Translate this page into:
Brachiocephalic artery thrombosis in adult nephrotic syndrome
Address for correspondence: Dr. V. N. Unni, Department of Nephrology, Amrita Institute of Medical Sciences and Research Centre, Kochi - 682 041, India. E-mail: unnivn@aims.amrita.edu
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Thrombotic events are known to occur in nephrotic syndrome, as these patients have a hypercoagulable state. Venous thrombosis is well recognized, but arterial thrombosis is rare and is mainly noted in pediatric population. In the present study, we report a case of thrombosis of right brachiocephalic artery, embolic occlusion of right axillary artery, and right middle cerebral artery territory infarction due to thromboembolism in an adult patient with nephrotic syndrome (Minimal change disease). Patient underwent thromboembolectomy in the right axillary artery followed by anticoagulation therapy.
Keywords
Brachiocephalic artery thrombosis
cerebral infarction
nephrotic syndrome
Introduction
Multiple factors are responsible for the hypercoagulable state and vascular thrombosis in nephrotic syndrome. Alterations in blood levels of various factors involved in coagulation and fibrinolytic systems, endothelial cell dysfunction, alterations in platelet functions, hyperviscosity of blood, hemoconcentration due to diuretics use, and possibly long-term steroid use are contributory factors. Venous thromboembolism is much more frequent than arterial thrombosis. Cerebral infarction due to arterial thromboembolism in adults with nephrotic syndrome has been rarely reported.[12]
Case Report
A 44-year-old man presented to our hospital in 2005 with complaints of generalized edema and frothy urine of two months duration. Evaluation showed nephrotic range proteinuria, hypoalbuminemia, and hypercholesterolemia. Kidney biopsy showed minimal change disease. There was no clinical or laboratory evidence of a secondary cause for nephrotic syndrome. Patient responded to oral prednisolone 1 mg/kg/day and attained complete remission in 4 weeks, when prednisolone was tapered over 8 weeks and stopped; on subsequent follow-up over 4 years, he was an infrequent relapser. He was readmitted in June 2009 with anasarca of three weeks duration and sudden onset of weakness involving left upper and lower limbs, and severe pain with bluish discoloration of right hand for 1 day. He was not a smoker. There was no history of trauma or intake of any medications. Right hand and forearm showed clinical features of ischemia with absence of pulsations in brachial, radial, and ulnar arteries. Central nervous system examination revealed left supranuclear facial palsy and dense left hemiplegia. Evaluation confirmed relapse of nephrotic syndrome: Nephrotic range proteinuria (24 hours urinary protein: 8 gm), hypoalbuminemia (serum albumin: 1.4 gm/dl), and hypercholesterolemia (serum cholesterol: 433 mg/dl). Renal functions (serum creatinine: 0.8 mg/dl) and liver functions were normal. Doppler study showed absence of blood flow in all arteries of right upper limb; carotid arteries did not show any evidence of plaques. Doppler study did not reveal any evidence of thrombosis in renal veins, IVC, or lower limb veins. Chest roentgenogram and ECG were normal. Echocardiography showed normal heart valves and chambers with no evidence of thrombus in the cardiac chambers. Computed tomography (CT) angiogram showed thrombus involving right brachiocephalic trunk [Figures 1a and 1b] with embolic occlusion of right axillary artery and right middle cerebral artery (MCA). CT scan of head showed features of acute right MCA territory infarction [Figure 2]. Patient was worked up for hypercoagulable state: protein C 27% (normal, 70 – 140%), protein S 61% (normal, 60 – 110%), antithrombin III 73% (normal, 75 – 125%), absent factor V Leiden mutation (negative), APTT 32 seconds (control, 32 seconds), PT 13.2 seconds (INR, 1.0), homocysteine 13 micromol/l (normal, 5 – 15 micromol/l). Blood fibrinogen was 736 mg/dl (normal, 200 – 400 mg/dl). Cryoglobulins, anticardiolipin antibodies, and beta-1-glycoprotein antibodies were negative.

