Translate this page into:
Brachiocephalic Arteriovenous Fistula for Hemodialysis through the Median Antecubital Vein
Address for correspondence: Dr. E. Elamurugan, Department of Cardiothoracic and Vascular Surgery, Mahatma Gandhi Medical College and Research Institute, Sri Balaji Vidayapeeth University, Puducherry - 607 402, India. E-mail: drmars01@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
In patients unsuitable for radiocephalic fistula creation, the next option is brachiocephalic fistula. In such patients, we exploited the venous interconnections in the cubital fossa for median cubital vein-Brachiocephalic arteriovenous fistula (AVF) creation. In this article, we describe our experience in the creation of such technical variant of the brachiocephalic fistula AVF, its success and associated complications. A retrospective review of such AVF created between September 2014 and August 2015 was done. The data collected included demographics, co-morbidities, basic disease, operative details, patency, complications, and mortality. A total of 68 vascular access surgeries were done which included 26 (38.2%) brachiocephalic AVF using the median antecubital vein. The mean cephalic vein diameter and mean flow rate were 7.18 mm and 1415 ml/min, respectively 2 months after fistula creation. The primary and secondary failure rates were 3.87% and 7.69% respectively. Complications included aneurysm (7.69%), edema (19.23%), hematoma (11.53%), and wound infection (3.8%). Using reverse flow in the median antecubital vein is a safe and simple way to perform brachiocephalic AVF before brachiobasilic AVF and grafts.
Keywords
Arteriovenous fistula
smooth loop arteriovenous fistula
vascular access
Introduction
The KDOQI recommended order of preference for placement of fistulae in patients with chronic kidney disease should be a forearm (radiocephalic) primary fistula, an elbow (brachiocephalic) primary fistula, a transposed brachial-basilic vein fistula, followed by arteriovenous graft (AVG) of synthetic or biological material.[1] In patients with unfavourable anatomy for radiocephalic fistula, if the median antecubital vein or median basilic vein has a favorable anatomy (>2.5 mm and connected to median cephalic vein), it can be used to construct a brachiocephalic arteriovenous fistula (AVF) with reverse flow in that vein which has no valve. Our hypothesis is that this technique even with poor caliber of cephalic vein can increase the flow in the cephalic vein that is sufficient for maturation and cannulation for hemodialysis. Â smooth loop is created from brachial artery to cephalic vein through the antecubital vein and by ligating the distal cephalic vein, perforating vein, and the median vein of forearm. This technical variant has already been described by Pantea and Bengulescu [2] without results data.
Materials and Methods
We did a retrospective analysis of patients who underwent brachiocephalic AVF creation through median antecubital vein in our institute between September 2014 and August 2015. Data collected include each patient's preoperative evaluation, operative procedure, patency, failures, and complications. All patients underwent preoperative ultrasound during their initial clinical evaluation. Several studies support the 2.5-mm vein and 2.0 mm artery diameter threshold for successful creation of a fistula.[1] The patients with following criteria were taken up for brachiocephalic AVF using the median antecubital vein.
-
The anatomy of cephalic vein and radial artery at the wrist is unsuitable for AVF creation
-
Cephalic vein diameter is <2.5 mm
-
Either median antecubital vein/median basilic vein is more than 2.5 mm in diameter and
-
Brachial artery diameter at elbow more than 2 mm.
Primary failure was defined as an AVF that did not mature or thrombosed before the first successful cannulation for hemodialysis treatment. The definition includes (1) inadequate maturation, (2) early thrombosis, (3) failure of the first cannulation, and (4) other complications such as ischemia or infection. Secondary failure was defined as irreversible failure of the AVF after it has been successfully used for hemodialysis.
Operative technique
Under local anesthesia, a transverse skin incision was made at about 1 cm above the elbow crease, centering with the brachial artery pulsation. The median antecubital vein (or median basilic vein) is dissected. The brachial artery is mobilised after dividing the bicipital fascia. A side to side anastamosis between Brachial artery and median basilic vein or median antecubital vein (MAV) was done using 6–0 Prolene. The upper part of the median basilic vein was ligated to change the side to side anastomosis into a side to end anastomosis. Ligation of the perforating vein and venous tributaries from the forearm to the loop created is done to limit the risk of high-flow fistula [Figures 1 and 2]. The fistula was allowed 6 weeks for maturation.

