Translate this page into:
Laparoscopic versus Open-surgery Catheter Placement in Peritoneal Dialysis Patients: A Meta-analysis of Outcomes
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The peritoneal dialysis catheter (PDC) can be placed either through the laparoscopic technique, percutaneous technique or surgical procedures. The utilization of these PDC placement procedures is based on successful placement and reduced risk of development of complications. The main objective of this study was to compare the complications associated with laparoscopic vs. open-surgery PDC placement procedure. Literature for this review was obtained from PubMed and Google Scholar databases. The literature search was limited to studies published in the period between 1998 and 2019. The meta-analysis was done using Stata Version 12. The results showed significant difference in catheter malfunction between the laparoscopic and open-surgery group (relative risk [RR] =0.58; 95% CI: 0.42–0.8; P = 0.031). Furthermore, there was no significant statistical difference in dialysate leakage (RR = 0.77; 95% CI: 0.51–1.17, P = 0.116) peritonitis (RR = 0.8; 95% CI: 0.6–1.06, P = 0.349) and exit-site infection (RR = 0.84; 95% CI: 0.65–1.09, P = 0.834) between the laparoscopic and open-surgery PDC placement groups. In conclusion, the laparoscopic PDC placement procedure was superior to open surgery in regards to catheter malfunction. Additionally, the choice of treatment procedure should put in consideration factors such as cost and comfortability of the patient.
Keywords
Peritoneal dialysis catheter insertion
CAPD catheter insertion
open surgery
laparoscopic PDC insertion
Introduction
Peritoneal dialysis (PD) is one of the documented alternative treatments for end-stage renal disease (ESRD). However, some of the challenges associated with this treatment method include catheter-related infections, leakage of dialysate and outflow obstruction among others.[1] Since the introduction of the PD in 1976, increased use of the treatment method has been reported by patients. In the period between 2009 and 2013 for instance, there was a 68% increase in use of PD among ESRD patients.[2] The increased acceptance of the treatment procedure was attributed to improved quality of life among patients, improved catheter survival rates after the first year of dialysis initiation and good protection of residual renal functioning.[3]
The placement of the peritoneal dialysis catheter (PDC) can be done through open surgical method, laparoscopic procedure, percutaneous fluoroscopic procedure and peritoneoscopic implantation.[4] Among the PDC procedures, the open surgical method is commonly used though constrained by high risks of complications among the ESRD patients.[5] In recent years, the laparoscopic procedure has been recommended since it is less invasive and has good visibility during catheter placement.[1] Some studies have, therefore, documented high efficacy of the laparoscopic catheter insertion technique as compared to open surgery.[6] On the other hand, some researchers report that the laparoscopic technique cannot avert the complications of PD.[17]
In the midst of the contradicting information, no studies have extensively and exhaustively compared the open-surgery and laparoscopic PDC placement procedures. Furthermore, most recent meta-analysis studies have not incorporated the current clinical studies.[8] Additionally, ESRD is significantly contributing to the global burden of disease with annual increasing rate of 20,000 cases.[910] Thus, this study aimed at comparing the laparoscopic and open-surgery catheter placement procedures in regards to catheter-related complications.
Methodology
Search strategy
A comprehensive and systematic literature search was conducted in PubMed and Google Scholar for studies focusing on the comparison between laparoscopic and open-surgery catheter placement procedures in PD. The following keywords were used in the search: PD, open surgery, laparoscopic, catheter placement and ESRD.
Study selection
The inclusion criteria included studies that were randomized controlled trials, cohort studies or retrospective studies. It also included studies that measured PDC placement outcomes, that is catheter malfunctioning, dialysate leakages, peritonitis and exit-site infection. Additionally, only the most recent clinical studies were considered. Studies that were excluded were case reports, letters and studies with unavailable data. Also, practical guides/manuals, non-English studies and paediatric studies were also excluded from the analysis. Two independent authors reviewed all articles obtained in the initial search against the inclusion criteria. Disagreements among the reviewers were resolved through consensus.
Data abstraction
Out of the 50 potential studies, 35 of them were eliminated due to duplication, unavailability of data, focusing on paediatric studies, being non-comparative studies and being written in a non-English language [Figure 1]. Data were abstracted using a standard form that captured the number of patients, demographic characteristics, study design and PDC placement-related outcomes.
