Translate this page into:
Diagnostic Dilemma: Cardiorenal Syndrome As an Unusual Presentation of IgG4-Related Disease
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
IgG4-related kidney disease (IgG4 RKD) is a rare clinical entity characterized by lymphoplasmacytic infiltration rich in IgG4-positive plasma cells along with fibrosis affecting several organs. Tubulointerstitial nephritis is commonly the predominant finding on kidney biopsy. Our patient was admitted with a provisional diagnosis of cardiorenal syndrome of unknown etiology. The patient was dialysis dependent for around 45 days following which kidney biopsy revealed features of acute tubulointerstitial nephritis (ATIN) with IgG4-positive plasma cells and no glomerular involvement. Positron emission tomography–computed tomography was supportive of findings of sialadenitis along with myocarditis. Our patient responded to treatment with steroids with definitive improvement in both renal and cardiac functions. This case highlights the importance of IgG4 RKD as an important differential in patients with ATIN presenting as a clinical syndrome.
Keywords
ATIN
IgG4-related kidney disease
myocarditis
PET-CT
sialadenitis
Introduction
IgG4-related disease (IgG4 RD) is a recently recognized entity with tumefactive lesions, with dense lymphoplasmacytic infiltrate rich in IgG4 plasma cells along with fibrosis occurring in a synchronous or metachronous fashion. The disease mainly affects middle-aged to elderly males. The serum IgG4 is usually elevated, and a favorable response to corticosteroids is generally seen.[1] Our case emphasizes on the varied clinical presentation of IgG4 RKD with normal IgG4 levels, the relevance of biopsy and PET-CT in corroborating the diagnosis.
Case Report
A 62-year-old male from Ethiopia with a past history of diabetes and allergic rhinitis was admitted outside with complaints of cough associated with fever, breathlessness, and anasarca for more than 1 month. The patient was evaluated and found to have dilated cardiomyopathy (ejection fraction 15%) along with rapidly deteriorating renal function. Urine analysis revealed albumin 2+, red blood cells 10–15/high-power field (hpf), white blood cells 15–30/hpf. Urine culture was negative. The patient had previous records of normal renal functions, electrocardiogram (ECG), and echocardiography (ECHO) findings 3 months back. On presentation to our hospital, the patient had fluid overload along with anuria for which he was started on hemodialysis. Ultrasonography revealed mildly enlarged kidneys (right kidney 11.5 cm × 4.5 cm; left kidney 12.5 cm × 4.3 cm) with altered echogenicity. In view of active urinary sediments in the setting of rapidly progressive renal failure, a workup for rapidly progressive glomerulonephritis (antinuclear antibody, C3, C4, antineutrophillic antibody, antiglomerular basement membrane antibody) was done, which was negative. Viral markers including human immunodeficiency virus, hepatitis B surface antigen, and hepatitis C antibody were negative. The patient was planned for renal biopsy, but the patient was lost to follow-up. The patient presented to us again a month later. He was getting regularly dialyzed thrice a week outside and his urine output had improved to around 400 mL/day, although his renal functions remained deranged (creatinine 5 mg/dL). In view of persistent renal dysfunction, he underwent renal biopsy, which revealed morphologically normal glomeruli on light microscopy. There was predominant lymphoplasmacytic infiltration involving 35% to 40% of sampled renal tissue along with few scattered eosinophils. The tubules show patchy acute tubule injury. An occasional entrapped vein showed nonocclusive phlebitis. The interstitial fibrosis had a storiform pattern and involved 20% to 25% of involved renal tissue. On immunofluorescence immunoglobulins (IgA, IgG, and IgM) and complements (C3 and C4) were negative. IgG4 immunostain highlighted 25% to 30% of plasma cells, and 12 plasma cells/hpf were identified. No tubular basement membrane deposits were noted. Overall, biopsy features were consistent with the diagnosis of IgG4-related kidney disease (IgG4 RKD).
