Translate this page into:
A case of Intravascular Lymphoma Masquerading as Calciphylaxis in a Patient on Haemodialysis
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Intravascular large B-cell lymphoma (IVLBCL) is a rare lymphoma entity with intravascular proliferation of clonal lymphocytes restricted to the lumen of small- and medium-sized blood vessels. In this case report, we describe a 70-year-old lady on maintenance hemodialysis who presented with altered sensorium and painful lesions over her inner thigh. While preliminary investigations were favoring calciphylaxis, it was the skin biopsy that showed vasculopathic lymphoid infiltrate with focal panniculitis, consistent with intravascular lymphoma. Although overall survival is poor, prompt use of intensive therapies have shown to improve the outcome.
Keywords
Calciphylaxis
hemodialysis
intravascular lymphoma
Introduction
Intravascular large B-cell lymphoma (IVLBCL) is a rare lymphoma entity with intravascular proliferation of clonal lymphocytes restricted to the lumen of small- and medium-sized blood vessels.[1] The presenting symptoms are nonspecific with most patients presenting with B symptoms, namely fever, night sweats, and weight loss. We report a case of IVLBCL presenting in a patient with clinical and laboratory features of calcific uremic arteriolopathy with a background of end-stage renal disease.
Case Report
A 70-year-old lady was admitted to the intensive care unit with altered sensorium and one episode of hypotension following her hemodialysis session. Her family gave a history of fever 2 days prior to this episode. Her background problems included diabetes mellitus type 2, essential hypertension, and chronic kidney disease. She had been recently commenced on hemodialysis. She had been hospitalized 1 month ago with volume overload and worsening renal parameters in view of which she had been started on hemodialysis. There were tender swellings over both her inner thighs and buttocks which had worsened over the past month. She had been advised punch biopsies from these lesions but the family had declined to have it done at that time.
On admission, this lady was found to be awake but confused and disoriented to time, place, and person. No obvious focal neurological deficit could be delineated. Her pulse rate was 110/min, blood pressure was 70/50 mm Hg, SPO2 was 98% in room air, and she was afebrile. Bilateral basal crepitations were noted on auscultation of the chest. Examination of skin over thighs revealed violaceous nodules with indurations that were extremely tender to palpation with overlying retiform purpura [Figure 1].

- Violaceous nodules with overlying retiform purpura over both inner thighs
Her preliminary investigation revealed a hemoglobin of 6.6 g/dl, total leucocyte count of 25.0 thou/cumm with neutrophilic leukocytosis, erythrocyte sedimentation rate of 119 mm/1st hour, c-reactive protein of 247 mg/L, serum albumin 1.01 g/dl, corrected serum calcium of 11.08 mg/dl, serum phosphate of 4.95 mg/dl, calcium phosphate product of 54.8, PTH 20.0 pg/ml, and creatine phosphokinase of 57 U/L. Venous Doppler of both lower limbs revealed subcutaneous edema with no evidence of deep vein thrombosis. Magnetic resonance imaging of both lower limbs suggested subcutaneous fat reticulation, edema, and soft tissue changes related to lipodermatosclerosis. A positron emission tomography scan was done which showed metabolically inactive subcutaneous fat stranding in bilateral thighs, likely panniculitis, and no evidence of metabolically active disease anywhere else. ANA profile, p ANCA, c ANCA, and APLA IgM were negative. A serum protein electrophoresis with immunophenotyping revealed an IgG kappa monoclonal band. Bone marrow aspiration cytology showed plasma cell <10%, and she was considered to have monoclonal gammopathy of uncertain significance (MGUS).
In view of the site and features of the lesions, in the background of CKD with hypercalcemia, low PTH, calcium phosphate product of 54.8, and hypoalbuminemia, a clinical diagnosis of calciphylaxis was made. She was commenced on empirical IV antibiotics (meropenem and vancomycin). Later, an antifungal agent, micafungin, was added. Due to worsening sepsis and persistent hypotension, she was commenced on intravenous colistin. Blood and urine cultures were sterile. She was also treated with calcitonin and zoledronic acid and continued on alternate-day hemodialysis with low calcium dialysate. She was also administered intravenous vitamin K. However, there was no improvement in symptoms. Subsequently, multiple punch biopsies were taken from the lesions after obtaining consent from the family. The biopsy finally revealed vasculopathic lymphoid infiltrate with focal panniculitis [Figure 2], with no specific deposits on diffuse immunofluorescence, which was consistent with intravascular lymphoma.
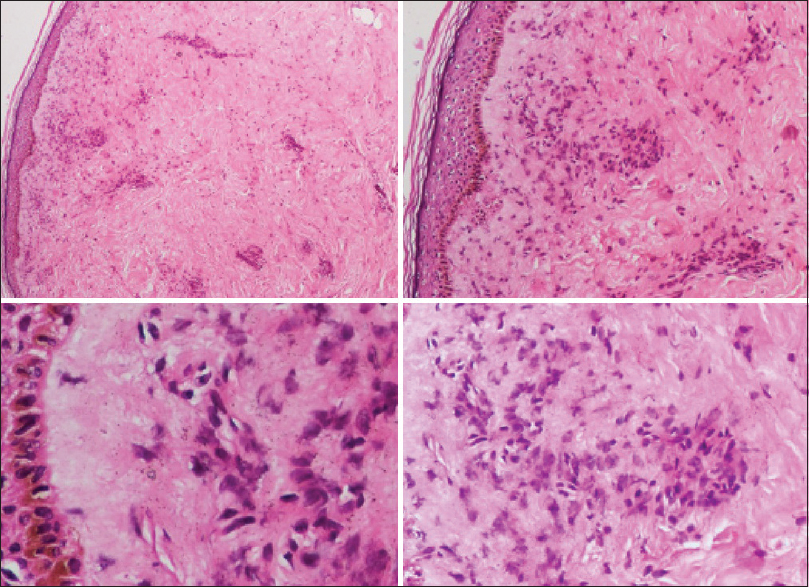
- Vasculopathic lymphoid infiltrate with focal panniculitis
She went into refractory septic shock. She was administered intravenous hydrocortisone 50 mg 6-hourly. Her family did not wish for any escalation of therapy. Over the next few days, there was very rapid deterioration of sensorium and she eventually expired.