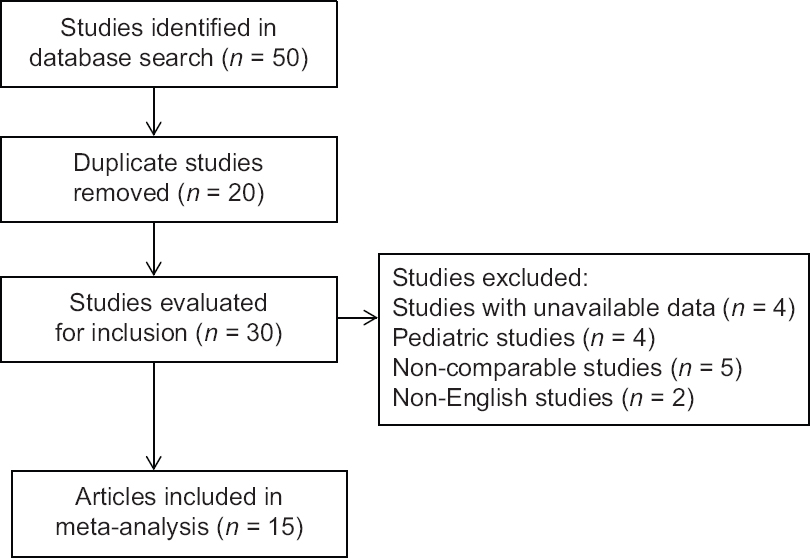
- Selection strategy for studies to be included in meta-analysis
Statistical analysis
Statistical analysis was conducted using Stata version 12 (Stata Corporation, College Station, TX 77845, USA). The random effects model was employed to assess the key outcomes of interest (dialysate leakage, catheter malfunction, peritonitis and exit-site infection). Forest plots were employed to show the between study variation in effect sizes. Publication bias was assessed using funnel plots. The heterogeneity across the studies was evaluated using the Q statistic and I2 index. Statistical analysis was done at 95% confidence interval.
Results
The studies included in the meta-analysis followed 4819 patients. The patients included in the study were adults aged 51.5 ± 33.5 years. The study period for the incorporated studies was from 1992 to 2019 as shown in Table 1. Based on the meta-analysis, there was no statistical significant difference in dialysate leakages between the laparoscopic and open-surgery groups (relative risk [RR] = 0.77; 95% CI: 0.51–1.17, P = 0.116) as shown in Figure 2. There was a significant difference in catheter malfunction between the laparoscopic and open-surgery group (RR = 0.58; 95% CI: 0.42–0.80, P = 0.031). Comparison of peritonitis between laparoscopic and open-surgery group showed that neither of the procedures had inferior incidences of peritonitis (RR = 0.8; 95% CI: 0.6–1.06, P = 0.349). There was no significant difference in exit-site infection between the laparoscopic and open-surgery group (RR = 0.84; 95% CI: 0.65–1.09, P = 0.834).
| Study | Country | Year of publication | Study design | Study period | Number of patients | Age (years) | Comparison | Outcomes |
|---|---|---|---|---|---|---|---|---|
| Tuncer, Yardimsever and Ersoy[11] | Turkey | 2003 | Prospective, non-randomized | March 1998-October 2001 | 42 | 46.9±8.8 | Laparoscopic omental fixation vs. open surgical placement | Complications |
| Soontrapornchai and Simapatanapong[12] | Thailand | 2005 | Prospective, non-randomized | May 1999-May 2001 | 102 | 57.5±19.1 | Open and laparoscopic secure placement | Complications |
| Jwo et al.[1] | China | 2008 | Prospective randomized | December 2002-October 2006 | 77 | 54.4±16.5 | Open surgery with laparoscopic-assisted placement | Positive findings of complications |
