a viable option. When cysts are abnormal in number or location, Gardener syndrome should be suspected. It is a rare inherited condition characterized by familial adenomatous polyposis of the colon associated with several other extracolonic abnormalities.
CNIs are the backbone of the immunosuppression armamentarium used in renal transplantation. Within CNIs, tacrolimus is considered superior to cyclosporine with a better cardiovascular risk profile and superior renal function.[3] One of the frequent side effects of cyclosporine is its cutaneous manifestation, commonly hirsutism, and gingival hyperplasia. Multiple cases of epidermoid cysts associated with cyclosporine have been described in the literature but cysts have rarely been linked with tacrolimus use. Herein, we describe a rare case of tacrolimus induced multiple epidermoid cysts in a renal transplant patient.
Case Report
A 57-year-old male underwent a live-related renal transplant in January 2016. He received anti-thymocyte globulin (ATG) and triple immunosuppressive drug regimen including tacrolimus, prednisolone, and mycophenolate mofetil (MMF). He was discharged on 10th-day postoperatively with serum creatinine (S.Cr) of 2.10 mg/dL. His tacrolimus level at discharge was 9.4 U/L. His S.Cr was stabilized at 2.02 mg/dL. In the 3rd month postoperatively, the patient noticed papular eruptions on the back and forehead. He consulted a skin specialist and symptomatic treatment was provided. Given the persistent appearance of new crops of skin lesion patient underwent a skin biopsy from his forehead, histopathology showed features consistent with the epidermoid cyst. Since tacrolimus induced epidermoid cyst is rare, and spontaneous eruption and resolution are more common, a conservative approach was followed without any change in the immunosuppression. In the following months, he noticed a gradual increase in size as well as numbers (>100 nodules) with the involvement of the face, chest, and arms over 2 years. In September 2017, he presented with a rise of creatinine to 2.8 mg/dL. In October 2017, a renal biopsy was done which showed chronic allograft injury with moderate Interstitial fibrosis and tubular atrophy. From December 2017 to September 2018, the patient had a persistent rise in S.Cr and eventually, he was shifted to hemodialysis. His immunosuppression medication including MMF and tacrolimus was stopped. Prednisolone was continued at a low dose (5 mg). Since then, new skin lesions have not yet appeared but inflammation and infection of the existing lesions have continued to occur [Figures 1-3]. Given persistent distress due to skin lesions over trunk and face multiple skin biopsies were taken from the back which showed characteristic features of the epidermoid cyst [Figure 4]. Another skin biopsy was done a few months later to detect HPV infection. Sample was tested for HPV-DNA by Real Time PCR (genotypes- 6, 11, 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, and 59), which came out to be negative.

- Multiple papulonodular lesions with characteristic “punctum” over the back. Healed dark brown scars along with tender erythematous nodules (Inset). A white bandage is seen overlying the skin biopsy site (Box)
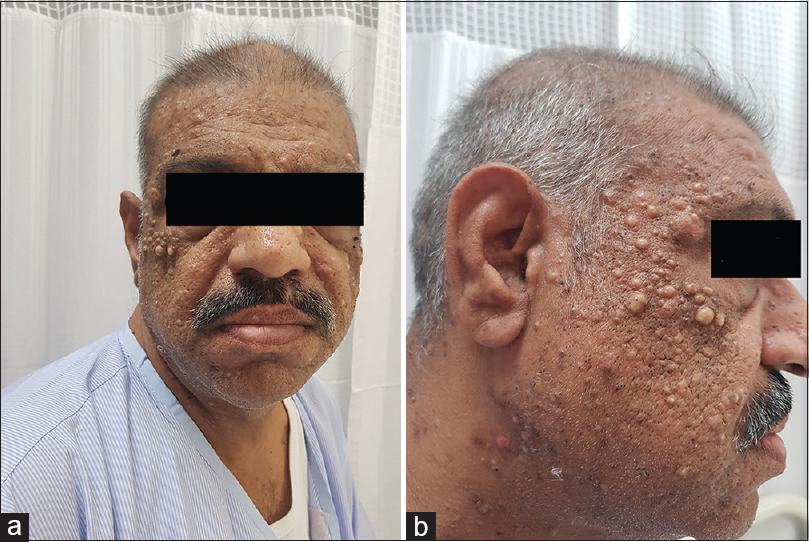
- (a and b): Characteristic epidermoid cysts over the face

