Translate this page into:
A Unified Citywide Dashboard for Allocation and Scheduling Dialysis for COVID-19 Patients on Maintenance Hemodialysis
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
The coronavirus disease 2019 (COVID-19) pandemic has caused significant global disruption, especially for chronic care like hemodialysis treatments. Approximately 10,000 end-stage kidney disease (ESKD) patients are receiving maintenance hemodialysis (MHD) at 174 dialysis centers in Greater Mumbai. Because of the fear of transmission of infection and inability to isolate patients in dialysis centers, chronic hemodialysis care was disrupted for COVID-19-infected patients. Hence, we embarked on a citywide initiative to ensure uninterrupted dialysis for these patients.
Materials and Methods:
The Municipal Corporation of Greater Mumbai (MCGM) designated 23 hemodialysis facilities as COVID-positive centers, two as COVID-suspect centers, and the rest continued as COVID-negative centers to avoid transmission of infection and continuation of chronic hemodialysis treatment. Nephrologists and engineers of the city developed a web-based-portal so that information about the availability of dialysis slots for COVID-infected patients was easily available in real time to all those providing care to chronic hemodialysis patients.
Results:
The portal became operational on May 20, 2020, and as of December 31, 2020, has enrolled 1,418 COVID-positive ESKD patients. This initiative has helped 97% of enrolled COVID-infected ESKD patients to secure a dialysis slot within 48 hours. The portal also tracked outcomes and as of December 31, 2020, 370 (27%) patients died, 960 patients recovered, and 88 patients still had an active infection.
Conclusions:
The portal aided the timely and smooth transfer of COVID-19-positive ESKD patients to designated facilities, thus averting mortality arising from delayed or denied dialysis. Additionally, the portal also documented the natural history of the COVID-19 pandemic in the city and provided information on the overall incidence and outcomes. This aided the city administration in the projected resource needs to handle the pandemic.
Keywords
COVID-19
dashboard
end-stage kidney disease (ESKD)
hemodialysis
Mumbai
Project Victory
web-based portal
Introduction
The ongoing coronavirus disease 2019 (COVID-19) pandemic caused by the severe acute respiratory coronavirus 2 (SARS-COV-2) infection has affected all populations. Several global and national agencies have created virtual dashboards for reporting country-/city-specific data of COVID-19-infected patients. The outcomes of COVID-19 disproportionately affect vulnerable populations such as the elderly, obese, diabetic, and immunocompromised people. Patients with end-stage kidney disease (ESKD) are also at a higher risk for infection and mortality.[1] These patients are exposed to each other at dialysis facilities with limited social distancing. Managing maintenance hemodialysis (MHD) patients, therefore, remains a challenge due to the risk of cross-infection and the inability to isolate the infected patients. There is also an additional risk of death arising from missed dialysis due to inaccessible COVID-19-designated hemodialysis facilities.
India has 10.2 million confirmed cases of COVID-19 as of end of December 2020, with approximately 149,000 deaths. The city of Mumbai recorded 293,436 confirmed cases with 11,116 deaths on this date.[2] Mumbai is the sixth most populous city in the world with about 20 million inhabitants spread over 233 square miles (population density 73,000/square mile).[3] There are 174 hemodialysis facilities in Mumbai catering to about 10,000 estimated ESKD patients. Dialysis facilities in Mumbai operate on different models, including charitable trusts, government, municipal, and for-profit facilities. There is a wide disparity in the economic, educational, and social class of patients who are treated at these facilities. In the spring of 2020, the entire nephrology community of this metropolis was faced with twin problems – the high mortality associated with COVID-19 infection and the inability to manage the dialysis needs of an infected patient at the existing dialysis centers. The national lockdown in India initially resulted in the shutting down of some hospitals and lack of clear guidance to balance infection containment while maintaining life-saving treatments such as dialysis.[4] This was the stimulus to develop a solution to meet this unprecedented challenge. Hence, the local public health authority, the Municipal Corporation of Greater Mumbai (MCGM), intervened and designated certain dialysis facilities, strategically distributed across the city to treat only the COVID-positive/-suspect patients [Figure 1a]. But the onus of finding a suitable dialysis slot fell on the patients and their primary nephrologist. However, lack of information to direct a patient to an available slot at a specific facility caused widespread anxiety and led to chaos. Despite the mixed and fragmented model of dialysis services in Mumbai, the Nephrology community quickly responded by developing and deploying a strategic citywide dashboard with a focus on providing hemodialysis in a timely fashion to all COVID-19-infected ESKD patients across the city. [Appendix] We report on how this was developed and implemented with clinical outcomes.