- Operative anatomy of the cubital fossa
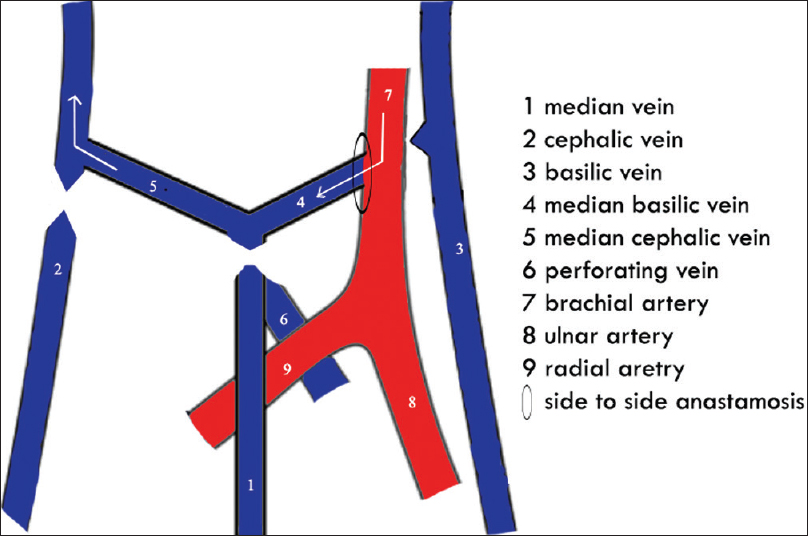
- Brachiocephalic arteriovenous fistula through median antecubital vein at the elbow
A “back wall first” technique is used in all patients, similar to the method described by Tellis et al.[3] This involves initiating the suture in the mid portion of the back wall and using a running suture technique, closing the back wall from the inside of the anastamosis and then completing each corner. The front wall closure is completed with this same continuous running technique. This allows assessment of cephalic vein patency and detects a misplaced suture.
Results
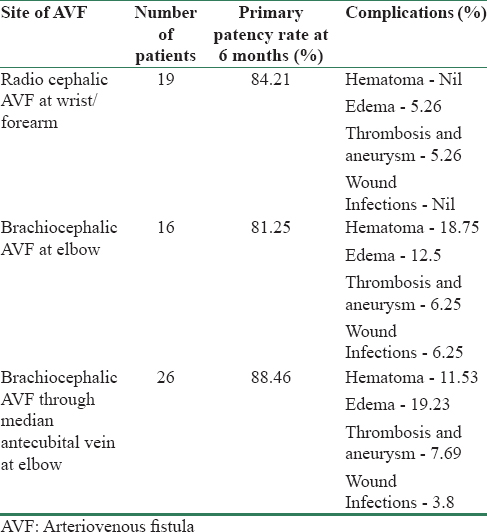
Between September 2014 and August 2015, a total of 68 patients underwent arteriovenous (AV) access surgery. The most common site was brachiocephalic AVF through a median antecubital vein (38.2%) followed by the radiocephalic AVF at the wrist (25%). The other sites were Brachiocephalic AVF at the elbow (23.5%), Radio cephalic AVF at mid forearm (2.9%), proximal radial artery/median vein of forearm AVF (2.9%), and Brachiobasilic AVF with transposition (1.5%). Only three patients (4.5%) underwent AV Graft surgery as they had no choice for native AVF. Lower limb AVF between posterior tibial and saphenous vein was done in one patient (1.5%) due to poor caliber of upper limb veins and unaffordability of the patient for AVG.
The 26 patients with Brachiocephalic AVF through median antecubital vein were included for further analysis. The mean age of patients was 50.78 ± 11.27 years with a range of 30–67 years. Males were 18 (69.2%), and females were 8 (30.8%). The mean follow-up duration was 6 months. The co-morbidities include diabetes mellitus in 8 (30.76%), hypertension in 22 (84.61%), and malignancy in 2 (7.69%) patients.
The mean preoperative diameter of artery and vein were 4.89 mm and 2.85 mm, respectively. The mean cephalic vein diameter before the surgery and 2 months after surgery was 1.95 mm and 7.18 mm respectively. Immediate thrill was present in all the patients. The mean flow across AVF 2 months after creation was 1415 ± 734.01 ml/min ranging from 910 to 2800 ml/min.
Primary Patency rate at 6 months in our series was 88.46% comparable to radiocephalic and brachiocephalic fistula [Table 1]. The primary failure rate of AVF in our series was 3.8% due to thrombosis. The secondary failure rate was 7.69% due to aneurysm formation and thrombosis. Complications include aneurysm and thrombosis (7.69%), edema (19.23%), hematoma (11.53%), and wound infection (3.8%) [Table 1]. During follow-up, 4 (15.38%) patients died with functioning fistula, 6 (23.07%) patients were lost to follow-up, and 13 (50%) patients were continuing dialysis with Brachiocephalic AVF through median antecubital vein. None of the patients died due to complications of AVF surgery.
Discussion
As the life expectancy of hemodialysis patients have improved over years, many patients require multiple vascular access procedures over their lifetime. Furthermore, the long term patency and complications of AVG are worse compared to AVF.[45] Hence, it is prudent to preserve as many vessels possible and start using the distal vessels. In such scenario, the Brachiocephalic AVF through median antecubital vein provides an opportunity to sustain hemodialysis.