Discussion
Intravascular lymphoma (IVL) or the oncologist's “great imitator” is a rare, clinically aggressive lymphoma characterized by an almost exclusive growth of large cells within the lumen of all-sized blood vessels. The reasons for this peculiar localization of neoplastic cells are only partially understood.[2] Pfleger and Tappeiner originally described IVL as a cutaneous small-vessel neoplasm because of the predilection for skin involvement.[1] It is a unique subset of diffuse large B-cell lymphoma (DLBCL), which is characteristically confined to intravascular spaces such as venules, capillaries, and arterioles but not large arteries and veins and hence called neoplasm of “homeless” lymphocytes. It involves extra-nodal organs such as kidneys, lungs, brain, spinal cord, and skin, but lymph nodes, spleen and bone marrow are generally spared. Clinically, the classical variant presents with many nonspecific signs and symptoms such as fever of unknown origin and involvement of the central nervous system and skin. Cases that show disease limited to the skin following extensive staging workup are called cutaneous variants and show a better prognosis.
Laboratory findings include anemia (63%), thrombocytopenia (29%), or leucopenia (24%). The erythrocyte sedimentation rate may be elevated in 43% cases, hypoalbuminemia may be seen (18%), and a monoclonal serum component is present in 14% of cases. Further, 15% of patients show altered hepatic, renal, or thyroid function.[2] In this case, the antecedent bone marrow aspiration did not reveal any evidence of a lymphoproliferative disorder. Her serum protein electrophoresis immunohistochemistry had revealed an IgG kappa monoclone, which was probably secondary to the IVL.
This lady presented as panniculitis. There have been sporadic case reports of IVL presenting as panniculitis. Demirer et al.[3] reported a case of a 61-year-old male patient who was diagnosed with Kaposi sarcoma of the lower extremity. He presented with rapidly growing, pigmented skin nodules on the extremities. Despite targeted treatment, he succumbed. An autopsy revealed diffuse IVL involving the skin, liver, and spleen.[3] Maiolo et al.[4] reported a case of intravascular large B-cell lymphoma in a 77-year-old Iranian woman who presented with a 3-month history of painful abdominal and inframammary subcutaneous nodules. Phoon et al.[5] reported another case of intravascular large B-cell lymphoma that presented as tender indurated non-ulcerated nodules located bilaterally over the calves without lymphadenopathy.
The clinicopathological characteristics of 38 human immunodeficiency virus-negative patients with IVL were reviewed by Ferreri et al.[6] who found the brain and skin to be the most common sites of disease. Further, patients with disease limited to the skin (“cutaneous variant”; 26% of cases) were invariably females with a normal platelet count and exhibited a significantly better outcome than the remaining patients. Overall survival was usually poor; however, the early use of intensive therapies could improve the outcome in young patients with unfavorable features.
This case presented with fever, nonspecific neurological symptoms (altered sensorium), and tender nodular cutaneous lesions. She was found to have elevated serum calcium, hypoalbuminemia, low PTH (probable adynamic bone disease), and classical painful nodular lesions in adipose abundant areas which was presumed to be due to calcific uremic arteriolopathy in the background of end-stage renal disease. The abnormal laboratory findings and hematological parameters did not prompt a suspicion of lymphoma as these findings were nonspecific and can present in both diseases. Diagnosing IVLBCL in these patients can be challenging and can only be done by histopathological examination of a tissue biopsy.
Conclusion
In a patient with end-stage renal disease presenting with clinical signs suggestive of calciphylaxis, IVLBCL must be considered in the differential diagnosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Intravascular large B-cell lymphoma presenting as cutaneous panniculitis. Acta Medica (Hradec Králové). 2003;46:121-3.
- [Google Scholar]
- Intravascular large B-cell lymphoma: A chameleon with multiple faces and many masks. Blood. 2018;132:1561-7.
- [Google Scholar]
- Four varied cases of intravascular lymphomatosis and a literature review. Cancer. 1994;73:1738-45.
- [Google Scholar]
- Intravascular large B-cell lymphoma presenting as panniculitis. JAAD Case Rep. 2017;3:536-8.
- [Google Scholar]
- Intravascular large B-cell lymphoma presenting as panniculitis clinically: A case report. Singapore Med J. 2018;59:163-64.
- [Google Scholar]
- Intravascular lymphoma: Clinical presentation, natural history, management and prognostic factors in a series of 38 cases, with special emphasis on the 'cutaneous variant' Br J Haematol. 2004;127:173-83.
- [Google Scholar]







