Translate this page into:
Challenges in Management of Disseminated Melioidosis with Endocarditis in a Patient with Chronic Kidney Disease
Address for correspondence: Dr. Edwin Fernando, Plot No. 1623, 9th Main Road, Ramnagar South, Madipakkam, Chennai - 600 091, Tamil Nadu, India. E-mail: nephroeddy@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Melioidosis is a tropical infection that is increasingly being reported from South India. It is frequently observed in patients with diabetes mellitus, chronic ethanol consumption and chronic kidney disease (CKD). It presents commonly with pneumonia, deep seated abscesses or osteoarticular infections. Cardiac complications are very rare with endocarditis being reported in very few patients. We report the first case of endocarditis in melioidosis in India. Although infections are common in patients with CKD, melioidosis at the time of diagnosis of CKD has never been reported in the past. Our patient had multiple liver abscesses and endocarditis, and responded well to a 6 week course of ceftazidime and doxycycline, with the latter being continued for 20 weeks.
Keywords
Melioidosis
chronic kidney disease
liver abscess
endocarditis
Introduction
Melioidosis is an emerging infectious disease of major public health importance, which has been increasingly reported from South India over the last decade. It has been frequently observed in patients with diabetes, alcoholism and renal failure. Its presentation varies from an acute fulminant septicemia to a chronic granuomatous disease.[1] We describe a case of disseminated melioidosis in a young girl, who presented with multiple liver abscesses at the time of diagnosis of Chronic Kidney Disease (CKD) stage 5. The infection was complicated by endocarditis that further protracted the course of the patient.
Case Description
A 16 year old girl, who was premorbidly asymptomatic, presented to our emergency department with high-grade intermittent fever, loose stools and abdominal pain for 4 weeks duration. Examination was significant for pallor, pedal edema and right hypochondrial tenderness. Initial investigations were significant for severe renal failure [creatinine = 13.3 mg/dL, urea = 178 mg/dL], severe anemia [hemoglobin = 6.3 g/dL] and neutrophilic leucocytosis [total counts = 13,600 with 80% polymorphs] [Table 1]. Imaging (with computed tomography (CT) and ultrasound) revealed bilateral contracted kidneys (7.5 and 6 cm – right and left respectively) and urinalysis was normal. She was thus diagnosed with CKD-stage 5, probably due to chronic interstitial nephritis and was initiated on hemodialysis for the same.
| Investigation | Result |
|---|---|
| Hemoglobin | 6.3g% |
| Packed cell volume | 19.8% |
| RBC count | 2.22 million/mm3 |
| Total leucocyte count | 13600 cells/mm3 |
| Differential count | 80% polymorphs, 18% lymphocytes, 2% eosinophils |
| Platelet count | 1.92 lakhs/mm3 |
| ESR (60 min) | 95 mm |
| Creatinine | 13.3 mg/dL |
| Urea | 178mg/dL |
| Sodium | 132 meq/L |
| Potassium | 4.6 meq/L |
| Chloride | 101 meq/L |
| Bicarbonate | 14 meq/L |
| Random blood glucose | 84mg/dL |
| Total bilirubin | 0.2mg/dL |
| Total protein | 5.8g/dL |
| Albumin | 3.2g/dL |
| Globulin | 2.6g/dL |
| SGOT (ALT) | 82 U/L |
| SGPT (AST) | 16 U/L |
| Alkaline phosphatase | 116 U/L |
| Blood-borne viral screen (HIV, HbsAg, HCV) | Negative |
RBC: Red blood cell; ESR: Erythrocyte sedimentation rate; SGOT: Serum glutamic-oxaloacetic transaminase; ALT: Alanine aminotransferase; AST: Aspartate transaminase; HCV: Hepatitis C virus
Imaging also detected the presence of multiple liver abscesses (measuring 63 × 35 mm in the superior aspect of the right lobe, 43 × 40 mm in the inferior aspect of the right lobe, and 80 × 55 mm in the left lobe) [Figure 1]. Given the history of loose stools and the background of recently diagnosed CKD (which made her an immunocompromised host), the possibility of pyogenic liver abscess was considered, with the gram-negative enteric organisms being implicated. She was hence initiated on parenteral broad-spectrum antibiotics (piperacillin + tazobactam and metronidazole) after blood cultures. Possible sources of portal pyemia were looked for with the help of colonoscopy and contrast CT imaging. Source control in the form of drainage of liver abscesses was also done, but the fever persisted. Although the blood cultures were negative, pus aspirated from the liver abscess grew Burkholderia pseudomallei. They were identified by the presence of wrinkled medium-sized colonies with metallic sheen on Mac Conkey agar [Figure 2]. She was diagnosed with melioidosis and switched over to ceftazidime (1g IV 8th hourly) and oral cotrimoxazole (double strength, twice a day).

