Translate this page into:
Cerebral venous sinus thrombosis in children with nephrotic syndrome
Address for correspondence: Dr. Dinesh Nirmaldas Gera, Professor, Professor, Department of Nephrology and Clinical Transplantation, Institute of Kidney Diseases and Research Centre, Dr. Hargovind L. Trivedi Institute of Transplantation Sciences [IKDRC-ITS], Civil Hospital Campus, Asarwa, Ahmedabad - 380 016, Gujarat, India. E-mail: dinesh.gera@ikdrc its.net
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Nephrotic syndrome in infancy and childhood can be associated with thromboembolic complications. We describe two cases of nephrotic syndrome who presented with non-specific findings. Magnetic resonance imaging brain with magnetic resonance venography showed thrombosis of multiple venous sinuses. Patients were successfully treated with anticoagulants and there was complete resolution of thrombosis on repeat imaging.
Keywords
Anticoagulation
cerebral venous sinus thrombosis
magnetic resonance imaging
magnetic resonance venography
nephrotic syndrome
Introduction
Thromboembolism in patients with nephrotic syndrome is a well-known complication because of hypercoagulable state and many other factors like hemoconcentration, increased blood viscosity, hypoalbuminemia, alteration in platelet function, and possibly administration of steroids and/or diuretics.[1] The thromboembolic complication of peripheral and deep veins is more common in adults as compared to children though lower incidence in children, it tended to be more severe in children.[2] Cerebral venous sinus thrombosis (CVST) in children is a rare complication and only few cases have been reported.[3–7] Following two cases demonstrate this rare complication. Sinovenous thrombosis is probably less recognized and the symptoms and clinical course are highly variable. As in the present reported cases, symptoms may be very non-specific like headache, vomiting, drowsiness and altered behavior. The CVST should be suspected in any patient with nephrotic syndrome who develops any neurologic symptoms like headache, vomiting and cranial nerve palsy, altered sensorium or seizures. Easy availability of imaging techniques like magnetic resonance imaging (MRI) and magnetic resonance venography (MRV) along with increasing awareness of condition should make it more frequently diagnosed, with scope of its reversal with timely treatment.
Case Reports
Case 1
A 4-year-old boy, weighing 14 kg with steroid-responsive nephrotic syndrome of 1-year duration developed vomiting and drowsiness for 2 days, with fresh re-appearance of edema (relapse of nephrotic state). He had vomiting, 5-6 times a day, after each feeding attempt. He was on tapered treatment with prednisolone 5 mg per day, but developed fresh relapse. On admission, dose of prednisolone was increased to 20 mg daily. Past medical history was negative for migraine headaches, head trauma, febrile illness, substance abuse, vitamin intake or thrombophlebitis. Family history was unremarkable.
On admission, his vital signs were normal with pulse rate of 80/min, regular, and blood pressure of 110/80 mmHg. General examination revealed periorbital edema with mild ascitis. He was drowsy, apathetic, resenting disturbance and liking to be lying undisturbed. Neurologic examination revealed uncooperative child, conscious but resenting interference with normal cranial nerve examination and good tone and power in all four limbs with normal sensation and normal deep tendon reflexes. There was no neck rigidity, fundus examination revealed blurring of disc margin with early papilledema. The rest of systemic examination was normal.
Investigations showed hemoglobin 11.1 gm/dl with packed cell volume of 36%, total leucocytes count of 12,600/mm3, platelet count 2.8 lac/mm3, serum creatinine of 0.42 mg/dl, blood urea of 18 mg/dl and serum albumin of 2.1. Serum electrolytes were normal. Coagulation profile showed prothrombin time of 11 s with international normalized ratio (INR) of 1.12 and activated partial thromboplastin time of 28 s. Protein C and protein S levels were normal. Urine analysis showed 2+ proteinuria, 24 h urine protein excretion was 2.0 gm/day. Serum C3 and C4 complements levels were normal. Renal ultrasonography revealed normal sized kidney without dilatation of pelvicalyceal system.