| Wright et al.[13] | UK | 1999 | Prospective randomized | 45 | 49.3±20.2 | Laparoscopic and open peritoneal dialysis | Complications of catheter insertion | |
| Prabhakar et al.[14] | USA | 2019 | Retrospective, non-randomized | May 2005-March 2018 | 173 | 58.3±1.1 | Laparoscopic and open CAPD placement | Complications (infection, malposition and malfunction) |
| Atapour et al.[15] | Iran | 2011 | Randomized clinical trial | 2009-2010 | 61 | 55.1±17.2 | Outcome of open surgical procedure and PDC insertion using laparoscopic needle | Complications |
| Cox et al.[16] | USA | 2016 | Retrospective, non-randomized | 2005-2012 | 3134 | 59.4±24.0 | Laparoscopic vs. open peritoneal dialysis | Surgical outcomes for PDC placement |
| van Laanen et al.[17] | Netherlands | 2018 | Randomized controlled trial | March 2010-March 2016 | 90 | 63.6±21.3 | Open vs. laparoscopic placement | Reasons for failure and clinical successes |
| Bircan and Kulah[18] | Turkey | 2016 | Prospective non-randomized | 2007-2014 | 69 | 63.1±21.1 | Open vs. laparoscopic preperitoneal tunnelling | Catheter-related complications |
| Gadallah et al.[19] | USA | 1999 | Prospective cohort | October 1992-October 1995 | 148 | 46.4±4.5 | Peritoneoscopic vs. surgical placement | Complications and causes of termination of study monitoring |
| Tsimoyiannis et al.[20] | Greece | 2000 | Prospective randomized | 50 | 60±17 | Laparoscopic placement of the Tenckhoff catheter | Operative variables | |
| Gajjar et al.[21] | USA | 2007 | Retrospective non-randomized | 75 | 55.7±32.2 | Laparoscopic vs. traditional placement techniques | Immediate function and complications | |
| Crabtree and Fishman[22] | USA | 2005 | Prospective cohort | 1992-2002 | 341 | 52.3±16.5 | Basic and advanced laparoscopic vs. open dissection | Clinical details of PDC placement |
| Batey et al.[6] | Kentucky | 2002 | Retrospective cohort | January 2000-March 2001 | 26 | 45.5±26.5 | Mini laparoscopic assisted vs. open surgical method | Operative and post-operative data |
| Draganic et al.[23] | Australia | 1998 | Retrospective cohort | 60 | 50.5±32.5 | Laparoscopy vs. laparotomy | Perioperative complications | |
