Translate this page into:
Collapsing Glomerulopathy in a Patient with Tuberculosis and Poncet’s Disease
Corresponding Author: Dr. Vinod Kumar, Aster RV Hospital, CA-37, 24th Main Road, ITI Layout, 1st Phase, JP Nagar, Bengaluru - 560 078, Karnataka, India. E-mail: drvinodkumark17@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shah Alam T, Kumar V, Thomas J, Shenoy N, Philips G. Collapsing Glomerulopathy in a Patient with Tuberculosis and Poncet’s Disease. Indian J Nephrol 2024;34:88-9. doi: 10.4103/ijn.ijn_264_22
Abstract
A 39-year-old woman presented with inflammatory polyarthritis, low-grade fever, progressive pedal edema, and frothy urination of three weeks duration. She had nephrotic range proteinuria and elevated creatinine. Kidney biopsy showed collapse of capillary tuft in the glomeruli and proliferation, hyperplasia, and hypertrophy of the overlying podocytes suggestive of collapsing glomerulopathy. Histology of the cervical lymph node showed necrotizing granulomatous inflammation suggestive of tuberculosis. With all other possible causes of polyarthritis ruled out, a diagnosis of Poncet’s disease—a form of polyarthritis observed in patients suffering from an active form of extrapulmonary tuberculosis (TB)—was considered. Association between TB lymphadenitis and collapsing glomerulopathy (CG) is very rare, and the patient had partial remission of the disease after being started on anti-tuberculosis therapy (ATT) along with steroids.
Keywords
Collapsing glomerulopathy
nephrotic syndrome
Poncet’s disease
proteinuria
tuberculosis
Introduction
Collapsing glomerulopathy (CG) is a severe, pathological form of focal segmental glomerulosclerosis and is often associated with reduced glomerular filtration rate, heavy proteinuria, and end-stage renal disease (ESRD).1 Although the exact cause of CG is unknown, it has been associated with several infections, autoimmune diseases, and medications. Among infections, rare cases of tuberculosis being associated with CG has been reported in the literature.2,3
Case Report
A 39-year-old woman presented with low-grade evening rise of temperature and multiple joint pains involving both the wrist and ankle joints associated with morning stiffness for three weeks duration. She also reported bilateral, progressive pedal edema and frothy urination.
Laboratory investigations revealed normocytic, normochromic anemia and elevated inflammatory markers like C-reactive protein (110 mg/L) and erythrocyte sedimentation rate (45 mm/h). Renal function tests revealed elevated serum creatinine (1.26 mg/dl). Urine showed microscopic hematuria (5–8 RBCs/hpf) and 3+ proteinuria. Twenty-four-hour urinary protein was 4.1 g. Serum albumin was 3.2 g/dl and serum total cholesterol was 284 mg/dl. Serological testing for antinuclear antibody (ANA), ANA profile, rheumatoid factor (RF), and anti-cyclic citrullinated peptide (anti-CCP) revealed negative results. Antibodies against HIV, hepatitis C virus (HCV), and hepatitis B surface antigen (HBsAg) were all negative. COVID reverse transcription polymerase chain reaction (RT-PCR) was negative at the time of admission. Ultrasound and computed tomography of the abdomen were normal except for ovarian cysts.
Kidney biopsy revealed collapse of capillary tuft in 3 out of 21 glomeruli with visceral epithelial cell proliferation. Two other glomeruli showed segmental sclerosis without collapse. Tubules and interstitium were unremarkable [Figure 1].
