Translate this page into:
Assessing the Practice of Infection Control Among Dialysis Staff in Dialysis Centers in Northeast India
Corresponding author: Loukrakpam Sharatchandra Singh, Department of Nephrology, Regional Institute of Medical Sciences, Imphal, Manipur, India. E-mail: loukra19@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Singh TB, Hulang BJ, Singh LS, Singh A, Misra S, Bhagat S, et al. Assessing the Practice of Infection Control Among Dialysis Staff in Dialysis Centers in Northeast India. Indian J Nephrol. doi: 10.25259/ijn_573_23
Abstract
Background:
Chronic kidney disease patients on maintenance hemodialysis have multiple co-morbidities and high risk of infections. This study was conducted to assess the idea and practice of infection control measures in dialysis units in northeast India.
Materials and Methods:
This observational descriptive study was conducted among the participants of the 5th hemodialysis technician’s conference, held at Guwahati on 29 and 30th October 2022. Data was collected through questionnaire prepared from Center for Diseases Control and Prevention 2016 Infection Prevention and Control Assessment Tool for hemodialysis with some additional parameters.
Results:
A total of 200 dialysis staff working in different dialysis units of northeast India participated in the study. Among infection control practices, 38% of participants said that their centers had no dedicated area for parenteral medication preparation. Twenty two percent did not clean the dialysis machine after each session. Thirty percent of participants responded that they had no regular training for infection control practices. Sixteen percent reported inadequate hand hygiene facilities near waiting areas.
Conclusion:
Dialysis staff has a crucial role in providing good standard dialysis care in ESRD patients. Dialysis facilities should have written policies on infection prevention and control and provide regular training to dialysis staff.
Keywords
Infection
Hemodialysis
Dialysis staff
Introduction
Patients on maintenance hemodialysis (MHD) have multiple co-morbidities and high risk of infections. These can lead to costly consequences like hospital admissions, risk of hospital acquired infections and even death.1 Infection is the most common cause of hospitalization and second most common cause of mortality among dialysis patients.2 World Health Organization (WHO), Center for Diseases Control and Prevention (CDC) and Association of Professionals in Infection Control (APIC) address the best practice guidelines for infection control in dialysis units based on several evidence based guidelines and recommendations.3-5
The increased risk of contracting health-care-associated infections (HAIs) among hemodialysis (HD) patients are mainly due to immune compromised status, frequent and prolonged exposure of blood through the vascular access and extra-corporeal circuit, contaminated water, close proximity to other sick patients with infectious disease and frequent contact with healthcare workers.6 Other important factors that increase the risk of infection are non-adherence or a breakdown in the implementation of recommended practices, which may be a result of understaffing, inadequate training of staff and lack of necessary equipment.
HD units should have written policies for prevention of infection-related complications. Staff members should possess thorough knowledge of the correct dialysis techniques, medication related complications and its management and aseptic techniques.7
There have been no studies on infection control measures in dialysis facilities in northeastern India thus far. Therefore, this study was conducted to assess the idea and practice of infection control measures in dialysis units in northeast India.
Materials and Methods
This is an observational descriptive study that was conducted among the participants of the 5th Hemodialysis Technician’s Conference, which was held in Guwahati, Assam in India, on the 29th and 30th October 2022. Nearly 200 technicians participated in the conference from more than 30 different dialysis centers in the northeastern states of India. The participants consent was obtained. Data was collected through a questionnaire prepared from CDC 2016 infection prevention and control assessment tool for hemodialysis with some additional parameters.4
Questionnaire was made with an aim of assessing the basic knowledge of infection control practice, facilities and policies in HD units, with respect to the following two components: a) infection control and safety practice with respect to the staff and b) infection control facilities and policies in dialysis unit.
The statistical package for social sciences (SPSS version.26) was used for data entry and analysis. Data were presented in descriptive statistics and were analyzed in the form of frequencies and percentages.