| Eklund et al.[24] | Finland | 1998 | Retrospective cohort | June 1994-March 1997 | 102 | 51.1±1.1 | Peritoneoscopic vs. surgical | Catheter-related complications |
| Sun et al.[25] | New Zealand | 2016 | Retrospective cohort | August 2009-July 2013 | 224 | 55.2±16.4 | Peritoneoscopic vs. surgical | Perioperative outcomes |
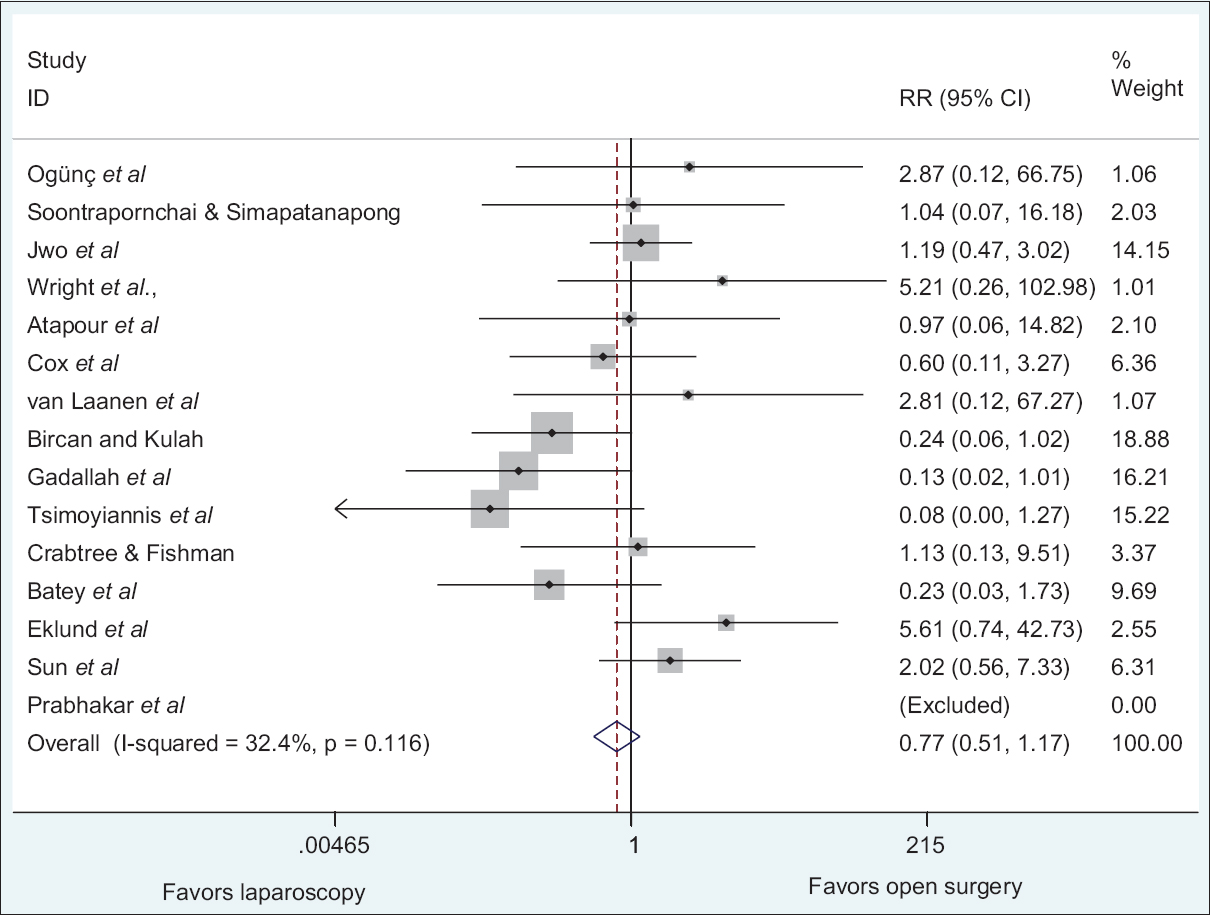
- Relative ratio of dialysate leakages between laparoscopic and open-surgery PDC placement technique
Publication bias
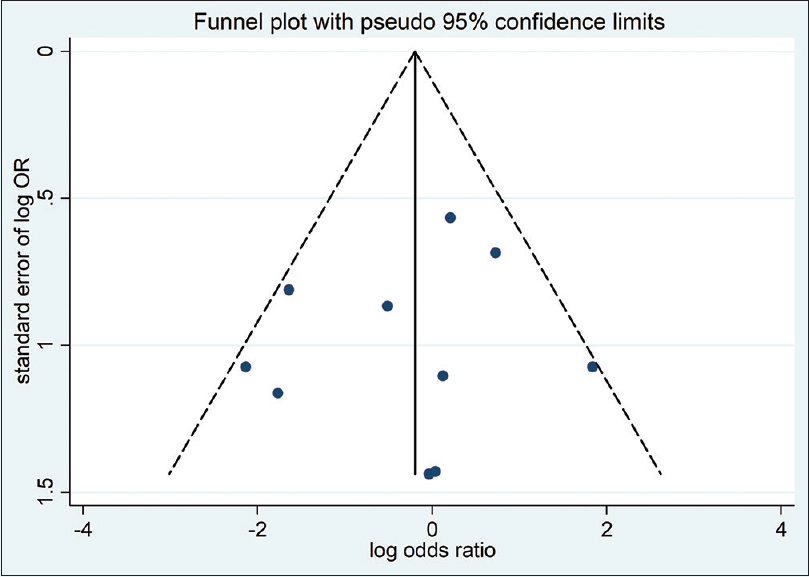
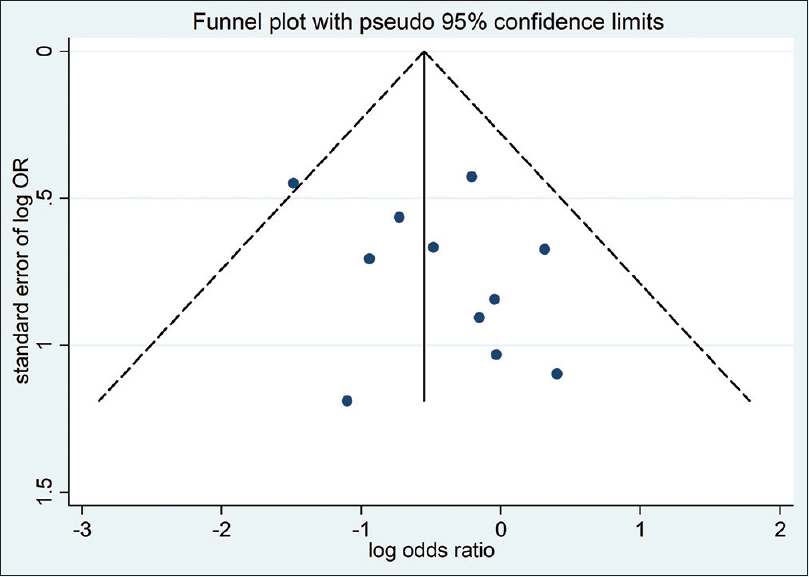
Funnel plots of studies included in the meta-analysis reporting on occurrence of dialysate leakage, catheter malfunction, peritonitis and exit-site infection between laparoscopic and open-surgery group are shown in Figures 6–9. All funnel plots were symmetrical and thus there was no publication bias.

- Relative ratio of catheter malfunction between laparoscopic and open-surgery PDC placement techniques
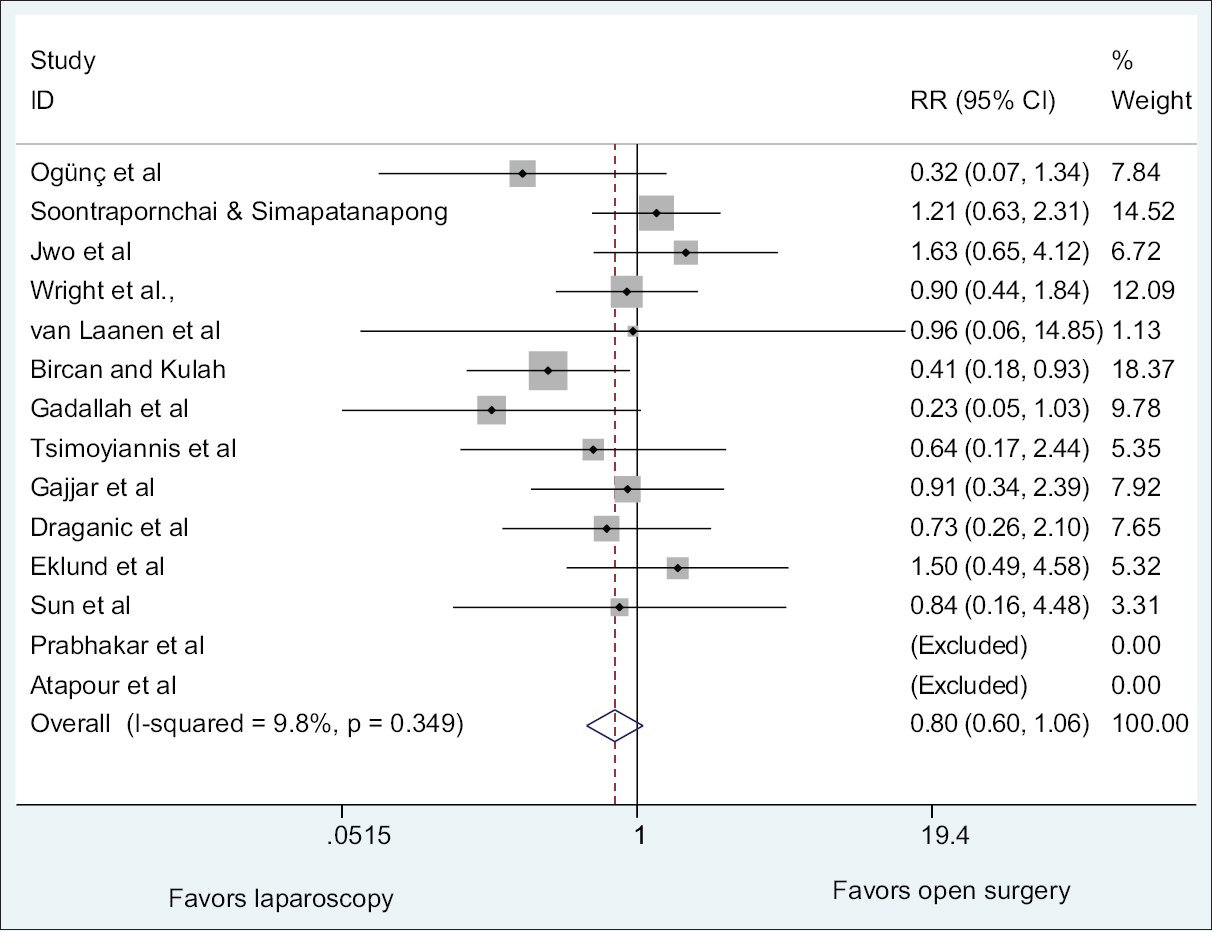
- Relative ratio of peritonitis between laparoscopic and open-surgery PDC placement techniques
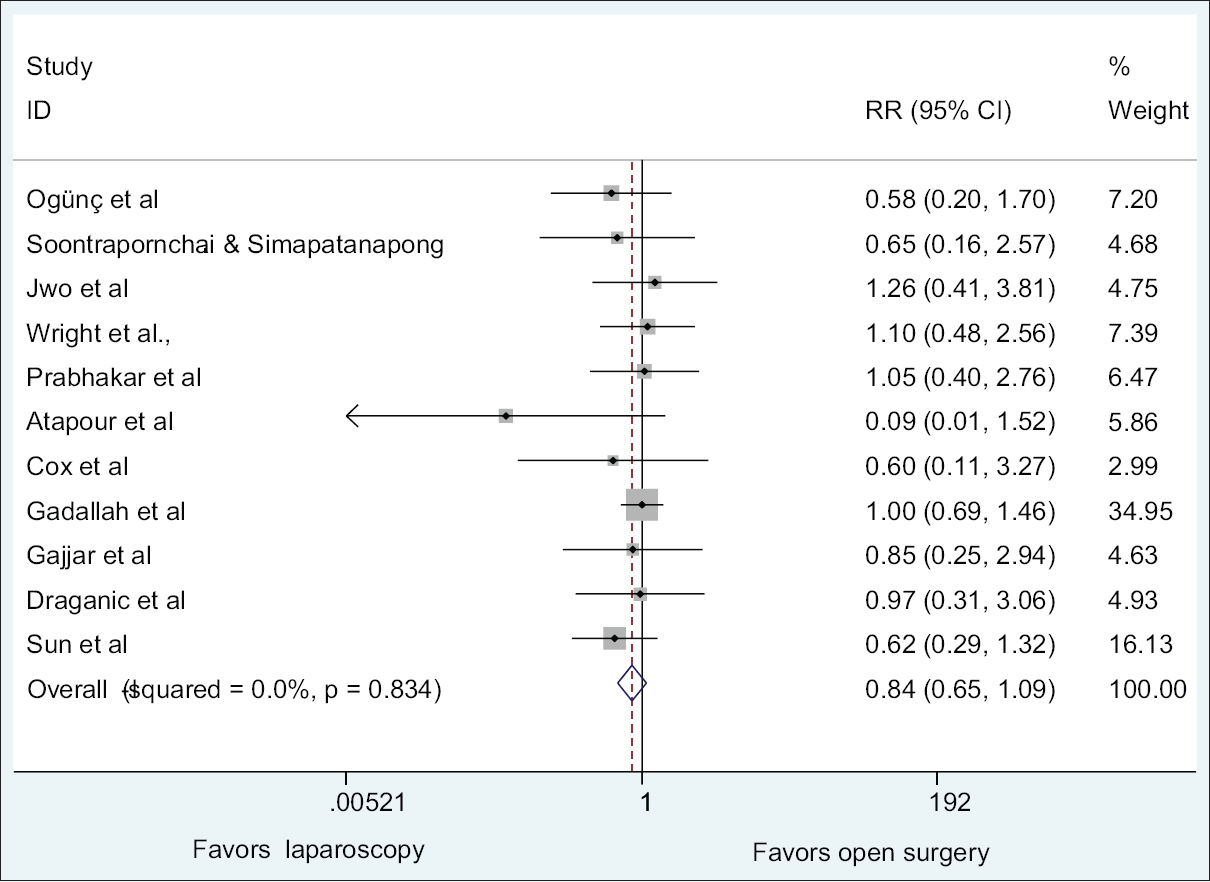
- Relative ratio of exit-site infection between laparoscopic and open-surgery PDC placement techniques
- Funnel plot from all studies comparing dialysate leakage between laparoscopic and open-surgery PDC placement techniques
- Funnel plot from all studies comparing catheter malfunction between laparoscopic and open-surgery PDC placement techniques

- Funnel plot from all studies comparing peritonitis between laparoscopic and open-surgery PDC placement techniques
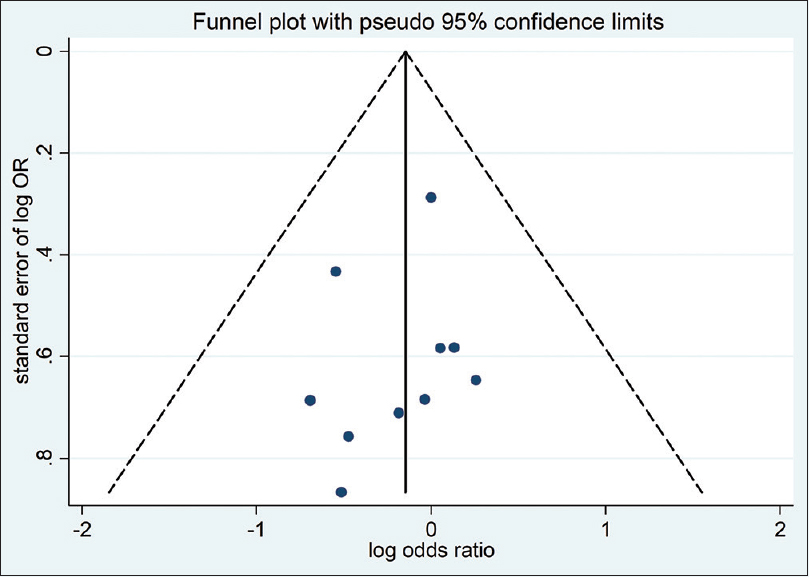
- Funnel plot from all studies comparing exit-site infection between laparoscopic and open-surgery PDC placement techniques
Risk of bias assessment
Risk of bias was assessed using Harbord test as shown in Tables 2–5. Based on the analysis, the meta-analysis was not significantly affected by small studies. Therefore, the meta-analysis could be affected by other factors and not small study effect.
| Z/sqrt (V) | Coef. | Std. err. | t | P>t | 95% Conf. interval | |
|---|---|---|---|---|---|---|
| sqrt (V) | −1.242677 | 0.9392929 | −1.32 | 0.210 | −3.289221 | 0.803866 |
| Bias | 1.179963 | 1.094247 | 1.08 | 0.302 | −1.204196 | 3.564121 |
Test of H0: No small-study effects, P=0.302