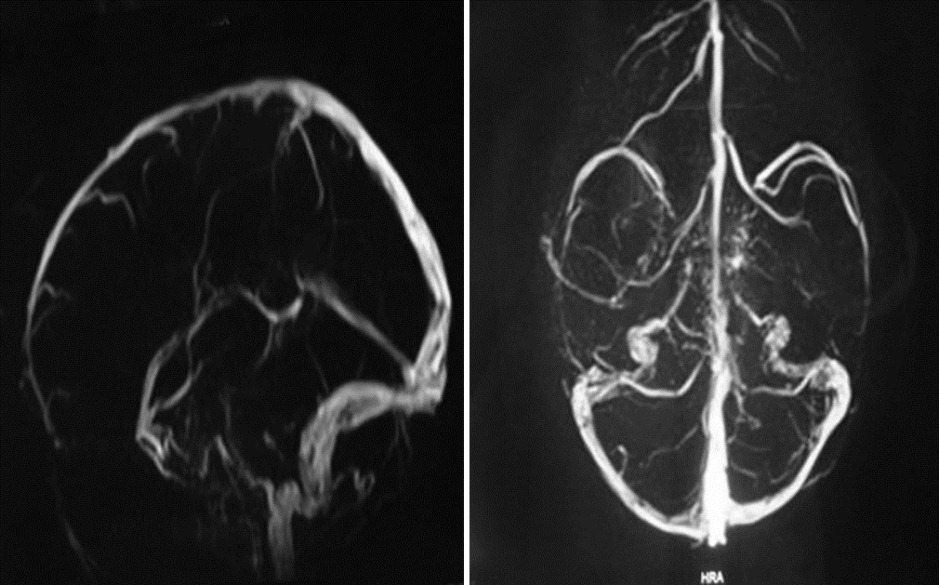
Computer tomography scan brain without contrast was normal, so MRI brain and MR venography was done which demonstrated thrombosis of superior sagittal, left transverse and left sigmoid sinuses. There were no cerebral parenchymal or brainstem lesions [Figure 1].

- Magnetic resonance imaging brain (left) and magnetic resonance venography (right) showing thrombosis of superior sagittal sinus, left transverse and left sigmoid sinuses
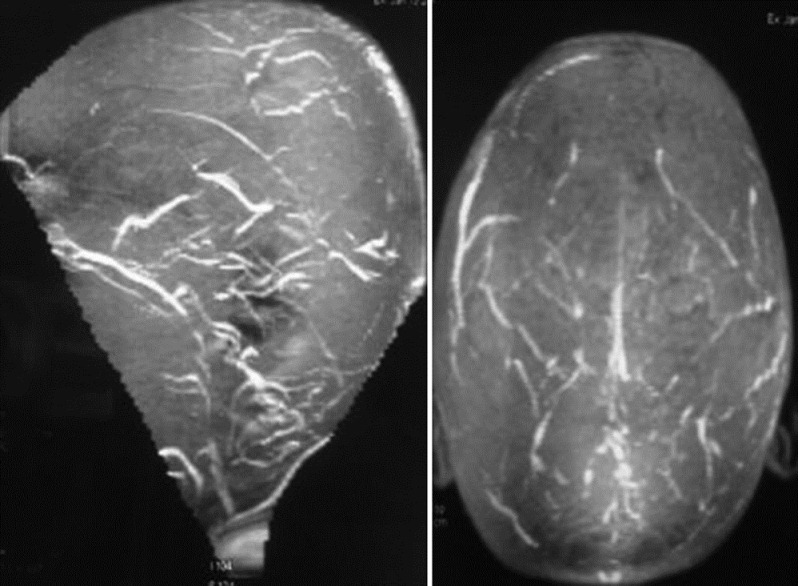
He was treated with daltaparin, a low molecular weight heparin 1000 U (75-100 U/kg each dose 12 h) subcutaneous twice daily for 5 days, and oral anticoagulant warfarin was added on fourth day in dose of 0.75 mg twice a day. Dose of warfarin was adjusted to keep INR between 2.0 to 2.5 (in dose range of 0.05-0.1 mg/kg). The nephrotic state was treated with 50 ml of 20% human albumin i/v daily for four days with prednisolone 20 mg/day and patient had increased dieresis on 4th day of admission and child had nil proteinuria after 10 days. The child responded well to treatment, his drowsiness and vomiting improved in 2 days, and he recovered completely in 2 weeks. Repeat MRI brain with MRV performed after 2 months showed complete resolution of thrombus from all the cerebral venous sinuses. His warfarin dose was reduced after resolution, and was continued in lower dose 0.5 mg twice a day for further 6 months, though INR was difficult to keep at two. At present, patient is off anticoagulant treatment without any neurological complaints [Figure 2].