Results
A total of 200 dialysis staffs working in different dialysis units of northeast India participated in the study. The male to female ratio of participant was 2.3:1 and the most common age group was 20–30 years (76%) [Table 1]. Eighty five percent (85%) of participants held diploma degree, whereas 13% were graduates in dialysis technology. Their working experience ranged between 1 and 12 years. Twenty five percent (25%) of the study participants had working experience from one to three years whereas 40% had experience from 9 to 12 years.
| Age group (years) | Male n (%) | Female n (%) | Total n (%) |
|---|---|---|---|
| 20–30 | 112 (56) | 40 (20) | 152 (76) |
| 30–40 | 20 (10) | 10 (5) | 30 (15) |
| 40–50 | 6 (3) | 8 (4) | 14 (7) |
| >50 | 2 (1) | 2 (1) | 4 (2) |
Seventy six (38%) of participants said that their centers had no dedicated area for parenteral medication preparation. Forty four (22%) participants did not clean dialysis machine after each session, whereas 24% were not recapping needle immediately after use [Table 2].
| Infection control practice | Yes n (%) |
|---|---|
| Vaccinated against Hepatitis B | 184 (92) |
| Needle recap immediately after use | 152 (76) |
| Sharp injury | 172 (86) |
| Ever had blood splash | 176 (88) |
| Use of alcohol-based hand rub | 180 (90) |
| Use of Apron/Head cover during HD | 184 (92) |
| Wash hand before examining the patient | 176 (88) |
| Use gloves during dialysis | 200 (100) |
| Dialyzer reuse in Hepatitis B, Hepatitis C and HIV | 0 |
| Parenteral medication preparation in dedicated area | 124 (62) |
| Cleaning dialysis machine after each session | 156 (78) |
| Use alcohol based chlorhexidine (0.5 %) as first line skin antiseptic agent during dressing changes of catheter | 200 (100) |
| Routinely apply antibiotic ointment or povidone to catheter | 200 (100) |
HD: hemodialysis; HIV: human immunodeficiency virus
The provisions available at HD centers for healthcare personnel safety varied considerably. Thirty percent (n = 60) of participants responded that they did not have regular training for infection control practices. Fifty six (28%) technicians said their facilities had no segregating facilities for symptomatic patients by 6 feet. Thirty two (16%) of participants said that facilities for hand hygiene were lacking near waiting areas [Table 3].
| Elements assessed | Yes n (%) |
|---|---|
| Providing personal protective equipment | 200 (100) |
| Post exposure evaluation and prophylaxis at free cost | 180 (90) |
| Hepatitis B vaccination to working personnel | 160 (80) |
| Facilities for hand hygiene in or near waiting areas | 168 (84) |
| Facility of facemask use upon entry to symptomatic patients | 200 (100) |
| Separate symptomatic patients by at least 6 feet from other patients | 144 (72) |
Figure 1 shows the different parameters in surveillance facilities and disease reporting pattern, including water quality monitoring and viral markers. In our study only, 80 (40%) staff members said that the blood culture was withdrawn before antimicrobial administration. Vascular access care and policies in HD units are shown in Table 4. Inadequate training with respect to environment cleaning and disinfection was found in 16% and 20%, respectively.
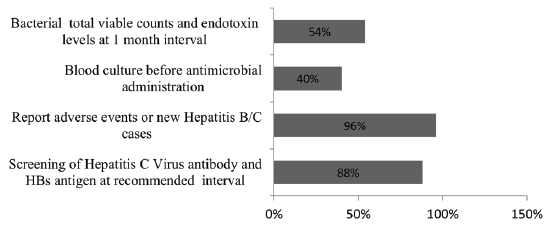
- Surveillance facilities and disease reporting (n = 200). HB: Hepatitis B.
| Elements assessed | Yes n (%) |
|---|---|
| Training of staff specific to catheter or vascular access care | 168 (84) |
| Written policies and procedures for routine cleaning and disinfection of environment surfaces | 180 (90) |
| Training of personnel on environment cleaning and disinfection | 160 (80) |
| Policy for decontamination of spill of blood or body fluid | 200 (100) |
| Policy/procedures for reusable medical devices | 200 (100) |
| Policies on dialyzer reuse | 200 (100) |
| Routine training for infection control practices | 140 (70) |
HD: hemodialysis
Discussion
Infection is the second most common cause of mortality among patients on MHD after cardiovascular disease.8 Noncompliance to infection control measures at dialysis unit could cause complications in both dialysis staff and patients.