- Plain CT imaging of the abdomen showing centrally hypoattenuating lesion in the right lobe measuring 63 × 35 mm
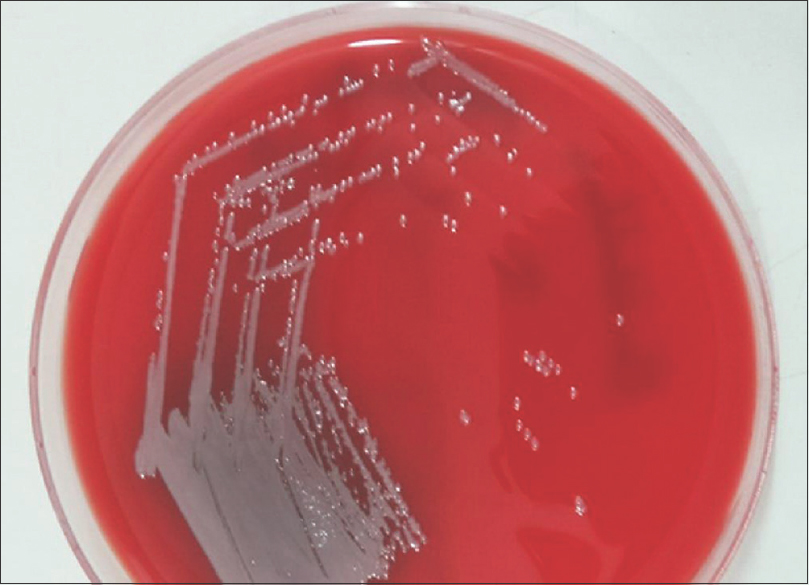
- Pus aspirated from the liver abscess cultured on Mac Conkey agar. Growth of Burkholderia pseudomalleii evident by the colonies with “metallic sheen”
However, fever persisted and multiple blood cultures done subsequently were also found to be sterile. Repeat imaging of the chest and abdomen did not reveal any new focus of infection. However, echocardiogram detected the presence of vegetations on the mitral valve [Figure 3] and the diagnosis was revised into disseminated melioidosis with endocarditis. Therefore, it was decided to increase the dose of ceftazidime (to 2g IV 8th hourly) and extend the intensive phase of treatment to 6 weeks. Her fever settled over the subsequent 4 days and she continued to remain afebrile throughout the course of hospitalization.