- Distribution of hemodialysis facilities and COVID-19 patients on MHD across the city of Mumbai. (a) Hemodialysis facilities were strategically classified as COVID-19 positive/suspect/negative by the Municipal Corporation, to segregate and isolate COVID-19-infected patients. (b) The density of infected patients as depicted by the heat map mirrored the population density. (COVID-19, Coronavirus disease 2019; MHD, maintenance hemodialysis)
Materials and Methods
Development of portal and dashboard
A real-time web-based portal was developed to offer COVID-19-infected ESKD patients seamless and timely access to a COVID-19 (positive/suspect) dialysis facility within the city. This involved building an information technology (IT) framework that tracked real-time information on ESKD patients who tested positive.
The framework was deployed in the following stages.
Planning Stage: This coordinated effort was named “Project Victory.” The MCGM first designated 23 dialysis facilities as dedicated COVID-19 positive centers (11 public centers and 12 private centers), two as COVID-19 suspect centers (one public and one private), and 149 as COVID-19 (negative) dialysis centers [Figure 1a]. An advisory was issued that all COVID-19, positive or suspect, ESKD patients need to be moved to these dedicated centers to continue their dialysis care. This initiative was communicated via messaging in the dedicated WhatsApp (WhatsApp Inc., Menlo Park, California) Mumbai Nephrology Group to all 160 nephrologists and 174 dialysis centers, wherein the concept was discussed and accepted by all members.
Establishment of a common portal: A coordination portal called Covidialysis (https://covidialysis.in) was set up. Later this portal was closed in Feb 2021, when it was not required. The portal was designed as a progressive web application accessible from a variety of operating systems. A team of engineers from the Indian Institute of Technology–Bombay (IITB) built, tested, improvised the portal, and created a dashboard for real-time graph generation from the data. A dashboard coordinator was identified who had a comprehensive view of all enrolled patients and available dialysis slots. His primary role was to meet the demand for dialysis slots for COVID-19 (positive/suspect) patients in the minimum possible time, in coordination with the persons in charge of the centers.
Registration and Communication: Each dialysis center was registered on the portal using a Google Form (Google Inc., Menlo Park, California), which included details of its location, capacity, and dialysis shifts. The designated person in charge of each center updated the portal with the patient data on a Google Form and could access it using a range of devices (laptops, tablets, or smartphones). These persons in-charge were responsible for transmitting information about new COVID-19 (positive/suspect) cases to the dashboard coordinator who guided the patient to a specified dialysis slot in the city.
As the portal evolved, a data analytics interface was incorporated. The results were visualized on a dashboard built using Redash (Redash Ltd., Tel Aviv, Israel). All tools that were used in putting together this platform were FOSS (Free and Open-Source Software).
Patient management and transfer
There were no uniform COVID-19 testing policies in dialysis centers in the city of Mumbai. Each center used its own discretion to test patients, either as a screening tool for all patients or testing only symptomatic ones. Once a COVID-19 (positive/suspect) patient was identified, the dashboard coordinator was notified, who promptly assigned the patient to an appropriate COVID-19 facility. Each patient was given the choice of COVID-positive facility (public/private) to be transferred to. This eliminated conflicts pertaining to payments. To handle COVID-19 (suspect) patients, the coordinator followed a similar procedure and accommodated them within the suspect centers until the test results became available, then they were triaged either to a COVID-19 (positive) facility or back to their home center based on the result. By capturing the PIN code of each patient registered on the portal, every attempt was made to accommodate these patients at the COVID-positive facilities closest to their respective home PIN codes. When there were bed availability issues, they were given more distant options. The MCGM made arrangements for dedicated COVID-positive vehicles to transport such patients. There were also private paid services available for the same. One of these available transportation options was adopted.