| Z/sqrt (V) | Coef. | Std. err. | t | P>t | 95% Conf. interval | |
|---|---|---|---|---|---|---|
| sqrt (V) | −1.350746 | 0.9195935 | −1.47 | 0.168 | −3.354368 | 0.652876 |
| Bias | 1.083912 | 1.333848 | 0.81 | 0.432 | −1.822292 | 3.990117 |
Test of H0: No small-study effects, P=0.432
| Z/sqrt (V) | Coef. | Std. err. | t | P>t | 95% Conf. interval | |
|---|---|---|---|---|---|---|
| sqrt (V) | 0.0531265 | 0.771228 | 0.07 | 0.946 | −1.665277 | 1.77153 |
| Bias | −0.5625115 | 1.290941 | −0.44 | 0.672 | −3.438908 | 2.313885 |
Test of H0: No small-study effects, P=0.672
| Z/sqrt (V) | Coef. | Std. Err. | t | P>t | 95% Conf. interval | |
|---|---|---|---|---|---|---|
| sqrt (V) | 0.2393408 | 0.3787949 | 0.63 | 0.543 | −.6175528 | 1.096234 |
| Bias | −0.9076283 | 0.6999336 | −1.30 | 0.227 | −2.490988 | 0.6757315 |
Test of H0: no small-study effects, P=0.227
Discussion
The success of PD is measured by reduction of catheter-relatedcomplications. Catheter-related complications may result to technical failures which may reduce catheter survival and may consequently warrant for haemodialysis.[26]
The results of this meta-analysis show that there was no statistically significant difference in dialysate leakages between the laparoscopic and open-surgery PDC placement. The results of this study were similar to other meta-analysis which reported no significant difference in dialysate leakages between the laparoscopic and open-surgery groups.[2728] A number of articles have been published which are concurrent with the findings of the meta-analysis. For instance, a prospective randomized study done by Jwo et al. reported no significant difference in dialysate leakage between the laparoscopic and open-surgery group.[1] Similarly a review done by John H. Crabtree revealed no differences in the incidences of dialysate leakage between open surgery and laparoscopic group.[22] However, it is noteworthy to note that dialysate leakage is influenced by other factors such as the time when PD is started. Beginning PD immediately after insertion increases the risk to occurrence of leakage due to inadequate healing of the peritoneum. Additionally, the number of cuffs in a catheter has been documented to influence the occurrence of leaks, especially for the laparoscopic procedure.[28]