- Repeat magnetic resonance imaging brain with magnetic resonance venography performed after 2 months showed complete resolution of thrombus from all the cerebral venous sinuses
Case 2
A 3 and a 1/2-year-old boy weighing 12.5 kg with new onset nephrotic syndrome of 15 days duration presented with continuous frontal headache for 3 days at the time of admission. Headache was not associated with fever, vomiting, and blurring of vision. He was taking prednisolone 15 mg/d for nephrotic syndrome. Past medical history and family history was unremarkable. On admission, patient was conscious, cooperative, and well oriented. His pulse rate was 86/min and blood pressure was 100/60 mmHg. On general examination, child showed moderate ascitis and peripheral edema. Rest of systemic examination was normal.
Investigations showed hemoglobin 11.6 gm/dl, total leucocyte count of 11800/mm3, platelet 2.3 lac/mm3, serum creatinine of 0.50 mg/dl, blood urea of 22 mg/dl, and serum albumin of 1.7 gm/dl, S. Serum cholesterol was 537 mg/dl. Serum electrolytes were normal. Renal ultrasound revealed normal sized kidney. Coagulation profile showed prothrombin time of 10 s with INR of 1.1, and activated partial thromboplastin time of 29 s Cranial MRI and MRV showed thrombosis of superior sagittal, bilateral transverse and bilateral sigmoid sinuses [Figure 3].
- Magnetic resonance imaging and magnetic resonance venography showed thrombosis of superior sagittal, bilateral transverse, and bilateral sigmoid sinuses
His steroid dose was continued at 15 mg per day and daily intravenous human albumin (20%) 50 ml was given for 5 days till his serum albumin rose to 3 gm/dl. He was started on deltaparin (LMWH) 1000 U (75-100 U/kg each dose 12 h) subcutaneous twice daily for 5 days and warfarin was added on the fourth day with a dose of 0.75 mg (in dose range of 0.05-0.1 mg/kg) twice a day. Sixth day onwards, patient was maintained on warfarin only to keep INR between 2.0 and 2.5. There was complete resolution of headache within 5 days of starting the treatment. His MRI with MRV done 3 weeks later showed significant dissolution of thrombosis in all affected sinuses. Presently, the boy is on warfarin 1.5 mg for venous thrombosis, prednisolone 15 mg/day, and mycophenolate mofetyl 125 mg twice a day with his nephrotic state in remission. MRV after 3 weeks of treatment is shown in Figure 4.
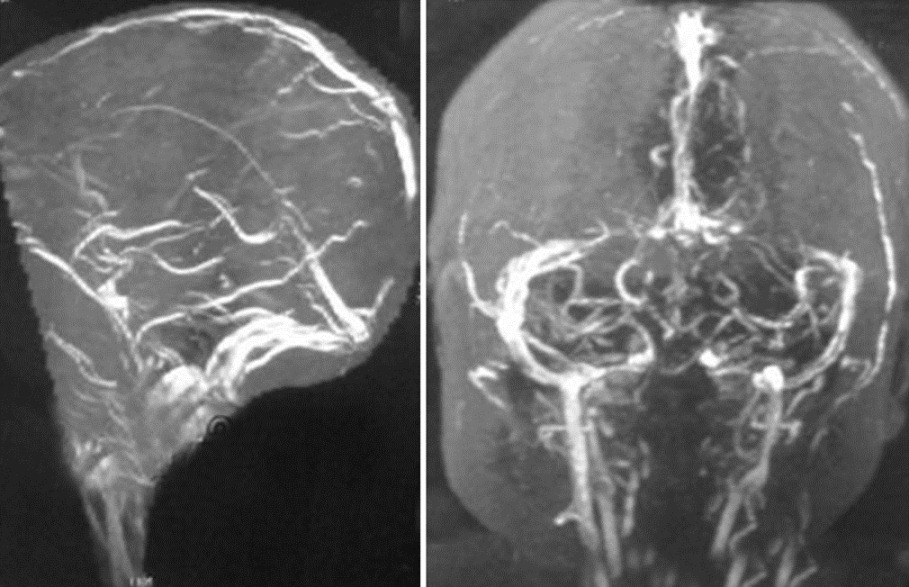
- Magnetic resonance venography brain showing partial dissolution of thrombosis in cerebral venous sinuses
Discussion
Cerebral sinovenous thrombosis is a rare disorder in children, but increasingly diagnosed now because of greater clinical awareness, sensitive neuroimaging techniques. In follow-up of 700 children with nephrotic syndrome over a period of 17 years, Divekar et al. reported only one case of CVST.[8] It is surprising that case 2 in the present study had persistant headache at the time of initial presentation of nephrotic syndrome of 15 days duration.