In patients with unsuitable cephalic vein at the forearm and elbow, the options are brachiobasilic fistula with transposition and AV grafts either autologous or synthetic. These types of vascular access have few disadvantages, i.e., difficult to construct, the requirement of a second procedure for transposition, costs of graft, and associated infection.[6] However, the presence of multiple interconnected veins with anatomic variations in the cubital fossa allows for AVF creation with other veins such as median basilic vein, MAV and median vein of forearm.
The advantages include avoiding the need for superficialization of the basilic vein in arm. In none of our patients with Brachiocephalic AVF through median antecubital vein, a superficialization of the basilic vein in arm was needed. The main basilic vein is preserved and can be used for future AVF creation. Ligating the tributaries from forearm to the loop created including the perforating vein will prevent the development of high-flow and venous hypertension, and will increase the flow in the cephalic vein.
The demographic profile of our series is similar to other studies with diabetes as the most common cause of end-stage renal disease and the mean age of around 50 years. The most common site of AVF in our study was using brachial artery (63.24%) followed by a radial artery (30.88%). The strategies followed by us were using median basilic vein with caliber (>2.5 mm) adequate enough for anastamosis, larger arteriotomy of 8–10 mm, and side to side anastamosis which allowed for establishing increased blood flow across the anastamosis to aid maturation. Though the mean preoperative caliber of cephalic vein was less than recommended 2.5 mm, using the above strategies resulted in dilatation of venous segment to 7.18 mm and mean flow rate of 1415 ml/min after maturation. KDOQI recommends venous segment diameter of at least 6 mm and flows rate of at least 600 ml/min for successful cannulation.[1] Though we created a larger arteriotomy to enhance flow across fistula, none of our patients developed vascular steal phenomenon.
All our patients underwent side to side anastamosis with proximal vein ligation and ligation of tributaries from forearm to the loop created. The advantages of creation of a side-to-side anastamosis are technical simplicity and uniform wall shear stress profile which would lead to reduced rate of intimal hyperplasia.[7] In a study by O'Banion et al. side to side anastamosis with distal vein ligation has been found to be superior to end to side anastamosis in radiocephalic fistula in terms of early thrombosis, 6-month primary patency and cannulation rates.[8]
Primary failure rate (3.87%) was much lesser compared to rates in the current literature (15–30%) which includes both distal and proximal fistulas.[9] However, the primary failure rates of distal fistulas are higher than proximal fistulas due their small caliber and lower flow rates. Pramila and Biradar reported primary failure rates of 7% and 22.8% in brachial and radial arteries respectively.[10] The primary failure rates were radiocephalic AVF (39%), brachiocephalic AVF (17%), and brachiobasilic AVF (18%) in a study by Gonzalez et al.[11] Our primary failure rate (3.87%) of Brachiocephalic AVF through median antecubital vein is comparable to the above studies.
The complications of AVF surgery in our study was similar to that reported by ChecheriTa et al.[12] Aneurysm resulted in secondary AVF failure in two patients (7.69%).
Conclusion
To conclude, our study supports the use of Brachiocephalic AVF creation through median antecubital vein in patients with favorable veins configurations at the elbow based on adequate blood flow rates, venous segment dilatation, low primary failure rates, and complication rate equivalent to those of other native fistulas. Based on our findings, we prefer native AVF before creating AV grafts by utilizing the cubital fossa venous connections along with its variations.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- NKF-KDOQI. Clinical practice guidelines for vascular access. Am J Kidney Dis. 2006;48(Suppl 1):S248-S272.
- [Google Scholar]
- Internal arteriovenous fistula for hemodialysis. Surg Gynecol Obstet. 1971;132:866-70.
- [Google Scholar]
- Vascular access for hemodialysis: Current perspectives. Int J Nephrol Renovasc Dis. 2014;7:281-94.
- [Google Scholar]
- Vascular access profile in maintenance hemodialysis patients. Iran J Kidney Dis. 2014;8:218-24.
- [Google Scholar]
- Arteriovenous fistulas constructed using side-to-side anastomosis with ligation and division of distal venous arm; a tertiary care hospital experience. J Vasc Access. 2010;11:26-30.
- [Google Scholar]
- Radiocephalic fistulas for hemodialysis: A comparison of techniques. Am Surg. 2015;81:341-4.
- [Google Scholar]
- Hemodialysis angioaccess choice and survival in a tertiary care Saudi Arabian center from 1993 to 2004. Nephrourol Mon. 2011;3:69-73.
- [Google Scholar]
- A study of arteriovenous fistula failure in haemodialysis patients. Sch J Appl Med Sci. 2014;2:336-9.
- [Google Scholar]
- Two-stage brachial-basilic transposition fistula provides superior patency rates for dialysis access in a safety-net population. Surgery. 2010;148:687-93.
- [Google Scholar]
- An overview of permanent vascular access in hemodialyzed patients. Rom J Morphol Embryol. 2015;56:27-31.
- [Google Scholar]