The results of the meta-analysis are in agreement with other meta-analysis which concluded that there was significant difference in catheter malfunction between laparoscopic and open-surgery group.[28] Similarly, other studies have reported laparoscopic as a superior catheter placement procedure with lower incidences of catheter malfunction as compared to open surgery. For instance, the study by Crabtree and Fishman which had the highest weight (19.64%) reported higher incidences (17.5%) in the open-surgery group as compared to the laparoscopic group (0.5%).[22] However based on a study conducted in the USA, there was no significance difference in incidences of catheter malfunction between the laparoscopic and open-surgery group.[19] The inconsistency among studies could be attributed to differences in catheters used in different studies.[28] For instance, studies have reported that use of coiled catheters tends to reduce incidences of catheter malfunction.[29] Additionally, the size of the studies may confound the results of the meta-analysis.
Peritonitis remains a big impediment to the application of PD and a contributor to patients going back to haemodialysis.[30] Based on the results of the meta-analysis, there was no significant difference in peritonitis between the laparoscopic and the open-surgery group (P = 0.349). Similarly, based on other meta-analyses, neither the laparoscopic nor the open-surgery PDC placement was superior to the other in terms of peritonitis.[2731] It is worth noting that the results of meta-analysis could be potentially influenced by factors such as application of perioperative antibiotics which has been reported to significantly reduce the risk of early development of peritonitis.[32] Additionally, studies have documented that there is still no consensus on the type of antibiotics to use to prevent occurrence of peritonitis as well as when the antibiotics should be administered.[28]