Until July 2020, the RT-PCR (reverse transcription polymerase chain reaction) test turnaround times (TAT) was 3 to 4 days. Later, as the TAT decreased to 24 hours, the need for suspect facilities waned, and by August 2020, few patients needed this service leading to decommissioning of machines at these suspect centers.
Once patients became noninfective, they were transferred back to their primary center. The duration of stay at the designated COVID-19 facility changed over time as the guidance changed from a test-based isolation to a symptom- and duration-based framework. Initially, every COVID-19 (positive) patient had to test RT-PCR negative before being transferred out of the COVID-19 (positive) facility.[5] However, in May 2020, this guideline was modified, and any COVID-19 (positive) patient who was asymptomatic and spent 14 days in the COVID-19 (positive) facility could be transferred back to their primary center without mandatory retesting. The citywide population density of COVID-19 (positive) patients on MHD is shown in Figure 1b. The schematic in Figure 2a depicts the process of universal screening of all patients at the dialysis centers, identification of symptomatic patients, and transferring them into COVID-19 (positive/suspect) facilities. Figure 2b depicts the transfer process of COVID-19 (positive) patients from the community dialysis centers into the designated COVID-19 (positive) facilities assisted by the portal.
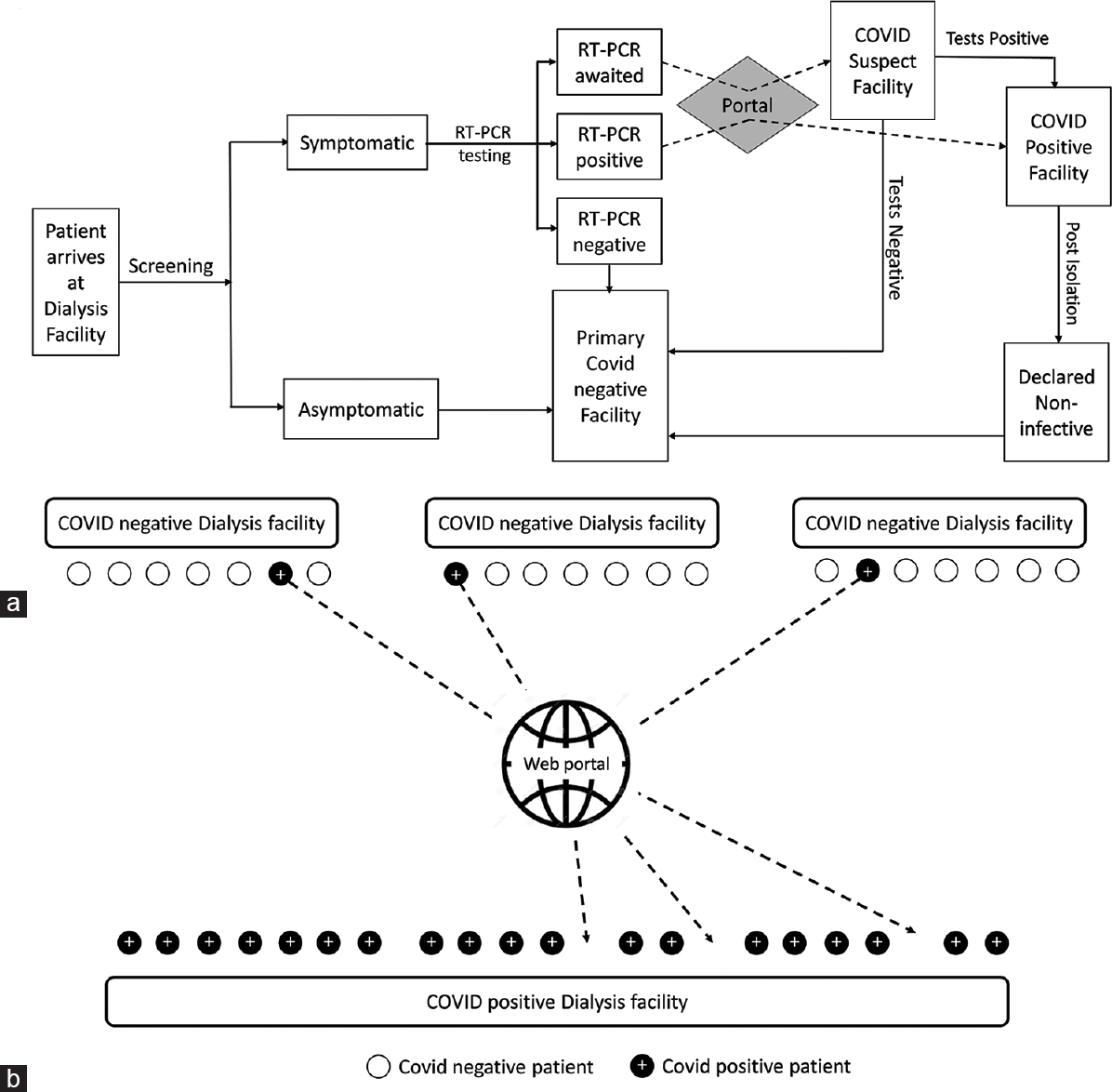
- COVID-19 positive/suspect MHD patient handling and assignment to designated hemodialysis facilities. (a) Flow diagram – primary screening, testing, enrollment, and transfer. (b) Schematic of portal-directed assignment of patients to designated hemodialysis facilities. (COVID-19, Coronavirus disease 2019; MHD, maintenance hemodialysis; RT-PCR, reverse transcription polymerase chain reaction)
Data collection, analysis, and outcome
Data collection: All clinical data (age; gender; comorbidities including hypertension, diabetes mellitus, and ischemic heart disease; and duration on dialysis), COVID-19 PCR status, testing dates, and hospitalization details were recorded. In addition, transfer dates, follow-up PCR test dates and transfers to primary dialysis units, and death data were also