Translate this page into:
Calciphylaxis Induced Isolated Bowel Gangrene in a Septic Deceased Donor Renal Transplant Recipient
Corresponding author: Sarbpreet Singh, Department of Renal Transplant Surgery, Postgraduate Institute of Medical Education and Research, Chandigarh, India. E-mail: drsarbpreet@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Gysley BBJW, Singh S, Bamaniya BB, Sethi J, Patil SKS, Kenwar DB, et al. Calciphylaxis Induced Isolated Bowel Gangrene in a Septic Deceased Donor Renal Transplant Recipient. Indian J Nephrol. doi: 10.25259/IJN_383_2024
Abstract
Calciphylaxis is a rare and life-threatening condition caused by the buildup of calcium in the small blood vessels. It usually affects the deep layers of the skin and tissues in areas such as the abdomen and lower limbs, but can also affect internal organs like the intestines, causing symptoms like gastrointestinal bleeding and bowel tissue death. We encountered a case of calciphylaxis affecting the blood vessels in the intestines of a chronic kidney disease patient who had received a deceased donor kidney transplant. Unfortunately, the diagnosis was delayed, leading to a fatal outcome. This case underscores the importance of considering visceral calciphylaxis in high-risk patients, even when there are no outward signs on the skin.
Keywords
Isolated visceral calciphylaxis
Renal transplant recipient
Mesentery ischemia
Introduction
Calciphylaxis, also known as calcific uremic arteriolopathy (CUA), is a life-threatening complication seen in chronic kidney disease (CKD) patients, particularly those undergoing chronic hemodialysis, renal transplant surgery, experiencing increased parathyroid hormone (PTH) levels, and having imbalanced calcium and phosphate levels as well as other systemic calcification disorders.1 The incidence of calciphylaxis in dialysis patients ranges from 0.04% to 4%. This condition typically presents with cutaneous or subcutaneous lesions in the initial stages and may progress to visceral calciphylaxis.2 Calciphylaxis carries a high risk of mortality, with one-year mortality rates ranging from 45% to 80%.3
We report a case of isolated mesenteric calciphylaxis in a CKD patient on chronic hemodialysis who underwent a septic deceased donor renal transplantation and recently presented with bowel gangrene and peritonitis.
Case Report
A middle-aged man, was a case of end-stage kidney disease on maintenance hemodialysis for seven years with secondary hyperparathyroidism. He underwent a deceased donor renal allograft transplant from a 29-year-old donor with no comorbidities. The donor was found to be in sepsis with elevated procalcitonin, and blood culture yielded Acinetobacter baumannii sensitive to meropenem and Candida auris. So, transplantation was done under meropenam and caspofungin cover. Preoperatively, anti-thymocyte globulin induction was given followed by tacrolimus, mycophenolate mofetil (MMF), and prednisolone. He made an uneventful recovery and was discharged home.
He presented with intermittent colicky pain in the left iliac fossa with one episode of melena at the end of 1 month. The abdominal examination showed diffuse tenderness to light palpation without guarding or rebound tenderness. Abdominal imaging was normal, with normal vascular opacification and no findings of visceral calcification. He had a persistently elevated leukocytosis (>16 k cells/mL), raising procalcitonin (12–32 mcg/l), CRP (165–290 mg/l), and lactate levels (6–10 mmol/L). Other lab parameters showed hemoglobin (7.8 gm), serum creatinine (0.8 mg/dL), intact PTH (766 pg/mL), serum calcium (10.6 mg/mL), serum phosphate (6.3 mg/mL), and albumin (2.6 mg/dL). Microbiological analysis showed no growth in blood and urine samples. The patient developed rigidity and the clinical condition deteriorated. The immunosuppression was stopped and just maintained on IV hydrocortisone. He was also empirically started on meropenam and liposomal amphotericin B. A diagnostic laparoscopy, which revealed multiple gangrenous patches in the small bowel loop and caecum with minimal pus flakes [Figure 1]. Ileocecal resection and segmental resection of the small bowel were done with stoma creation. Intraoperatively, mesenteric vessels were normal.
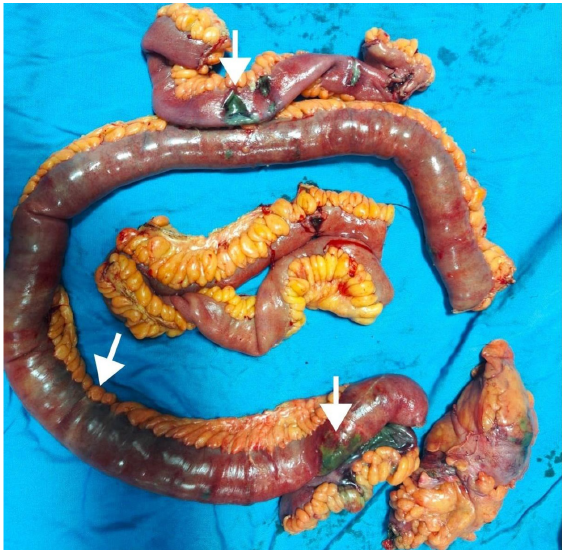
- Resected small bowel segment showing gangrenous patches (marked by arrow heads) with intervening normal segments.