The patient underwent workup for the same. The serum IgG4 was normal, but serum IgE was elevated (880 IU/mL) without peripheral eosinophilia. Workup for IgG4 mimickers such as sarcoidosis and rheumatoid arthritis were negative. Repeat complement levels C3 70 mg/dL (90–180 mg/dL), C4 7.4 mg/dL (10–40 mg/dL) were low. Positron emission tomography–computed tomography (PET-CT) was done, which revealed diffuse uptake in the parotid and submandibular glands along with uptake in the left atrial chamber, which was suggestive of myocarditis that was corroborated by normal angiography, ECG findings of left bundle branch block, and raised cardiac enzymes. No evidence of malignancy was seen. The patient was not willing for any further parotid or endomyocardial biopsy.
A final diagnosis of Cardiorenal Syndrome Type 5 secondary to systemic IgG4 RKD was made. The patient was given intravenous pulse methylprednisolone 125 mg/day for three doses followed by oral prednisolone 40 mg/day. The patient responded to treatment, and his renal functions improved to 1.4 mg/dL after a month. Repeat ECHO was done at 3 months and the ejection fraction improved to 50%. The patient is now in remission after 6 months and has been advised to continue the long duration of low-dose steroids.
Discussion
IgG4 RD is a disease with multiorgan involvement characterized by the following histopathological features: lymphoplasmacytic infiltrate with IgG4-related plasma cells, obliterative phlebitis, and storiform fibrosis. IgG4 RD as a systemic entity was reported in the early 21st century, with the majority of the cases reported in the literature being from Japan.[2] IgG4 RKD has male predominance (73%–87%), and the average patient age is about 65 years. The most common lesion in IgG4 RKD is acute tubulointerstitial nephritis (ATIN).[3] Other renal manifestations include membranous nephropathy, pyelitis, and hydronephrosis due to retroperitoneal fibrosis[4] IgG4 RKD is a rare entity, and it occurs in 15% of patients with IgG4 RD. Two criteria have been proposed for IgG4 RKD: the Japanese Society of Nephrology and the Mayo Clinic criteria.[56] We have compared the clinicopathological presentation of our patient with the diagnostic features as per the Mayo Clinic criteria and the Japanese Study [Tables 12]. Our patient had biopsy features of ATIN with interstitial fibrosis as shown in Figure 1. Elevated serum IgG4 levels is one of the criteria for IgG4 RKD, although our patient had normal IgG4 levels. Serum IgG4 levels can be elevated in IgG4 mimickers such as sclerosing cholangitis, malignancy, and sarcoidosis, and also can be present in up to 5% of the normal population.[7] There have been case reports of IgG4-negative IgG4 RD in which the patients showed typical clinical, imaging, and histopathological features of IgG4 RD, despite normal serum IgG4 levels.[89] One of the possible explanations could be the “prozone effect.” This occurs due to excess antigen that inhibits agglutination, leading to artificially low serum levels of IgG4.[29]

- (a) Fibroinflammatory interstitial lesion (hematoxylin and eosin [H&E], 10 × magnification) (b) Lymphoplasmacytic inflammation with few scattered eosinophils with patchy acute tubular injury. (c) Storiform fibrosis with nonocclusive phlebitis as highlighted by arrow (H&E, 20× magnification). (d) Plasma cells are positive for IgG. (e) About 25% to 30% plasma cells are positive for IgG4 stain, and 12 IgG4 plasma cells/hpf are identified (immunohistochemistry, 20× magnified)
| Our patient | Inoue D et al | |
|---|---|---|
| Sex | Male | Predominantly male |
| Age | 60 Yrs. | 50-70 Yrs. (Predominantly) |
| Common underlying etiolgies | Diabetes, allergic rhinitis | Diabetes >allergies |
| Clinical presentation | Subacute/rprf | Subacute |
| Organ involvement | Atin, sialadenitis | Aip >atin >sialadenitis >dacroadenitis |
| Cardiac -myocarditis | Cardiac-periaortitis (pericarditis, as per studies) | |
| Mediastinal lymphadenopathy | Lymphadenopathy-mediastinal, paraortic |
AIP: Autoimmune Pancreatitis, ATN - Acute Tubulointerstitial nephritis
| Clinical/radiological findings | Mildly enlarged kidneys, sialedenitis | Diffuse/localised swellings in organs/cortical nodules |
|---|---|---|
| Elevated serum IgG4 levels (> 135 mg/dl) | Absent | Present |
| Histopathological features of atin (a & b mandatory) | ||
| a) lymphoplasmacytic infiltration | Present | Present |
| b) >10 IgG4 positive plasma cells/hpf | Present | Present |
| IgG4 positive/IgG plasma cells>40% | Present | Present |
| Phlebitis | Present | Present |
| Tissue eosinophillia | Present | Present |
| Fibrosis | Minimal present (<20%) | Present |
| Others | ||
| Complements (c3, c4) | Low | Low |
| Serum IgE elevated | 880 | >350 |
PET-CT without contrast was done to look for any systemic manifestation of possible IgG4 RD. Diffuse fluorodeoxyglucose (FDG) uptake was noticed in the parotid and submandibular glands suggestive of sialadenitis [Figure 2]. Also, the patient had discrete mediastinal lymphadenopathy. As per the study by Zhang et al.,[10] the role of FDG PET-CT has been conclusively demonstrated in diagnosing IgG4 RD. Sialadenitis has been labeled as a strong-level recommendation, whereas lymphadenopathy as a moderate-level recommendation, indicative of IgG4 RD. PET-CT apart from diagnosis can also be used for monitoring therapeutic response and guiding interventional treatment of IgG4 RD.