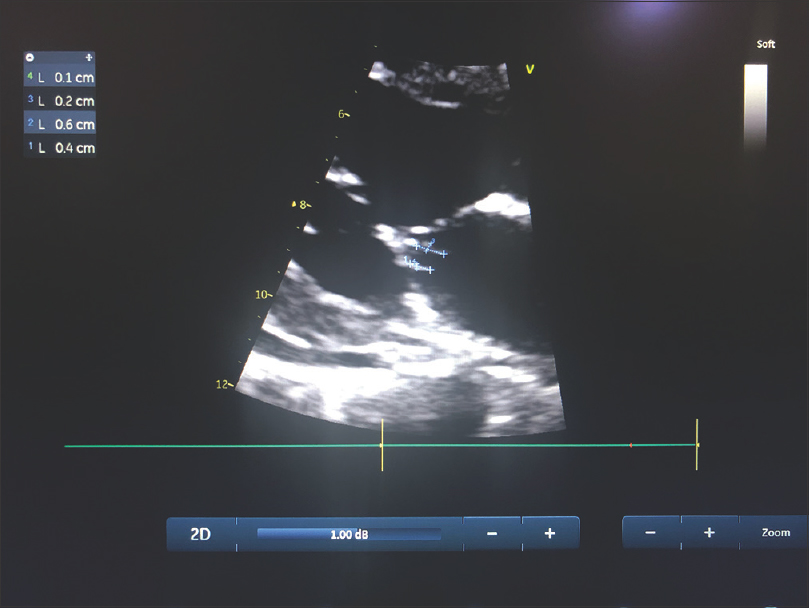
- Transthoracic echocardiogram showing two vegetations attached to the atrial aspect of the posterior mitral leaflet measuring 4 × 1 mm and 6 × 2 mm
One week after initiation of treatment, her potassium levels started rising despite alternate day hemodialysis and a potassium-free diet. Cotrimoxazole was thought to be the culprit drug and it was switched to oral doxycycline (100mg twice daily). Subsequently, her potassium levels stabilized and eradication phase with doxycycline was planned for a total of 20 weeks.
The patient was followed up subsequently after 3 months and was found to have significant clinical improvement with near-total resolution of systemic symptoms. Repeat imaging revealed clearance of the vegetation and significant decrease in size of the liver abscesses. She has been advised to continue eradication therapy with doxycycline. She continues to be on thrice weekly schedule of hemodialysis.
Discussion
Melioidosis is an infection that is endemic to South East Asia and Northern Australia.[2] There has been an increase in reports of Meloidosis from South India in the past decade, probably owing to increase in awareness that translates into higher index of clinical suspicion and improved diagnostic methods.[13]
Melioidosis is caused by the Gram-negative bacterium, Burkholderia pseudomalleii. It is a saprophytic organism that favours moist clay soils. Inhalation (rather than inoculation or ingestion) of aerosolized dust has been implicated in acquisition of infection in most cases. Our patient belonged to an agricultural family from rural south India (Karaikudi). Most cases reported had an occupational history of exposure to soil.[2]
Although melioidosis is more common among males, there has been a study that noted female preponderance among the patients with end stage renal disease.[4] Poorly controlled diabetes mellitus, chronic ethanol consumption and CKD have been frequently reported as risk factors. Other comorbidities reported include thalassemia, sickle cell anemia, liver disease, steroid use, chronic obstructive pulmonary disease and tuberculosis. The effect of these risk factors on neutrophil function has been implicated in the pathogenesis of melioidosis.[5]
The manifestations of the disease are protean. The disease has been usually observed in two forms: localized melioidosis (where the involvement is confined to a single organ like septic arthritis or deep-seated visceral abscess) and disseminated melioidosis (with multi-system involvement).[5] Pulmonary involvement is common in the acute presentation and often the patients tend to present with septicemia, whereas the chronic forms may be either localized in the form of visceral abscesses (splenic, hepatic, prostatic) or osteoarticular infections (septic arthritis or osteomyelitis), or may be disseminated with multifocal involvement.[1] In patients with CKD 5 requiring dialysis, the presentation was frequently acute and the presence of bacteremia was more common.[4]
Isolation of the bacterium from pus, body fluids or blood is the gold standard in diagnosis of melioidosis.[6] The organism shows bipolar staining on Gram stain and has a typical “safety pin” appearance. Growth on blood agar and Mac Conkey agar reveal smooth wrinkled colonies with a metallic sheen. Selective media like Ashdown agar medium have a better yeild.[7]
The management of melioidosis is divided into 2 phases: the initial shorter intensive phase (which lasts for 2 weeks) and the subsequent longer eradication phase (which lasts for 20 weeks). Ceftazidime, carbapenems (imipenem and meropenem) and to a lesser extent amoxicillin clavulanate are the preferred options for the initial phase of treatment.[2] Ceftazidime is the only drug with mortality benefit in melioidosis and doses upto 2g 6th hourly can be given.[8] Cotrimoxazole and Doxycycline (either or both) constitute the eradication therapy for most patients, although the former seems to have a higher efficacy with lower relapse rates.[9] As the organism is intrinsically resistant to a wide range of antibiotics (third-generation cephalosporins, penicillins, rifamycins, aminoglycosides, and to a lesser extent quinolones and macrolides), choice of initial antibiotic is vital in patients with suspected melioidosis.