recorded. The dashboard captured data of the infected and suspect patients and documented their mortality, recovery, and activity status throughout the period of the pandemic. It also computed the efficiency of assigning COVID-19 (positive) patients to suitable dialysis centers. This provided precise data of case growth and projected resource needs. All collected data were stored in a PostgreSQL database management system on the Amazon Web Services (Amazon Inc., Seattle, Washington) cloud computing platform. The data presented in this study include all COVID-19 (positive) ESKD patients who were enrolled on the portal between May 20, 2020, and December 31, 2020. Institutional review board approval from IITB was taken to conduct this study.
Analysis: All continuous variables were described as mean with standard deviation, and categorical variables were described as frequency and percentages. The mortality rate was captured as a ratio of the number of deaths due to COVID-19 to the total number of COVID-19 (positive) cases. The analysis of outcomes between the survivors and non-survivors of COVID-19 infection in the ESKD population was done using the Fisher's exact test.
Outcomes: The data from the portal described the demographics of the affected population, mortality, risk factors, transfer time to designated dialysis centers, and the infection trend over time.
Oversight: The MCGM backed this effort. It sent a mandate to all dialysis centers to ensure compliance with full participation with this project.
Results
Study population
Of an estimated 10,000 ESKD patients on MHD in the city of Mumbai, 1,418 (14%) patients developed COVID-19 infection over the period of study. COVID-19-infected patients originated from 106 of the 174 (61%) hemodialysis facilities across the city and were transferred to 23 designated COVID-19 (positive) centers. Figure 1a shows the distribution of hemodialysis centers in the city. The heat map of the concentration of COVID-19 (positive) cases across the city is shown in Figure 1b. The origin of infected patients roughly mirrored the population density across the city. There were 870 men (61%, mean age = 56 ± 15 years) and 548 women (39%, mean age = 53 ± 13 years). Symptomatic patients constituted 67% of all infected patients.