The WHO has established guidelines on hand hygiene for health care professionals.9 Previous studies also have shown that major route of transmission of HAIs is through contaminated hands of the health care providers.10-18 In our study we found that 12% of the staff were not washing hand before procedure and 16% said that their center was lacking inadequate hand hygiene facilities. In a study done in Saudi Arabia also found that 15%–18% of total participants were not compliant to hand hygiene.19 This lack of compliance may be because of the fact that HD staffs need to perform hand hygiene multiple times during one session of dialysis, leading to work fatigue and shortage of time. Repeated training, provision of sufficient number of sinks with soap dispensers at appropriate locations and alcohol-based hand rubs placed at each patient station can improve the compliance.
Hospital acquired infection is transmitted by contaminated environmental surfaces with different pathogens.20 Microorganisms can survive on environmental surfaces for varying periods of time. Szewczyk et al. recommended that the disinfection of dialysis machine should be done after each dialysis session or after every 72 hours breaks in working.21 In this study, 22% of dialysis staffs were not following these recommendations. This may be due to lower educational status of participants (80% were only diploma holders) or because of excessive workload with time constraint. Education with regular trainings about the risk and benefit of disinfection to the staff as well as patients will solve these problems.
As per the guidelines by CDC and APIC medications packaged as multi-dose should be assigned to a single patient and preparation should be carried out in a clean area away from the patient treatment area, as well as patients should be segregated by minimum distance of 6 feet.22-24 In our study, dedicated area for parenteral medicine preparation was not assigned in 38%, and 28% of participants answered that there were no facilities for segregating symptomatic and asymptomatic patients. This may be due to failure of the hospital authority to provide adequate space and lack of knowledge on part of technicians. So a strict enforcement of guidelines for setting up of a new dialysis center in accordance with the national and international norms and adequate training will help in solving this problem.
Infection with tunneled dialysis catheters is found to be the leading cause for bacteremia in chronic HD patients.25 In this study, staff training with respect to catheter care was not given to 16% of the staff members. This may be because of lack of in house trainer on catheter care technique. So regular in-house training by a trained individual should be carried out.
Hepatitis B vaccination is recommended to susceptible healthcare workers in dialysis units.26 Ninety two percent (92%) of dialysis staff were vaccinated against hepatitis B in this study. Vaccine was provided by the HD facilities only in 80%. Written policies on control and prevention of infection, and blood sample collection before starting antibiotic therapy was lacking in 10% and 60% of the staff members, respectively. All HD facilities in charge should keep written policies for control and prevention of infection in dialysis unit to improve patient care.
In India, with implementation of the Pradhan Mantri National Dialysis Programme, there has been drastic increase in dialysis centers. However, these dialysis centers should strictly follow the guidelines laid down by the Indian Society of Nephrology for starting new standalone dialysis centers, so as to be able to give a standard care to patients as well as personal safety of the staffs.27 Training institute of dialysis technician should also strictly follow the minimum standards of teaching set by paramedical council of India.
Our study derives data covering most of the staff working in different dialysis facilities in northeast India and is the first study that has assessed infection control measures in this part of country. An important drawback of our study was that data was collected through questionnaire and there was no direct observations made over the infection control practices which could have resulted in information bias.
Conclusion
A dialysis staff has a crucial role in providing a good standard dialysis care in ESRD patients and an error in dialysis care can have various effects on patient health as well as on staff themselves. In our study, dialysis units were predominantly lacking in providing facilities of dedicated space for parenteral medication preparations, separation of symptomatic patients and providing vaccination of staff and periodic monitoring of water quality. They were also lacking in providing in house or otherwise training of staff about infection control practices. There should be regular training of dialysis staff on infection control practices. It is the cornerstone for risk reduction and improvement in survival in HD patients.
Conflicts of interest
There are no conflicts of interest.
References
- Adverse safety events in chronic kidney disease: The frequency of “multiple hits”. Clin J Am Soc Nephrol. 2010;5:95-101.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Maintaining safety in the dialysis facility. Clin J Am Soc Nephrol. 2015;10:688-95.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Infection prevention and control. Available from: https://www.who.int/teams/integrated-health-services/infection-prevention-control [Last accessed on 2023 Sep 6].
- Guideline, recommendations and resources. Available from: https://www.cdc.gov/dialysis/guidelines/index.html [Last accessed on 2023 Sep 7].
- Infection prevention and control dialysis settings. (2022). Available from: https://apic.org/implementation_guide/infection-prevention-and-control-in-dialysis-settings/ [Last accessed on 2023 Sep 7].