- Epidermoid cysts over the chest and abdomen (a) and arms (b)

- Light microscopy showing stratified squamous epithelium (long arrow) with keratin debris (Arrowhead) (H and E stain; 4X)
Discussion
The direct causality of tacrolimus with the epidermoid cyst is difficult to establish as the literature on this is very scarce. Multiple case reports have been published attributing association of epidermoid cyst with cyclosporine. [456] In a prospective analysis by Bencini et al. in 67 renal transplant patients treated with cyclosporine and low-dose steroids found that epidermoid cyst occurred in 28% of patients. Around 74% of cysts appeared in the first 3 months of transplant and 88% of cysts in the initial 6th month.[4]
Tacrolimus though differs from cyclosporine in chemical structure, its mechanism of action is similar. Both are CNIs and act by inhibition of dephosphorylation of the nuclear factor of activated T cells (NFAT) thereby inhibiting the downward signaling and lymphocyte proliferation. Tacrolimus, due to its potent T-cell inhibition and keratinocyte apoptosis inhibition, is indicated in certain dermatological conditions such as atopic dermatosis. In a case report by Schoendorff C and colleagues, they hypothesized that the follicular blockage caused by the increased keratinization induced by cyclosporine and steroids would have led to the epidermoid cyst.[6] Since the mechanism of action both the drugs are the same that could explain cyst in this patient also.
Multiple studies have demonstrated the association of HPV in the epidermoid cyst in non-immunosuppressed patients.[278910] In an immunosuppressed person, exacerbation of HPV infection with a florid presentation as seen in this case was a strong possibility. In view of this, a repeat biopsy was performed to specifically look for HPV. Its absence in the tissue suggests alternative mechanisms.
In a similar case to ours, Ahn and colleagues reported multiple epidermoid cysts in a post-transplant patient who was on tacrolimus.[11] The cyst appeared after 3 years post-transplant which was rather late as compared to other case reports where it was most common after 3 months of transplantation in patients on cyclosporine. In our case, cysts appeared within 3 months of transplantation which can be explained with a higher dose of tacrolimus during initial months of transplantation.
Tacrolimus induced epidermoid cyst is extremely rare and this is the second case reported in the literature.
Conclusions
Epidermoid cysts rarely can occur with tacrolimus use. These cysts are large in number and heal with scars. Early withdrawal of the drug should be done to prevent the progression of the cysts.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Human papillomavirus infection and ultraviolet light exposure as epidermoid inclusion cyst risk factors in a patient with epidermodysplasia verruciformis? J Am Acad Dermatol. 2008;58:S68.e1-6.
- [Google Scholar]
- Tacrolimus versus ciclosporin immunosuppression: Long-term outcome in renal transplantation. Nephrol Dial Transplant. 2003;18:i7-11.
- [Google Scholar]
- Cutaneous lesions in 67 cyclosporin-treated renal transplant recipients. Dermatologica. 1986;172:24-30.
- [Google Scholar]
- Multiple, large, polypoid infundibular (epidermoid) cysts in a cyclosporin-treated renal transplant recipient. Dermatology. 2000;201:78.
- [Google Scholar]
- Multiple epidermoid cysts in a renal transplant recipient taking cyclosporine A. Cutis. 1992;50:36-8.
- [Google Scholar]
- Detection of human papillomavirus 60 in epidermal cysts of nonpalmoplantar location. Am J Dermatopathol. 2003;25:243-7.
- [Google Scholar]
- 'Cystic papilloma' in humans? Demonstration of human papillomavirus in plantar epidermoid cysts. Arch Dermatol. 1990;126:1599-1603.
- [Google Scholar]
- Human papillomavirus 57 identified in a plantar epidermoid cyst. Br J Dermatol. 1998;138:510-4.
- [Google Scholar]
- Epidermal cysts in a tacrolimus treated renal transplant recipient. Ann Dermatol. 2011;23(Suppl 2):S182-4.
- [Google Scholar]