Incidence of COVID-19 infection
The number of incident COVID-19 (positive) patients peaked by late June and declined thereafter. There have been minor spikes in the number of new cases during certain periods, without a noticeable second wave as of December 2020. The portal's primary objective was to allocate a COVID-19 (positive) hemodialysis slot to every enrolled patient. This was met within 24 hours for 73% patients, 48 hours for 97% patients, and 72 hours for all patients. As shown in Figure 3, there was an initial surge of COVID-19 (positive) cases in May, 2020. This was because of the inclusion of not just the incident but also the prevalent cases when the portal initially rolled out. Over time, there was a general decline in the number of new cases.

- Weekly enrollments of symptomatic/asymptomatic/suspect patients onto the portal
COVID-19 suspect cases
There were 156 patients who were COVID-19 (suspect) over the period, of which 78 (50%) eventually tested COVID-19 (positive).
Follow-up COVID-19 testing
During the study period, 47% of COVID-19 (positive) patients underwent retesting by RT-PCR based on the prevalent guidelines. In these patients, repeat COVID test was negative after a median of 12 days (interquartile range 7–20 days).
Outcomes
Outcomes over time in all patients are depicted in Figures 4a and 4b. Of the 1,351 patients with known outcomes, 370 died giving a mortality rate of 27% in COVID-19 (positive) patients on MHD. This is against a rate of 4% in the general population [Figure 4b].[2] The mean age of patients who died was 60 ± 13 years as compared with 52 ± 14 years in survivors. Time to death was 7 days (interquartile range 2–15). There was no statistical difference in mortality between the genders. Those patients who had one or more comorbidities (hypertension, diabetes, or ischemic heart disease) had a mortality of 51% as against 17% in those without comorbidities. Mortality figures varied among different COVID-19 (positive) health care facilities ranging from 20% to 48%.

- Outcomes of COVID-19 positive hemodialysis patients. (a) Cumulative number of enrollments, recoveries, deaths, and active patients over the study period. (b) Mortality rate due to COVID-19 infection in hemodialysis patients (blue curve) and in the general population (red curve) during the study period. (COVID-19, Coronavirus disease 2019)
COVID-19 infection among dialysis staff: The portal also gathered information on COVID-19 infection in hemodialysis personnel from 116/174 dialysis centers (67%). COVID-19 infection occurred in 191 of 1,725 hemodialysis personnel (11%) from these 116 centers, with no deaths.
Thus, our prospective study showed a COVID-19 infection rate of 14% among a large cohort of chronic MHD patients from multiple centers in a big metropolitan city. The mortality rate in this group was 27%. The IT platform and a collaborative approach between nephrologists with oversight from the city Municipal Corporation helped ensure the continuation of dialysis care for these patients.
Discussion
Across the world, dashboards have taken a center stage during the COVID-19 pandemic. The online interactive dashboard from the Johns Hopkins University, Baltimore, was the first such publicly shared resource.[6] It has helped researchers, public health authorities, and the public to visualize and track reported cases of COVID-19 infections and assisted with critical policy decision making as the outbreak unfolded.[78910]
We have previously reported a high incidence of infection among ESKD patients on MHD in Mumbai.[1] In this study, the crude incidence of COVID-19 is at least 14% with possible ascertainment bias due to changing testing criteria over time. The creation and deployment of the COVID-19 dashboard allowed the relatively seamless provision of dialysis services across the public and private sector dialysis facilities within the city, with 97% provision within 48 hours and 100% within 72 hours for all COVID-19 suspect and positive cases. This is in stark contrast to reports from other places in the country where approximately 28% patients missed one or more dialysis sessions, about 3% required emergency dialysis sessions, and about 4% stopped reporting for dialysis.[11] The portal closely tracked the outcomes of each of the 1,418 patients registered on it. It ensured that each one received timely dialysis. None of these patients, therefore, dropped out from dialysis owing to this appropriate and timely intervention.
The portal concurrently compiled data of these patients developing into a useful data resource for COVID-19 infection in hemodialysis patients in the city. In the present study, 1,418 COVID-19 (positive) ESKD patients in Mumbai constituted approximately 14% of all MHD patients and 0.48% of the total number of infected cases in the city as of December 31, 2020. The infection was reported from 61% of all hemodialysis centers in the city. The overall mortality of COVID-19 in this MHD setting was 27%, in line with the reported literature.
