Translate this page into:
Atenolol and amlodipine combination overdose managed with continuous venovenous hemodiafiltration: A case report
Address for correspondence: Dr. Ram Rapur, Department of Nephrology, SVIMS, Tirupati, Andhra Pradesh, India. E-mail: ram_5_1999@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
We present a patient of who ingested large dose of of atenolol and amlodipine and was treated successfully with continuous venovenous hemodiafiltration. Early recognition of indications for renal support and early initiation of the same is the key to successful management.
Keywords
Atenolol
amlodipine
continuous veno-venous hemodiafiltration
Mobitz type II block
Introduction
Of all the deaths due to overdosage of cardiovascular medications more than 65% are due to ingestion of β-blockers (BBs) and calcium channel blockers (CCBs).[1] Co-ingestion of BBs and CCBs is dangerous owing to the similar changes they produce in the physiology. We present a patient who consumed large doses of BB and CCB with suicidal intent. She was successfully managed by continuous veno-venous hemodiafiltration (CVVHDF).
Case Report
A 35-year-old female patient was brought to our institute with history of consumption of 100 tablets each of amlodipine besylate of 10 mg and atenolol of 50 mg with a suicidal intention. She was brought 8 h after the ingestion. She was in altered sensorium with E2, V2, M4 on Glasgow coma scale. Her blood pressure was 70/50 mm Hg, pulse rate 62 bpm, respiratory rate 32/min and axillary body temperature 96.5°F. There was tachycardia and tachypnea with prolonged expiration. She was immediately placed on a mechanical ventilator and started on adrenaline, dopamine and vasopressin. The investigations showed serum creatinine 2.5 mg/dl, blood urea 68 mg/dl, random blood glucose 109 mg/dl, serum bicarbonate 10.8 mEq/L and pH 7.14, electrocardiogram showed Mobitz type II AV block [Figure 1]. Later investigations showed serum sodium 134 mEq/L, potassium 4.3 mEq/L, calcium 7.5 mg/dl, phosphorus 5.0 mg/dl, hemoglobin 11.7 g/dl. Echocardiography showed no regional wall motion abnormality, normal left ventricular systolic function and ejection fraction of 60%.
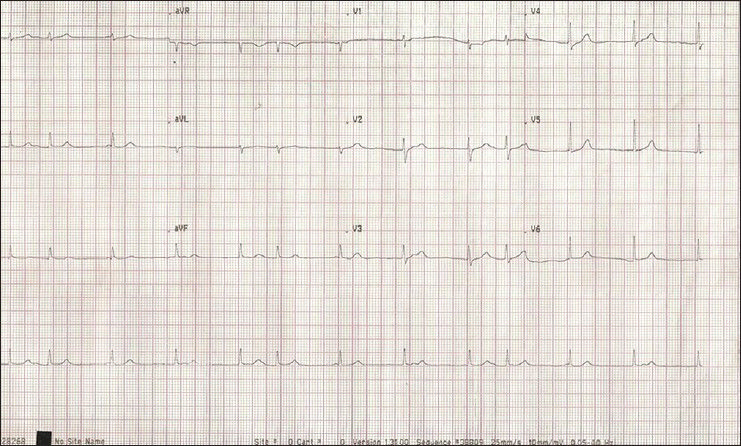
- Electrocardiogram: 2nd degree AV block, Mobitz type II
She was started on 10% solution of calcium carbonate, glucagon infusion at 5 mg/h for 20 h following the first 5 mg loading dose and regular insulin, 1 unit/kg loading dose followed by 0.5 unit/kg/h along with continuous infusion of glucose and potassium. Blood glucose was monitored once in 30 min and serum potassium was monitored for 6 h. Patient had no urine output for the first 6 h after admission. She had worsening metabolic acidosis and declining blood pressure despite these measures. She was initiated on CVVHDF. with a filter made of AN 69 membrane. The surface area of the membrane was 0.9 m2. The dose of continuous renal replacement therapy was 20 ml/kg/h and blood flow was 50 ml/min. Heparin was used as anticoagulation. All measures including CVVHDF were continued for 90 h after admission. The patient's sensorium and urine output improved gradually in these 90 h. The blood pressure normalized after intensive treatment for 120 h. Once the blood pressure returned to normal the pressors was discontinued and she was extubated. The serial values of serum creatinine after initiation of CVVHDF were 3.0, 2.8, 1.6 and 1.4 mg/dl.