Our meta-analysis suggests that there is no significant difference in exit-site infection between laparoscopic and open-surgery PDC placement (P = 0.834). Based on a study which had the highest weight (34.95%), the incidences of exit-site infection among the open-surgery and laparoscopic group were not significantly different.[19] Furthermore, the results of this study were in agreement with a previous meta-analyses.[831] Potential confounding factor of occurrence of exit-site infection in the open-surgery and laparoscopic group is the time when PD is started after the insertion of a catheter. Some studies recommend immediate start of PD after catheter insertion,[20] other studies recommend a waiting period of 3–5 days[23] while some authors suggest a waiting period of 2 weeks.[122122]
The limitation of the study is that 6 of the 17 studies included in the meta-analysis were non-randomized. The non-randomized studies could have contributed to bias due to uncaptured differences between the groups. Furthermore, the estimates generated were not adjusted and hence some confounding factors may have impacted negatively on the study. Nevertheless, despite the limitations, the meta-analysis provides meaningful information regarding complications associated with laparoscopic and open-surgery PDC placement procedures.
Conclusion
The present study shows that there was statistically significant difference in catheter malfunction between the laparoscopic and open-surgery group. Furthermore, there were no statistically significant differences in dialysate leakage, peritonitis and exit-site infection between the laparoscopic and open-surgery PDC placement procedures.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Prospective randomized study for comparison of open surgery with laparoscopic-assisted placement of Tenckhoff peritoneal dialysis catheter-a single center experience and literature review. J Surg Res. 2010;159:489-96.
- [Google Scholar]
- Who Shouldn ' t Get a Percutaneous PD Catheter ? Improving clinical outcomes with optimal patient selection and percutaneous techniques for peritoneal dialysis Endovasc Today. 2014
- [Google Scholar]
- Relative survival of peritoneal dialysis and haemodialysis patients: Effect of cohort and mode of dialysis initiation. PLoS One. 2014;9:1-10.
- [Google Scholar]
- A comparative analysis of percutaneous and open surgical techniques for peritoneal catheter placement. Perit Dial Int. 2012;32:628-35.
- [Google Scholar]
- Surgical complications of Tenckhoff catheters used in continuous ambulatory peritoneal dialysis. Singapore Med J. 2006;47:707-11.