Relapse has been reported in 13%-23% of patients, 6-8 months after successful treatment completion.[2] Risk factors for relapse appear to be poor compliance, multifocal involvement, initial presentation with a severe disease and shorter eradication period.[9]
Cardiac involvement is uncommon in melioidosis with pericardial effusion being more frequently encountered. There are very few case reports on endocarditis in melioidosis across the globe.[101112] Almost all the patients reported are males and had risk factors in the form of chronic ethanol consumption or chronic obstructive pulmonary disease. Two such patients had further complications in the form of cerebral infarcts.[1012] This is the first case report of endocarditis in melioidosis in India, to the best of our knowledge.
There are no existing guidelines on the treatment of melioid endocarditis, with most of the knowledge regarding the same, originating from case reports and case series. As our organism was resistant to aminoglycoside, we did not consider adding it to the existing regime, which had been earlier attempted with aminoglycoside susceptible strains.[11] A 6 week course of high-dose ceftazidime or carbapenem along with cotrimoxazole or doxycycline seem to constitute the intensive phase of treatment in these patients.
Conclusion
Melioidosis as the first presentation of CKD has not been reported in the past and our case is unique in this aspect. It is a disease with high case fatality rate and hence a high degree of clinical suspicion is required for early diagnosis. Ceftazidime or carbapenem may be a good choice for initial antibiotic in patients suspected with melioidosis. Endocarditis requires prolongation of the intensive phase of treatment to 6 weeks. Good compliance and completion of the eradication phase needs to be ensured to prevent relapse.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors would like to acknowledge their radiologist, Dr. Anand for his significant contribution towards the patient.
References
- Clinical manifestations, antimicrobial drug susceptibility patterns, and outcomes in melioidosis cases, India. Emerg Infect Dis. 2019;25:316-20.
- [Google Scholar]
- Melioidosis: Epidemiology, pathophysiology, and management. Clin Microbiol Rev. 2005;18:383-416.
- [Google Scholar]
- ' Melioidosis in southern India: Epidemiological and clinical profile. Southeast Asian J Trop Med Public Health. 2010;41:401-9.
- [Google Scholar]
- Melioidosis and end-stage renal disease in tropical northern Australia. Kidney Int. 2014;86:867-70.
- [Google Scholar]
- Melioidosis: An emerging Infection in India. J Assoc Physicians India. 2013;61:612-4.
- [Google Scholar]
- Melioidosis in South Asia (India, Nepal, Pakistan, Bhutan and Afghanistan) Trop Med Infect Dis. 2018;3:pii: E51.
- [Google Scholar]
- Clinical features and laboratory diagnosis of infection with the potential bioterrorism agents burkholderia mallei and burkholderia pseudomallei. Int J Biomed Sci. 2007;3:144-52.
- [Google Scholar]
- Halving of mortality of severe melioidosis by ceftazidime. Lancet Lond Engl. 1989;2:697-701.
- [Google Scholar]
- Risk factors for recurrent melioidosis in northeast Thailand. Clin Infect Dis Off Publ Infect Dis Soc Am. 2006;43:979-86.
- [Google Scholar]
- Melioidosis: An unusual cause of infective endocarditis: A case report. Eur Heart J-Case Rep. 2018;2:yty055.
- [Google Scholar]
- Melioidosis with endocarditis and massive cerebral infarct. Ital J Med. 2015;10:55.
- [Google Scholar]