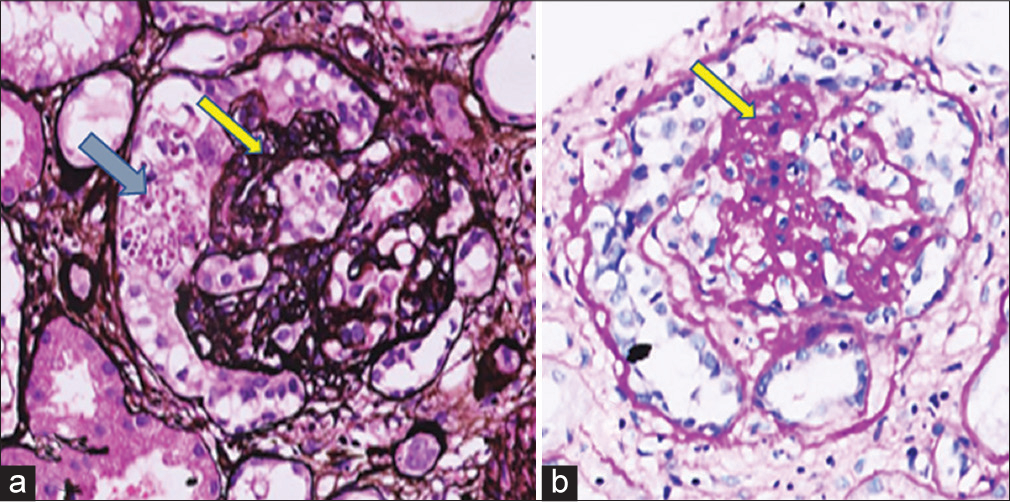
- (a) Silver stain showing collapse of glomerular tuft (arrow), with the overlying visceral epithelial cell proliferation giving an appearance of a pseudocrescent (double arrow). (b) Hematoxylin and eosin stain showing segmental sclerosis (arrow) in the glomerular tuft.
Fluoro-deoxy glucose (FDG) positron emission tomography (PET) revealed multiple small FDG-avid lymph nodes both below and above the diaphragm. Histopathology analysis of the lymph node taken from the cervical region suggested necrotizing granulomatous inflammation, indicating tuberculosis. Gene Xpert analysis from the tissue sample was positive for Mycobacterium tuberculosis. The patient was treated with 1 mg/kg of prednisolone for two months, which was slowly tapered over the next two months, and standard anti-tuberculosis therapy (ATT) consisting of isoniazid, rifampicin, pyrazinamide, and ethambutol for six months. There was partial resolution of proteinuria (1.2 g/day) and improvement in the creatinine level (1.1 mg/dl) at the end of six months, and there was complete resolution of constitutional symptoms including joint pains.
Discussion
Collapsing glomerulopathy is a morphological variant of focal segmental glomerulosclerosis (FSGS) that is characterized by segmental and global collapse of the glomerular capillaries, marked hypertrophy and hyperplasia of podocytes, and severe tubulointerstitial disease. Disorders associated with CG fall under six categories: infections, autoimmune diseases, malignancies, genetic disorders, drug exposures, and during the post-transplantation period. Apart from HIV, other common viral infections associated with CG include the Epstein–Barr virus, parvovirus B19, coxsackievirus , Cytomegalovirus, human T-cell lymphotropic virus type 1, the hepatitis C virus, and SARS-CoV-2.4–6 In our patient, most of these infections were ruled out, including SARS-CoV-2, at the time of clinical presentation. Autoimmune diseases, malignancies, and drugs implicated in the causation of CG were ruled out in our case.
The treatment of CG includes targeted therapy for nephrotic syndrome, treatment of its underlying cause, and immunosuppression. Our patient received ATT, angiotensin receptor blocker (ARB), and steroids.
Association of tuberculosis and CG has been rarely reported.1,2 Our patient had TB lymphadenitis and had inflammatory polyarthritis; however, serological evidence of autoimmune diseases yielded negative results. This was likely due to Poncet’s disease, which is a rare aseptic form of reactive arthritis and a musculoskeletal disorder seen in patients with tuberculosis. Even though synovial fluid analysis was not done in the patient, it is less likely to be TB arthritis or other infectious cause of arthritis which usually presents with monoarthritis. There was no radiological evidence of joint destruction. To the best of our knowledge, this is the first case that shows an association between Poncet’s disease and CG. Timely diagnosis and intervention with ATT and steroids have also yielded good results, as seen in our patient.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Current views on collapsing glomerulopathy. J Am Soc Nephrol. 2008;19:1276-81.
- [CrossRef] [PubMed] [Google Scholar]
- Tuberculosis-associated collapsing glomerulopathy: Remission after treatment. Ren Fail. 2010;32:143-6.
- [CrossRef] [PubMed] [Google Scholar]
- Collapsing glomerulopathy associated with pulmonary tuberculosis. Indian J Nephrol. 2016;26:373-5.
- [CrossRef] [PubMed] [Google Scholar]
- Viruses and collapsing glomerulopathy: A brief critical review. Clin Kidney J. 2013;6:1-5.
- [CrossRef] [PubMed] [Google Scholar]
- Infections and collapsing glomerulopathy. Am J Kidney Dis. 2020;76:600-1.
- [CrossRef] [PubMed] [Google Scholar]