The incidence of COVID-19 in published literature varies from 2% (Wuhan) to 20% (London).[1213] The cumulative cases of COVID-19 in MHD patients in England ranged from 0.9% to 33% in the individual region/centers, with an overall incidence of 11%.[14] This variability could be dependent on the community prevalence, testing policies wherein all or only symptomatic patients were tested, and other confounding factors. There were no uniform COVID-19 testing policies in dialysis centers in the city of Mumbai. Each center used its own discretion to test patients, either as a screening tool for all patients or testing only symptomatic ones. Of the patients registered on the portal, 33% were asymptomatic. In the Brescia study, 19% of COVID-19 (positive) patients were asymptomatic.[15] This is in sharp contrast to a previous study from Mumbai where all dialysis patients were tested and 74% of infected patients were found to be asymptomatic.[1] It is yet unclear whether the proportion of symptomatic and asymptomatic patients is related to an impaired immune response due to underlying CKD.[16]
The time to retest negative after enrollment was 16 ± 14 days (median 12 days). A previous study in Mumbai that was done in the early epidemic period when retesting was the rule, reported a 96% viral clearance rate by Day 17.[1] Data from the United Kingdom reported that on retesting in MHD patients after COVID-19 diagnosis, only 59% tested negative by Day 15.[17] The available data suggest that prolonged viral RNA (ribonucleic acid) shedding after symptom resolution is not clearly associated with prolonged infectiousness and may reflect replication-incompetent SARS-CoV-2.[181920]
The mortality due to COVID-19 was 18% in the previous study done in Mumbai and 16% in the Wuhan study.[121] Several case series from Europe and the United States with varying follow-up suggest a high mortality rate in the dialysis population with rates ranging from 20% to 41%.[22232425] The mortality rate of 27% in MHD patients in our study captures a longer duration of the pandemic and a larger caseload than published data to date and is within the range reported from the high-income countries mentioned above.
The mortality rate was initially low when the portal was deployed in late May 2020 (5%) possibly due to more aggressive testing for the virus during this period with a dilution of the numbers from milder and asymptomatic cases that could lower the mortality rate.[2627] This reached a peak in July 2020 and then maintained a plateau until December 2020, when the rate stood at 27%. This stability of the number subsequently might also indicate a degree of expertise in handling these patients as well as standardization in testing protocols after July 2020.
It is now known that older age, cardiovascular disease, diabetes, chronic respiratory disease, hypertension, and cancer are associated with an increased risk of death in COVID-19 infection.[28] Patients on MHD are at high risk as they share similar comorbidities.[29] In our study, patients who had at least one of three comorbidities (hypertension, diabetes, or ischemic heart disease) had a mortality of 51% as against 17% in those with none, reflecting published literature. The mortality in the top 10 hospitals that serviced the maximum number of COVID-19 (positive) patients ranged from 20% to 48%. This wide range in mortality could be attributed to a referral bias, overburdening of selective hospitals, and variation in treatment protocols.
Although 11% of the dialysis personnel contracted COVID-19 infection, none of them died. The Wuhan study had a lower rate of infection in hemodialysis staff (3%).[30] This higher infection rate among staff in our study is likely because it covered a longer duration of the epidemic (7 months) compared with the Wuhan study (2 weeks), as well as a higher community prevalence in Mumbai compared with Wuhan. Younger age and lack of comorbidities could potentially have contributed to the zero mortality in dialysis caregivers.
This report has certain inherent limitations. Patients with acute kidney injury due to COVID-19 were not included in this study. This study was focused on ESKD patients on MHD alone. We did not have the exact figure of the number of patients undergoing MHD in the city. Also, “Project Victory” was primarily aimed at ensuring the allotment of dialysis slots to COVID-19 (positive) ESKD patients; hence, the portal did not capture granular data on hospitalization or intensive care admissions, ventilator needs, or response to specific anti-COVID-19 therapies.