- Infection control in hemodialysis units: A quick access to essential elements. Saud J Kidney Dis Transpl. 2014;25:496-519.
- [CrossRef] [Google Scholar]
- How safe is renal replacement therapy? A national study of mortality and adverse events contributing to the death of renal replacement therapy recipients. Nephrol Dial Transpl. 2014;29:681-7.
- [CrossRef] [Google Scholar]
- Mortality caused by sepsis in patients with end-stage renal disease compared with the general population. Kidn Int. 2000;58:1758-64.
- [CrossRef] [Google Scholar]
- Infection prevention and control. Available from: https://www.who.int/teams/integrated-health-services/infection-prevention-control/hand-hygiene [Last accessed on 2023 Sep 7].
- Bacterial contamination of the hands of hospital staff during routine patient care. Arch Intern Med. 1999;159:821-6.
- [CrossRef] [PubMed] [Google Scholar]
- An epidemiological study assessing the relative importance of airborne and direct contact transmission of microorganisms in a medical intensive care unit. J Hosp Infect. 1990;15:301-9.
- [CrossRef] [PubMed] [Google Scholar]
- Improving adherence to hand hygiene practice: A multidisciplinary approach. Emerg Infect Dis. 2001;7:234-40.
- [CrossRef] [PubMed] [Google Scholar]
- Acquisition of nosocomial pathogens on hands after contact with environmental surfaces near hospitalized patients. Infect Control Hosp Epidemiol. 2004;25:164-7.
- [CrossRef] [PubMed] [Google Scholar]
- A causal link between hand washing and risk of infection? Examination of the evidence. Infect Control. 1988;9:28-36.
- [PubMed] [Google Scholar]
- Outbreaks of infection with methicillin-resistant Staphylococcus aureus on neonatal and burns units of a new hospital. Epidemiol Infect. 1990;105:215-28.
- [CrossRef] [PubMed] [Google Scholar]
- Nurses’ hands as vectors of hospital-acquired infection: A review. J Adv Nurs. 1991;16:1216-25.
- [CrossRef] [PubMed] [Google Scholar]
- Transfer of vancomycin-resistant enterococci via health care worker hands. Arch Intern Med. 2005;165:302-7.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with personal protection equipment use and hand hygiene among hemodialysis staff. Am J Infect Control. 2006;34:100-7.
- [CrossRef] [PubMed] [Google Scholar]
- Knowledge, attitudes and practice of nurses in renal dialysis units regarding infection control in Abha City – Saudi Arabia. Egypt J Hosp Med. 2017;66:103-14.
- [Google Scholar]
- Clinical practice guidelines for vascular access. Am J Kidn Dis. 2006;48 Suppl 1:S176-247.
- [Google Scholar]
- Are disinfectant residues remained after cleaning hemodialysis machine procedure safe for patients? Przegl Lek. 2013;70:97-101.
- [PubMed] [Google Scholar]
- Infection control requirements for dialysis facilities and clarification regarding guidance on parentral medication vials. MMWR Morb Mortal Wkly Rep. 2008;57:875-6.
- [PubMed] [Google Scholar]
- Association for professionals in infection control and epidemiology. Preventing infections in hemodialysis: An executive summary of the APIC Elimination Guide. Am J Infect Control. 2011;39:72-5.
- [CrossRef] [PubMed] [Google Scholar]
- Guideline for isolation precautions: Preventing transmission of infectious agents in healthcare settings. (2007). Available from: https://www.cdc.gov/infectioncontrol/guidelines/isolation/index.html [Last accessed on 2023 Sep 8]
- EPIBACDIAL: A multicenter prospective study of risk factors for bacteremia in chronic hemodialysis patients. J Am Soc Nephrol. 1998;9:869-76.
- [CrossRef] [PubMed] [Google Scholar]
- Immunization of Health-Care Workers: Recommendations of the Advisory Committee on Immunization Practices (ACIP) and the Hospital Infection Control Practices Advisory Committee (HICPAC). Available from: https://www.cdc.gov/mmwr/preview/mmwrhtml/00050577.html [Last accessed on 2023 Sep 8]
- Setting up of Hemodialysis Unit. Indian J Nephrol. 2020;30:S1-S5.
- [PubMed] [PubMed Central] [Google Scholar]