- Contrast-enhanced MDCT of neck and thorax, showing partial occlusion of right brachiocephalic trunk (arrow) with thrombus (transverse section)

- Contrast-enhanced MDCT of neck and thorax, showing partial occlusion of right brachiocephalic trunk (arrow) with thrombus (coronal section)
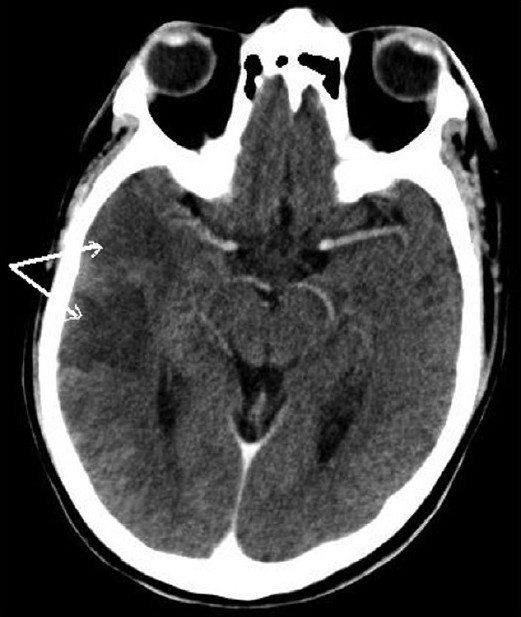
- CT scan head shows right MCA territory infarction (arrows)
He underwent emergency open right axillary artery embolectomy followed by anticoagulation. Initially he was started on heparin, which was followed by oral Warfarin. Subsequently, ischemic changes in the right upper limb improved clinically, power of left upper and lower limbs improved gradually. Patient was continued on oral anticoagulation therapy. Oral prednisolone 1 mg/kg/day was started. After 8 weeks, patient attained remission; steroids were tapered and stopped at the end of 16 weeks. Patient was lost to follow-up; hence, repeat imaging studies could not be done.
Discussion
Addis was the first to draw attention to an increased incidence of venous thrombosis in association with nephrotic syndrome.[3] The risk of vascular thrombosis is greatest within the first six months of diagnosis, with an annual incidence rate of 1.48% for arterial thromboembolism.[4] In nephrotic patients, arterial thrombosis, though rare, has been reported in aorta, mesenteric, axillary, subclavian, brachial, femoral, ophthalmic, carotid, cerebral, renal, pulmonary, and coronary arteries.[124–10]
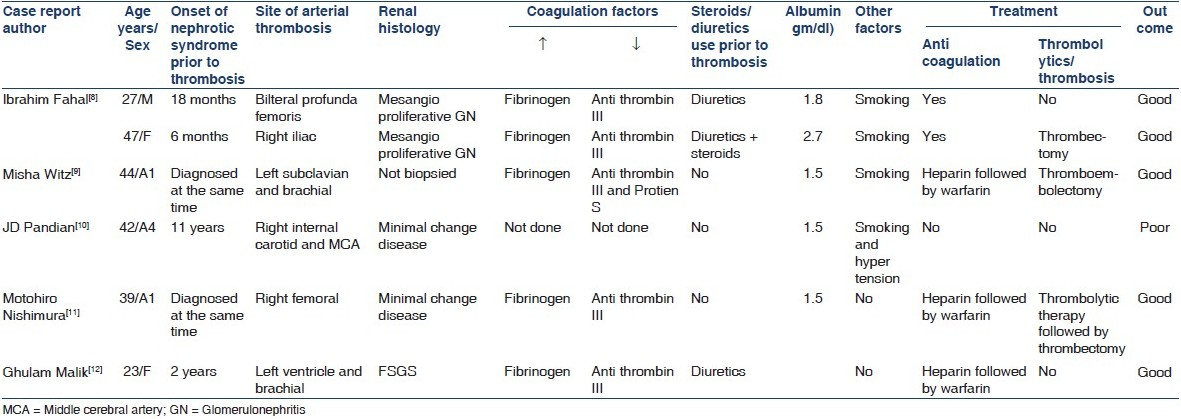
Our patient had brachiocephalic artery thrombosis and thromboembolism of multiple arteries on the right side from that source. Till date, brachiocephalic artery thrombosis with MCA territory infarction in nephrotic syndrome is not reported in literature. Cerebral infarction due to thromboembolism in nephrotic syndrome is an extremely rare but serious complication of nephrotic state.[12] Very few cases of arterial thrombosis in adult nephrotic syndrome have been published in literature [Table 1].