In conclusion, “Project Victory” is unique in being the only such citywide, centralized, large, collective effort utilizing a web-based portal to help COVID-19-infected MHD patients secure a quick dialysis slot. It has the largest number of reported cases of COVID-19 (positive) ESKD patients from a single city. This project has helped health care providers and administrators guide patients to access chronic MHD services efficiently. The overall incidence of infection was 14% with a mortality of 27% among COVID-19 positive cases. This mortality was due to the complications arising out of COVID-19 infection and not due to delayed or denied dialysis. With isolation, we may have prevented the patient-to-patient and patient-to-staff spread of the infection. The nephrology community and the city administration embraced this multidimensional initiative for a common cause, demonstrating the value of collaborative health care management during a pandemic.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to acknowledge the efforts of the dialysis staff and health care workers in the city, the Municipal Corporation of Greater Mumbai, and the Indian Institute of Technology, Bombay.
References
- From infection to immunity: Impact of COVID-19 across nine hemodialysis centers in Mumbai. Indian J Nephrol in press
- [Google Scholar]
- Adding insult to injury: Kidney replacement therapy during COVID-19 in India. Kidney Int. 2020;98:238-9.
- [Google Scholar]
- Discontinuation ofTransmission-Based Precautions and Disposition of Patients with COVID-19 in Healthcare Settings (Interim Guidance) Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/ disposition-hospitalized-patients.html
- [Google Scholar]
- John Hopkins University of Medicine. Global map. Accessed from: https://coronavirus.jhu. edu/map.html
- [Google Scholar]
- An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20:533-4.
- [Google Scholar]
- Responding to COVID-19: The UW medicine information technology services experience. Appl Clin Inform. 2020;11:265-75.
- [Google Scholar]
- Open access epidemiologic data and an interactive dashboard to monitor the COVID-19 outbreak in Canada. CMAJ. 2020;192:E420.
- [Google Scholar]
- Digital technologies in the public-health response to COVID-19. Nat Med. 2020;26:1183-92.
- [Google Scholar]
- The adverse effect of COVID pandemic on the care of patients with kidney diseases in India. Kidney Int Rep. 2020;5:1545-50.
- [Google Scholar]
- Clinical characteristics of and medical interventions for COVID-19 in hemodialysis patients in Wuhan, China. J Am Soc Nephrol. 2020;31:1387-97.
- [Google Scholar]
- Epidemiology of COVID-19 in an urban dialysis center. J Am Soc Nephrol. 2020;31:1815-23.
- [Google Scholar]
- UKRR COVID-19 dataset. Available from: https://renal.org/audit-research/data-permissions/data/ ukrr-covid-19-dataset
- [Google Scholar]
- A report from the Brescia Renal COVID Task Force on the clinical characteristics and short-term outcome of hemodialysis patients with SARS-CoV-2 infection. Kidney Int. 2020;98:20-6.
- [Google Scholar]
- COVID-19 in dialysis patients: Adding a few more pieces to the puzzle. Kidney Int. 2020;98:17-9.
- [Google Scholar]
- De-isolation of COVID-19-positive hemodialysis patients in the outpatient setting: A single-center experience. Kidney Int. 2020;98:236-7.
- [Google Scholar]
- Viral load dynamics and disease severity in patients infected with SARS-CoV-2 in Zhejiang province, China, January-March 2020: Retrospective cohort study. BMJ. 2020;369:m1443.
- [Google Scholar]
- Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581:465-9.
- [Google Scholar]
- The natural history and transmission potential of asymptomatic SARS-CoV-2 infection. Clin Infect Dis. 2020;71:2679-87.
- [Google Scholar]
- 2019 novel coronavirus disease in hemodialysis (HD) patients: Report from one HD center in Wuhan, China. medRxiv 2020 doi: 10.1101/2020.02.24.20027201
- [Google Scholar]
- COVID-19: Clinical course and outcomes of 36 hemodialysis patients in Spain. Kidney Int. 2020;98:27-34.
- [Google Scholar]
- Management of hemodialysis patients with suspected or confirmed COVID-19 infection: Perspective from the Spanish nephrology. Kidney360. 2020;1:1254-8.
- [Google Scholar]
- Results from the ERA-EDTA Registry indicate a high mortality due to COVID-19 in dialysis patients and kidney transplant recipients across Europe. Kidney Int. 2020;98:1540-8.