CVST in nephrotic syndrome is associated with a hypercoagulable state arising due to alteration in blood levels of various factors involved in coagulation, fibrinolytic system, alteration in platelet function, hemoconcentration, increased blood viscosity, and possibly administration of steroids and diuretics.[1] Loss of antithrombin III (physiological anticoagulants) and plasminogen in urine and their low level in blood has been correlated with low serum albumin level.[910] Increased production of fibrinogen adds to increased viscosity and hypercoagulability.[1112]
MRI with magnetic resonance venography is the preferred modality over CT scan for diagnosis and follow-up of cerebral venous thrombosis because of its high sensitivity.[413]
In addition to treating relapse of nephrotic state, correction of hypoalbuminemia by intravenous fresh frozen plasma to replace deficient physiologic anticoagulant factors and or i/v human albumin in small aliquots daily till serum albumin is reasonably normalized.[3] The most commonly used treatment is unfractionated heparin or low-molecular-weight heparin to arrest the thrombotic process for initial few days to a week with overlap of oral anticoagulants in the last 2 days of parentral heparin.[3–7] The optimal duration of oral anticoagulant (warfarin) treatment after the acute phase is unknown in this particular situation, but in the absence of recurrent thrombosis, according to the guidelines of seventh ACCP conference on antithrombotic therapy in children, anticoagulant therapy is to be continued at least for 6 months, using vitamin K antagonists (warfarin) with targeted INR range 2.0-3.0[14] Fibrinolytic agents have not been fully investigated in nephrotic children.
Conclusions
The signs and symptoms of cerebral venous thrombosis are occasionally non-specific making clinical diagnosis difficult. Hence, a high degree of suspicion is required, and a diagnosis of CVST should be considered in any child of nephrotic syndrome presenting with features of central nervous system involvement. MRI and MR venography is a better way of imaging as compared to CT scan. Prompt treatment with anticoagulation is very useful and should be instituted as early as possible to improve the outcome. Not allowing serum albumin to fall below 2 gm/dl could be a preventive measure to such complications.
Source of Support: Nil
Conflict of Interest: None declared
References
- Hemostasis and thromboembolism in children with nephrotic syndrome: Differences from adults. J Pediatr. 1987;110:862-7.
- [Google Scholar]
- Cerebral venous thrombosis in the nephrotic syndrome. Saudi J Kidney Dis Transpl. 2000;11:59-63.
- [Google Scholar]
- Vomiting, headache and seizures in a child with idiopathic nephrotic syndrome. Nephrol Dial Transplant. 1997;12:1280-1.
- [Google Scholar]
- Cerebral venous sinus thrombosis in minimal change nephrotic syndrome. Nephrol Dial Transplant. 1995;10:30-4.
- [Google Scholar]
- Superior sagittal sinus thrombosis in a child with nephrotic syndrome. Pediatr Nephrol. 1996;10:206-7.
- [Google Scholar]
- Plasminogen and antithrombin III deficiencies in the childhood nephrotic syndrome associated with plasminogenuria and antithrombinuria. J Pediatr. 1980;96:390-2.
- [Google Scholar]
- Fibrinogen metabolism and distribution in patients with the nephrotic syndrome. J Lab Clin Med. 1967;70:678-85.
- [Google Scholar]
- Blood viscosity and haemostasis in the nephrotic syndrome. Thromb Haemost. 1983;49:155-7.
- [Google Scholar]
- Children with cerebral venous thrombosis diagnosed with magnetic resonance imaging and magnetic resonance angiography. Neurosurgery. 1992;31:870-6.
- [Google Scholar]
- Antithrombotic therapy in children: The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126:645S-687.
- [Google Scholar]