Altered levels of coagulation factors and fibrinolytic system in patients with nephrotic syndrome leads to hypercoagulability.[7] The abnormalities include increased levels of fibrinogen, factor V, Von willebrand factor, factor VII, alpha-1 macroglobulin. This is thought to be due to increased hepatic synthesis of these factors stimulated by hypoalbuminemia[7] and decreased levels of antithrombin III, plasminogen, factor XI, factor XII, alpha one antitrypsin, protein S, and protein C due to urinary losses of these proteins.[7]
Most of the authors noted elevated levels of serum fibrinogen (due to increased hepatic production) and decreased level of antithrombin III (due to renal loss).[891112] Increased blood viscosity due to hemoconcentration contributes to occurrence of thromboembolic complications, which is often aggravated by the use of diuretics.[7] Steroids shorten prothrombin as well as accelerate partial thromboplastin times that aggravate the hypercoagulable state of nephrotic syndrome.[913] The risk of thrombosis is related to the severity and duration of the nephrotic state and appears to be particularly increased with serum albumin concentrations ≤2.0 g/dl.[414]
Arterial thrombosis can be diagnosed with the use of duplex scanning, CT, or magnetic resonance imaging. MDCT angiography has replaced conventional arteriography in almost all centers. Once the diagnosis of vascular thrombosis is established, anticoagulation therapy should be started. Patient can be treated with conventional or low molecular weight heparin, followed by oral Warfarin and antiplatelet agents.[1516] Thromboembolectomy or thrombolytic therapy is indicated in patients with ischemic limbs due to arterial thromboembolism. Attempts to reduce the degree of proteinuria, hyperlipidemia, and hypertension should be made in all nephrotics. Prophylactic anticoagulation may be considered in high-risk patients such as steroid resistant nephrotic syndrome, persistent hypoalbuminemia (serum albumin <2 gm/dl), and membranous nephropathy.[17]
Our patient was treated with combination of embolectomy and anticoagulation therapy. As he had a thrombus involving multiple arteries, he was continued on oral anticoagulation.
To conclude, vascular thrombosis is a rare but a serious complication of nephrotic syndrome. Assessment of various risk factors like duration and severity of hypoalbuminemia may be useful for identifying high-risk patients in whom possibility of vascular thrombosis needs to be expected.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Glomerular Nephritis Diagnosis and Treatment. New York, NY: McMillan Publishers Ltd; 1948.
- High absolute risks and predictors of venous and arterial thromboembolic events in patients with nephrotic syndrome: results from a large retrospective cohort study. Circulation. 2008;117:224-30.
- [Google Scholar]
- Hypercoagulability, renal vein thrombosis, and other thrombotic complications of nephrotic syndrome. Kidney Int. 1985;28:429-39.
- [Google Scholar]
- Status of the coronary arteries in the nephrotic syndrome: Analysis of 20 necropsy patients aged 15 to 35 years to determine if coronary atherosclerosis is accelerated. Am J Med. 1977;63:183-92.
- [Google Scholar]
- Coagulation and thromboembolic complications in the nephrotic syndrome. Adv Nephrol. 1984;13:75-114.
- [Google Scholar]
- Acute subclavian and brachial artery thrombosis as a complication of nephrotic syndrome. Isr Med Assoc J. 2004;6:441-2.
- [Google Scholar]
- Fulminant cerebral infarction in a patient with nephrotic syndrome. Neurol India. 2000;48:180-2.
- [Google Scholar]
- Acute arterial thrombosis with antithrombin III deficiency deficiency in nephrotic syndrome. Surg Today. 2000;30:663-6.
- [Google Scholar]
- Intraventricular and brachial artery thrombosis in nephrotic syndrome. Am J Nephrol. 1998;18:142-5.
- [Google Scholar]
- Vascular complications in nephrotic syndrome: Relationship to steroid therapy and accelerated thromboplastin generation. BMJ. 1970;4:273-6.
- [Google Scholar]
- The clinical spectrum of renal vein thrombosis: acute and chronic. Am J Med. 1980;69:819.
- [Google Scholar]
- Hemostatic complications in renal disorders of the young. Pediatr Nephrol. 1996;10:88-99.
- [Google Scholar]
- Membranous nephropathy and thromboembolism: Is prophylactic anticoagulation warranted? Nephron. 1993;63:249-54.
- [Google Scholar]