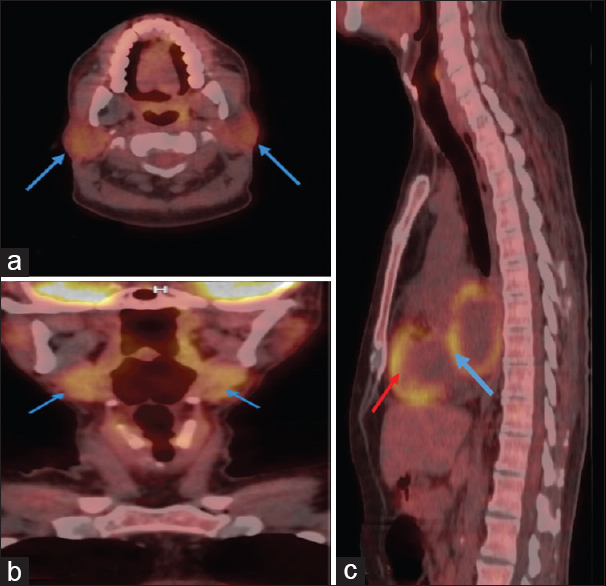
- (a and b) depict diffuse fluorodeoxyglucose (FDG) uptake (blue arrows) in the parotid and submandibular glands, respectively, suggestive of sialadenitis. (c) shows normal FDG uptake in the left ventricle (red arrow) as compared with abnormal uptake in the left atrium (blue arrow) suggestive of myocarditis
Our patient had global hypokinesia (ejection fraction 15%) on ECHO with raised cardiac enzymes. The patient underwent angiography to rule out the ischemic cause, which was normal. So, a possibility of inflammatory myocarditis was kept. Cardiovascular involvement can manifest as inflammatory periaortitis, aortic aneurysms, coronary arteritis, or pericarditis.[11] As per literature, FDG uptake is normally seen in ventricles, but uptake in the wall of atrial chambers does not occur. FDG uptake in the left atrium as shown in our patient [Figure 2] could be suggestive of myocarditis.[12] Thus, PET-CT findings further corroborated the underlying possibility of myocarditis. Myocarditis is a rare manifestation of IgG4 RD, and one case report of isolated myocarditis has been recently published.[13]
The optimal treatment for IgG4 RD is unknown. As per the recent International Consensus guidelines for the management of IgG4 RD,[14] the treatment is divided into induction phase with prednisolone, followed by tapering with steroids over 3 to 6 months, and then maintenance phase, which comprises low-dose steroids or steroid-sparing therapies. Steroid-sparing therapy comprises conventional drugs such as azathioprine, mycophenolate mofetil, or B-cell depleting therapies such as rituximab, which can also be tried in relapsing disease. Because our patient was dialysis dependent with features of severe ATIN, we pulsed him with methylprednisolone followed by oral steroids (prednisolone 40 mg/day). The patient responded to treatment and became dialysis independent. After 3 months of therapy, his complement levels came back to normal. Currently, after 6 months of therapy, the patient is in remission on low-dose prednisolone (5 mg/day) with a significant improvement in cardiac functions. The timeline of events is depicted in Figure 3.