- [Google Scholar]
- Presentation and outcomes of patients with ESKD and COVID-19. J Am Soc Nephrol. 2020;31:1409-15.
- [Google Scholar]
- Estimation of global case fatality rate of coronavirus disease 2019 (COVID-19) using meta-analyses: Comparison between calendar date and days since the outbreak of the first confirmed case. Int J Infect Dis. 2020;100:302-8.
- [Google Scholar]
- John Hopkins University of Medicine, 2020. Available from: http://coronavirus.jhu.edu/data/ mortality
- [Google Scholar]
- Characteristics of and important lessons from the Coronavirus Disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239-42.
- [Google Scholar]
- Managing the COVID-19 pandemic: International comparisons in dialysis patients. Kidney Int. 2020;98:12-6.
- [Google Scholar]
- Aggressive quarantine measures reduce the high morbidity of COVID-19 in patients on maintenance hemodialysis and medical staff of hemodialysis facilities in Wuhan, China. Kidney Dis. 2020;6:271-83.
- [Google Scholar]
Appendix:
Other members of the Mumbai Nephrology Group (Project Victory)
Shakir, Ahmad
Haridas, Ashwathy
Madan, Bahadur
Varun, Bansal
Vikas, Bharati
Amol, Bhawane
Harshal, Bhole
Nitin, Bhosale
Sandip, Bhurke
Pooja, Binani
Samuel, Chakola
Avinash, Chaudhari
Chandan, Chaudhari
Anup, Chaudhari
Hemant, Chaugule
Gaurav, Daga
Sudhiranjan, Dash
Keyur, Dave
Narendra, Dedhia
Paras, Dedhia
Jayesh D, Desai
Jayesh N, Desai
Rahul, Deshpande
Rushi, Deshpande
Martin, Desouza
Vaibhav, Dharap
Atit, Dharia
Haresh, Dodeja
Arun, Doshi
Rekha, Dubey
Bhupendra, Gandhi
Sohum, Gohil
Rajendra, Gunjotikar
Sachin, Gupta
Arun, Halankar
Atul, Ingale
Swapnil, Jadhav
Amit, Jain
Pankaj, Jawandhiya
Deepa, Jayaram
Makhija, Jhoomar
Vidya, Kadam
Shailesh, Kakde
Nikhil, Kedia
Vaibhav, Keskar
Jitendra, Khandge
Umesh, Khanna
Mustafa, Khokawala
Ashok, Kirpalani
Dilip, Kirpalani
Sachin, Kodgire
Amar, Kulkarni
Mihir, Kulkarni
Chaitanya, Kulkarni
Niranjan, Kulkarni
Arvind, Kunde
Siddharth, Lakhani
Amit, Langote
Dinesh, Mahajan
Jhoomar, Makhija
Raman, Malik
Hemant, Mehta
Mahendra, Merchant
Majid, Momin
Amit, Nagrik
Ravindra, Nikalji
Atim, Pajai
Aashay, Pandya
Harish, Pathak
Amjadkhan, Pathan
Ashwin, Patil
Rohan, Pradhan
Mahesh, Prasad
Prashant, Rajput
Akash, Ranka
Alka, Rao
Ramesh, Rao
Ruchi, Samdhani
Salman, Sayyed
Neha, Shah
Sohil, Shah
Arun, Shah
Bharat, Shah
Hemal, Shah
Rechal, Shah
Hardik, Shah
Wasiyeeullah, Shaikh
Suyash, Sharma
Mukesh, Shete
Sharad, Sheth
Ashay, Shingare
Abhishek, Shrikhande
Anurag, Shukla
Akash, Singhada
Nitin, Sonawane
Lohitaksh, Suratkal
Rudramani, Swami
Shruti, Tapiawala
Aseem, Thamba
Parag, Tilve
Kirti, Upadhyay
Deepa, Usulumarthy
Bhavesh, Vora
Harshal, Vora
Sameer, Vyahalkar
Menal, Wali
Jyotsna, Zope