- [Google Scholar]
- Mini-laparoscopy-assisted placement of tenckhoff catheters: An improved technique to facilitate peritoneal dialysis. J Endourol. 2002;16:1-4.
- [Google Scholar]
- Laparoscopic internal fixation is a viable alternative option for continuous ambulatory peritoneal dialysis catheter insertion. J Korean Surg Soc. 2012;83:381-7.
- [Google Scholar]
- The survival and complication rates of laparoscopic versus open catheter placement in peritoneal dialysis patients. Surg Laparosc Endosc Percutan Tech. 2015;25:440-3.
- [Google Scholar]
- Clinical epidemiology of infectious disease among patients with chronic kidney disease. Clin Exp Nephrol. 2018;23:437-47.
- [Google Scholar]
- Global trends in diabetes complications: A review of current evidence. Diabetologia. 2019;62:3-16.
- [Google Scholar]
- Laparoscopic omental fixation technique vs open surgical placement of peritoneal dialysis catheters. Surg Endosc. 2003;17:1749-55.
- [Google Scholar]
- Comparison of open and laparoscopic secure placement of peritoneal dialysis catheters. Surg Endosc. 2005;19:137-9.
- [Google Scholar]
- Randomized prospective comparison of laparoscopic and open peritoneal dialysis catheter insertion. Perit Dial Int. 1999;19:372-5.
- [Google Scholar]
- Outcomes of laparoscopic and open CAPD catheter placement: A single-center experience. Surg Open Sci. 2019;1:20-4.
- [Google Scholar]
- Comparing the outcomes of open surgical procedure and percutaneously peritoneal dialysis catheter (PDC) insertion using laparoscopic needle: A two month follow-up study. J Res Med Sci Off J Isfahan Univ Med Sci. 2011;16:463.
- [Google Scholar]
- Laparoscopic versus open peritoneal dialysis catheter placement. Surg Endosc. 2016;30:899-905.
- [Google Scholar]
- Randomized controlled trial comparing open versus laparoscopic placement of a peritoneal dialysis catheter and outcomes: The CAPD I trial. Perit Dial Int. 2018;38:104-12.
- [Google Scholar]
- Effects of a novel peritoneal dialysis: The open versus laparoscopic preperitoneal tunneling technique. Ther Apher Dial. 2016;20:66-72.
- [Google Scholar]
- Peritoneoscopic versus surgical placement of peritoneal dialysis catheters: A prospective randomized study on outcome. Am J Kidney Dis. 1999;33:118-22.
- [Google Scholar]
- Laparoscopic placement of the tenckhoff catheter for dialvsis peritoneal. Surg Laparosc Endosc Percutan Tech. 2000;10:6-9.
- [Google Scholar]
- Peritoneal dialysis catheters: Laparoscopic versus traditional placement techniques and outcomes. Am J Surg. 2007;194:872-6.
- [Google Scholar]
- A laparoscopic method for optimal peritoneal dialysis access. Am Surg. 2005;71:135-43.
- [Google Scholar]
- Comparative experience of a simple technique for laparoscopic chronic ambulatory peritoneal dialysis catheter placement. Aust N Z J Surg. 1998;68:735-9.
- [Google Scholar]
- Peritoneal dialysis access: A comparison of peritoneoscopic and surgical insertion techniques. Scand J Urol. 1998;32:405-8.
- [Google Scholar]
- Comparison of peritoneal dialysis catheter insertion techniques: Peritoneoscopic, radiological and laparoscopic: A single-centre study. Nephrology. 2016;21:416-22.
- [Google Scholar]
- Laparoscopic placement of Tenckhoff catheters for peritoneal dialysis: A safe, effective, and reproducible procedure. Perit Dial Int. 2008;28:170-3.
- [Google Scholar]
- Laparoscopic versus open catheter placement in peritoneal dialysis patients: A systematic review and meta-analysis. BMC Nephrol 2012:13-69.
- [Google Scholar]
- Laparoscopic versus open peritoneal dialysis catheter insertion: A meta-analysis. PLoS One. 2013;8:56531.
- [Google Scholar]
- The curled catheter: Dependable device for percutaneous peritoneal access. Perit Dial Int. 1990;10:231-5.
- [Google Scholar]
- Percutaneous versus surgical insertion of PD catheters in dialysis patients: A meta-analysis. J Vasc Access. 2015;16:498-505.
- [Google Scholar]
- Catheter type, placement and insertion techniques for preventing peritonitis in peritoneal dialysis patients? Cochrane Database Syst Rev. 2010;2:1-54CD004680. doi: 10.1002/14651858.CD004680. pub2
- [Google Scholar]
- Antimicrobial agents to prevent peritonitis in peritoneal dialysis: A systematic review of randomized controlled trials. Am J Kidney Dis. 2004;44:591-603.
- [Google Scholar]