Discussion
Cyclic AMP is the intracellular messenger of beta-stimulation; among its action is the “opening” of calcium channels to promote a positive inotropic effect.[2] The CCBs act by L-channel of calcium. The function of L-channel is to admit the substantial amount of calcium ions required for initiation of contraction via calcium induced calcium release from the sarcoplasmic reticulum.[3] The final effect of these two classes-BBs and CCBs of drugs is inhibition of calcium influx into cells. The consensus guidelines for toxic doses of BB and CCB have been published.[45] BBs with low lipid solubility that lack membrane stabilizing effects are safer so also the newer CCBs than the diltiazem and verapamil.[1678] The lowest reported toxic doses of common BBs and CCBs were reported recently. The lowest reported toxic dose of atenolol in for an adult was 500 mg and amlodipine was 30 mg.[9]
The presentation of combined BB and CCB overdose may have common manifestations such as hypotension and bradycardia.[9] The features such as bronchospasm, due to loss of β selectivity in overdose and central nervous system depression due to BB with lipophilicity are indicators of BB toxicity.[9] Carvedilol and propranolol are typically high lipid soluble whereas labetalol, metoprolol and pindolol are moderately lipid soluble and atenolol in low lipid soluble.[9] Prolonged QRS interval because of sodium channel block may also suggest BB toxicity. CCB overdose may result in sinus bradycardia and atrioventricular block.[8] Hyperglycemia is due to blocking of calcium influx into pancreatic cells which is required for the release of insulin.[10] The altered sensorium of our patient could be attributed to poor perfusion of the brain due to hypotension and not due to atenolol as the latter is not lipid soluble.
There were two reports[1112] of CVVHDF in combined BB and CCB overdose. The indications for performing CVVHDF in our patient were acute renal failure with anuria and metabolic acidosis with hypotension. The metabolic acidosis was due to lactic acidosis due to shock and acidosis due to acute renal failure. Ketoacidosis due to hyperglycemia could also be a cause but was not identified in this patient. The effluent dose was kept low owing to profound hypotension. The high protein binding (93%) nature of amlodipine makes it non-dialyzable.[13] Atenolol being only 10% protein bound can be removed by extracorporeal blood purification techniques.[714] High dose glucagon is recommended in cardiotoxicity due to BB because it activates adenylate cyclase in cardiac tissue by directly stimulating a G protein on the β receptor complex.[915] Insulin-dextrose-potassium infusion is effective in CCB overdose through enhanced cardiac carbohydrate metabolism and direct inotropic effects.[16]
We present a patient of co-ingestion of atenolol and amlodipine treated successfully with CVVHDF along with the other measures. Early recognition of indications for renal support and early initiation of the same is the key to successful management. Even if the drugs are not dialyzable the correction of electrolyte abnormalities, metabolic acidosis and thus hypotension improves the outcome.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Acute beta blocker overdose: Factors associated with the development of cardiovascular morbidity. J Toxicol Clin Toxicol. 2000;38:275-81.
- [Google Scholar]
- β.blocking agents. In: Opie LH, Gersh BJ, eds. Drugs for Heart (8th ed). Philadelphia, PA: Saunders; 2013. p. :1-37.
- [Google Scholar]
- Calcium channel blockers. In: Opie LH, Gersh BJ, eds. Drugs for Heart (8th ed). Philadelphia, PA: Saunders; 2013. p. :64-92.
- [Google Scholar]
- beta-blocker ingestion: An evidence-based consensus guideline for out-of-hospital management. Clin Toxicol (Phila). 2005;43:131-46.
- [Google Scholar]
- Calcium channel blocker ingestion: An evidence-based consensus guideline for out-of-hospital management. Clin Toxicol (Phila). 2005;43:797-822.
- [Google Scholar]
- The management of acute poisoning due to beta-adrenoceptor antagonists. Med Toxicol Adverse Drug Exp. 1989;4:32-45.
- [Google Scholar]
- Relative toxicity of beta blockers in overdose. J Toxicol Clin Toxicol. 1996;34:273-8.
- [Google Scholar]
- Treatment of poisoning caused by beta-adrenergic and calcium-channel blockers. Am J Health Syst Pharm. 2006;63:1828-35.
- [Google Scholar]
- High-dose insulin therapy for calcium-channel blocker overdose. Ann Pharmacother. 2005;39:923-30.
- [Google Scholar]
- Extra-corporeal life support for near-fatal multi-drug intoxication: A case report. J Med Case Rep. 2011;5:231.
- [Google Scholar]
- Successful treatment of a massive atenolol and nifedipine overdose with CVVHDF. Minerva Anestesiol. 2008;74:97-100.
- [Google Scholar]
- Refractory cardiogenic shock and complete heart block after unsuspected verapamil-SR and atenolol overdose. Clin Cardiol. 1991;14:933-5.
- [Google Scholar]
- Glucagon in beta-blocker and calcium channel blocker overdoses: A systematic review. J Toxicol Clin Toxicol. 2003;41:595-602.
- [Google Scholar]
- Beneficial myocardial metabolic effects of insulin during verapamil toxicity in the anesthetized canine. Crit Care Med. 1995;23:1251-63.
- [Google Scholar]







