Translate this page into:
Bartter's syndrome in a geriatric patient
Address for correspondence: Dr. R. Ram, Department of Nephrology, Sri Venkateswara Institute of Medical Sciences, Tirupati, Andhra Pradesh, India. E-mail: ram_5_1999@yahoo.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
A 62-year-old man presented with tingling sensation in the limbs and difficulty in getting up from squatting position for 2 years duration. He had episodic weakness of all limbs – a total of 7 during the last 2 years. He was treated with intravenous fluids with added injections after every episode, and improved over 2 days. There was no polyuria, passage of stone, or breathlessness, excess carbohydrate intake, exercise, diarrhea, diuretic, or over-the-counter medicine use. There was no family history of similar illness. His pulse was 80 bpm, and blood pressure was 110/70 mmHg. General and systemic examination was unremarkable. An ear-nose-throat specialist confirmed that there was no deafness. Investigations were hemoglobin 17.0 g/dl, serum creatinine 1.36 mg/dl, blood urea 35 mg/dl, serum potassium 2.3 mEq/L, sodium 140 mEq/L, calcium 9.4 mg/dl, phosphorus 2.2 mg/dl, uric acid 6.8 mg/dl, magnesium 2.2 mg/dl, renin activity 4.95 ng/ml/h (reference range on normal sodium diet supine 0.2–1.0 ng/ml/h and upright: 0.5–4.0 ng/ml/h), serum aldosterone 378 pg/ml (reference range: 25–315 pg/ml), 24 h urine potassium: 39 mmol (reference range: 10–20 mmol), 24 h urine calcium 301 mg (reference range: 100–250 mg), 24 h urine chloride 100 mmol (reference range: 10–20 mmol), serum pH 7.86, serum bicarbonate 61.5 mmol/l.
Computerized tomography of abdomen showed renal calculus disease on the right side [Figure 1]. The patient, therefore, had hypokalemia, metabolic alkalosis, hypercalciuria, high urine potassium and chloride excretion, high serum renin and aldosterone levels, and normal serum magnesium and renal calculus disease. The features suggested the diagnosis of Bartter's syndrome, type III. He was initiated on tablet spironolactone 25 mg/day, syrup potassium chloride, and liberal intake of fluids and diet rich in potassium. After 1-month, the reports were serum pH: 7.326, serum bicarbonate: 21.7 mmol/l, serum potassium: 4.3 mEq/L, and 24 h urine calcium: 150 mg.

- Computerized tomography of abdomen: Right renal calculus
Pseudo-Bartter's syndrome could be due to laxative abuse, furosemide abuse, bulimia, gentamicin nephrotoxicity, Sjogren's syndrome, and cystic fibrosis. Our patient lacked history and the clinical features were suggestive of any of these causes. This patient could not be suffering from Gitelman's syndrome. Gitelman's syndrome is characterized by hypokalemic metabolic alkalosis with significant hypomagnesemia and low urinary calcium excretion.
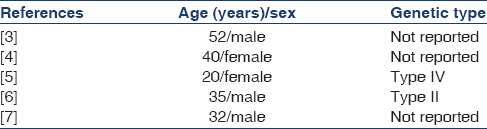
The pathophysiology of Bartter's syndrome is related to defect in the sodium chloride, potassium chloride cotransporter, or potassium channel in thick ascending limb of the loop of Henle. This leads to reduced reabsorption of sodium, potassium and chloride in the thick ascending limb of the loop of Henle. This in turn results in the delivery of these ions to the distal segments where only some sodium is reabsorbed and potassium is secreted. On the genetic basis, the Bartter's syndrome is classified into five types.[1] Types I, II, and IV are a neonatal presentation, while in type III the symptoms begin in the first 2 years of life, but diagnosis is made later, at school-age or adolescence.[2] Gitelman's syndrome is often not diagnosed until adolescence or early adulthood. There were a few reports[34567] of Bartter's syndrome in adults [Table 1]. Though Bartter's syndrome is diagnosed at a young age, an adulthood presentation is possible due to phenotypic variation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- An improved terminology and classification of Bartter-like syndromes. Nat Clin Pract Nephrol. 2008;4:560-7.
- [Google Scholar]
- Bartter's and Gitelman's syndromes: from gene to clinic. Nephron Physiol. 2004;96:p65-78.
- [Google Scholar]
- Bartter's syndrome. Study of a 52 year old man with evidence for a defect in proximal tubular sodium reabsorption and comments on therapy. Am J Med. 1976;61:111-8.
- [Google Scholar]
- Unusual adult-onset manifestation of an attenuated Bartter's syndrome type IV renal phenotype caused by a mutation in BSND. Nephrol Dial Transplant. 2007;22:288-9.
- [Google Scholar]
- Nephrocalcinosis as adult presentation of Bartter syndrome type II. Neth J Med. 2014;72:91-3.
- [Google Scholar]
- Bartter syndrome revealed at adult age by recurrent nephrolithiasis, associated with hypertension and metabolic syndrome. Tunis Med. 2011;89:405-6.
- [Google Scholar]






