Translate this page into:
Collagenofibrotic Glomerulopathy—An Unexpected Finding in a Young Female
Corresponding author: Naga Sarika Vennavalli, Department of Histopathology, Yashoda Hospitals, Hyderabad, Telangana, India. E-mail: sarivennavalli@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vennavalli NS, Annavarajula SK, Khubchandani SR, Wasnik DV. Collagenofibrotic Glomerulopathy—An Unexpected Finding in a Young Female. Indian J Nephrol. 2024;34:544-5. doi: 10.25259/IJN_164_2024
Dear Editor,
Collagenofibrotic glomerulopathy (CG) is a rare kidney disease, seldom suspected clinically. A 31-year-old lady was referred for the evaluation of hypertension and proteinuria, which she had developed in the third trimester of her second pregnancy and persisted for eight months postdelivery. Her first pregnancy was uneventful. Appropriate patient consent was taken.
On evaluation, she had proteinuria without haematuria or pyuria. The urine protein creatinine ratio was 2.52, serum creatinine was 0.57 mg/dl, and her kidneys looked normal on ultrasound examination. Serological examination for HIV, HBV, and HCV were negative. Evaluation for connective tissue disorders was not contributory. Hence, a kidney biopsy was performed with a spring-loaded gun under real-time ultrasound guidance for a definitive diagnosis.
On light microscopy, all the sampled glomeruli were viable, enlarged with diffuse mesangial widening which stained weakly positive by PAS, pale blue on Masson stain, and was negative with Jones silver methenamine stain. No immune deposits on immunofluorescence. The first impression was that of non-light chain amyloid, yet Congo red was negative [Figure 1]. Electron microscopy revealed haphazardly arranged curvilinear frayed bundles of banded collagen showing distinct periodicity and a diameter of 29.15 nm present in the subendothelial region and the mesangium, suggesting collagen fibrils and Type III collagen was confirmed by immunohistochemistry. The patient was prescribed an angiotensin receptor blocker and is being followed up.
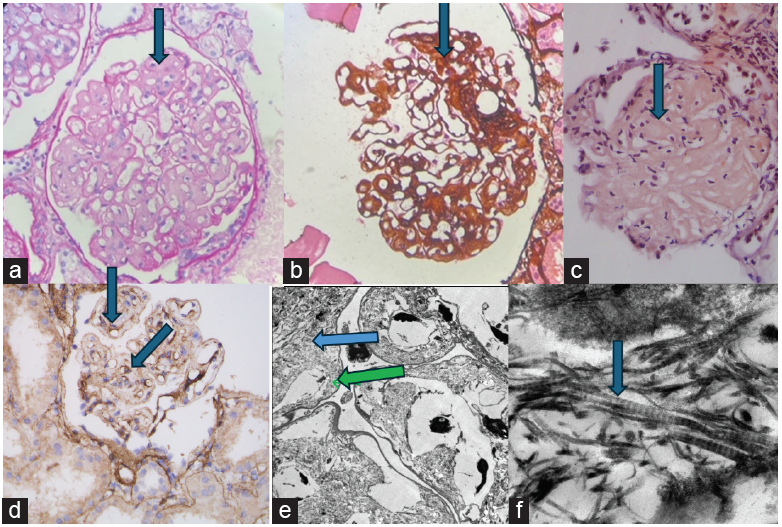
- (a) PAS negative widened mesangium (400x, blue arrow), (b) Silver negative widened mesangium, (400x, blue arrow). (c) Congo red negative widened mesangium (400x, blue arrow), (d) Type III collagen IHC, blue arrows marking peripheral and mesangial location of IHC stain. (e) Electronmicroscopy, blue arrow pointing mesangial location, green arrow pointing subendothelial location of fibrils. Original magnification 600x. (f) Electronmicroscopy, Curvilinear banded fibrils, 29.15 nm, original magnification 10000x, blue arrow.
Organized deposit disease must be considered in the differential diagnosis for any patient presenting with significant proteinuria, irrespective of age, gender, or systemic disease. Clinical history of comorbid conditions, light microscopy, immunofluorescence, and electronmicroscopy together play an important role in the diagnosis of this entity.
Conflicts of interest
There are no conflicts of interest.