The resected bowel segment exhibited transmural inflammation with thrombosis of capillaries and arterioles. The intestinal mucosa showed ischemic necrosis. There was also increased basophilic staining in the bowel wall, which on Von Kossa stain confirmed the metastatic calcium deposition that gave the diagnosis of visceral calciphylaxis and which led to vascular thrombosis and bowel gangrene [Figure 2]. Subsequently, the patient developed sepsis-induced disseminated intravascular coagulation and died.
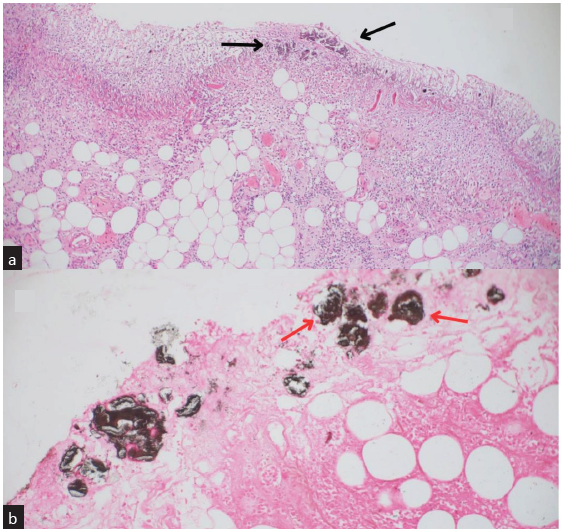
- (a) Shows complete loss of intestinal mucosa with ischemic necrosis. It also shows basophilic masses of calcification (bold black arrows) in the muscular mucosae and the lamina propria suspicious of calcium deposition (Stain—Eosin and hematoxylin at 200× magnification). (b) Von Kossa stain highlights the calcium deposits in the vessels by taking up the black color (bold red arrows). It also shows thrombosis within the serosal vessels, confirming the metastatic calcification leading to mucosal ischemia (400× magnification).
Discussion
The existing literature on calciphylaxis focuses on only cutaneous manifstations or visceral calciphylaxis after a cutaneous manifestation4 or the coexistence of cutaneous and visceral calciphylaxis. Cases have been reported among posttransplant patients with functional renal graft.5 Ours is the first documented case to be reported that primarily presented with visceral calciphylaxis, specifically involving mesenteric vessels with no cutaneous manifestations after transplantation. The patient presented with features of bowel ischemia (abdominal pain), followed by gastrointestinal (GI) bleeding (melena), and finally perforation peritonitis. In our case, we lacked a probing skin manifestation, so visceral calciphylaxis was never considered among our differentials during the initial evaluation. None of the imaging showed any evidence of calcifications in visceral or cutaneous sites. Abdomen exploration gave the first suspicion of mesenteric vasculature involvement due to the pattern of patchy gangrene. Microscopy of the resected bowel became diagnostic and showed a new spectrum of symptomatology in patients with calciphylaxis.
Conclusion
In cases of CKD, it’s important to consider the possibility of atypical calciphylaxis when patients experience GI symptoms and have risk factors for this condition. This is also relevant for posttransplant patients who had prolonged hemodialysis before their transplant. High index of suspicion is necessary with appropriate investigations as indicated.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
References
- A nationally representative study of calcific uremic arteriolopathy risk factors. J Am Soc Nephrol. 2016;27:3421-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Early clinical presentations and progression of calciphylaxis. Int J Dermatol. 2017;56:856-61.
- [CrossRef] [PubMed] [Google Scholar]
- Calciphylaxis: Natural history, risk factor analysis, and outcome. J Am Acad Dermatol. 2007;56:569-79.
- [CrossRef] [PubMed] [Google Scholar]
- Isolated mesenteric calciphylaxis with ischemic colitis in a hemodialysis patient without active cutaneous calciphylaxis: A case report of calcific uremic arteriolopathy. Kidney Med. 2020;2:209-12.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Gastric calciphylaxis in a patient with a functioning renal allograft. Clin Nephrol. 2007;67:119-25.
- [CrossRef] [PubMed] [Google Scholar]