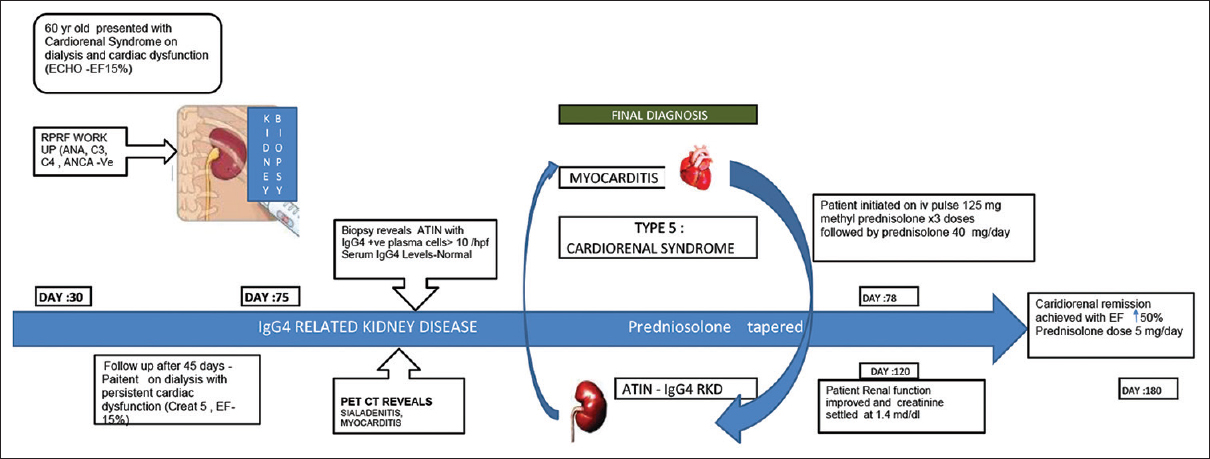
- Timeline of events of the patient
In conclusion, our patient had a cardiorenal presentation of IgG4 RD with myocarditis as an unusual feature, which responded to treatment with steroids. IgG4 RKD is still a newly recognized entity with diverse clinical presentation and requires further studies to have a better understanding of the disease. PET-CT is an innovative tool that along with kidney biopsy helps in corroborating the diagnosis of IgG4 RD.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- A novel clinical entity, IgG4-related disease (IgG4RD): General concept and details. Mod Rheumatol. 2012;22:1-14.
- [Google Scholar]
- Diagnostic approach to the complexity of IgG4-related disease. Mayo Clin Proc. 2015;90:927-39.
- [Google Scholar]
- Clinicopathological characteristics of patients with IgG4-related tubulointerstitial nephritis. Kidney Int. 2010;78:1016-23.
- [Google Scholar]
- Immunoglobulin G4-related kidney diseases: An updated review. World J Nephrol. 2018;7:29-40.
- [Google Scholar]
- IgG4-related disease: Dataset of 235 consecutive patients. Medicine (Baltimore). 2015;94:e680.
- [Google Scholar]
- Spectrum of disorders associated with elevated serum IgG4 levels encountered in clinical practice. Int J Rheumatol. 2012;2012:232960.
- [Google Scholar]
- IgG4-related kidney disease—An update. Curr Opin Nephrol Hypertens. 2015;24:193-201.
- [Google Scholar]
- IgG4-related kidney disease: A curious case of interstitial nephritis with hypocomplementemia. Case Rep Nephrol Dial. 2019;9:49-54.
- [Google Scholar]
- Characterizing IgG4-related disease with 18 F-FDG PET/CT: A prospective cohort study. Eur J Nucl Med Mol Imaging. 2014;41:1624-34.
- [Google Scholar]
- IgG4-related cardiovascular disease. The emerging role of cardiovascular imaging. Eur J Radiol. 2017;86:169-75.
- [Google Scholar]
- Utility of FDG PET/CT in inflammatory cardiovascular disease. Radiographics. 2011;31:1271-86.
- [Google Scholar]
- Isolated immunoglobulin G4-related disease myocarditis treated with heart transplantation. Circ Heart Fail. 2020;13:e007204.
- [Google Scholar]
- International consensus guidance statement on the management and treatment of IgG4-related disease. Arthritis Rheumatol. 2015;67:1688-99.
- [Google Scholar]







