Translate this page into:
Deceased donor transplantation in India: How the challenges are being met?
Address for correspondence: Dr. G. Abraham, Department of Nephrology, 4A J Jayalalitha Nagar, Madras Medical Mission, Chennai - 600 034, Tamil Nadu, India. E-mail: georgi_abraham@yahoo.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Deceased donor transplantation (DDT) in the state of Tamil Nadu has made major strides since 2008 and has a deceased donor rate of 2 per million population. This is as a result of public–private partnership spearheaded by the efforts of the state transplant coordinator and the participating team.[12] This partnership has provided DDT to the underprivileged sections of the society through the participating teaching hospitals in Tamil Nadu, especially in Chennai.
In this issue of the IJN, Gopalakrishnan et al.[3] have provided retrospective data on 173 DDT over a decade from 2005 to 2015 in the marginalized sections at the Rajiv Gandhi Government General Hospital in Chennai, highlighting the factors affecting patient outcomes and graft survival.
This is an admirable retrospective analysis in a resource-poor setting comparing the demographics, rejection rates, and the complications associated with DDT. The article also shows the differences in the immunosuppressive regimens used over time and the introduction of induction agents from 2012. Cytomegalovirus prophylaxis was given to the susceptible population in a cost-effective manner, which is again commendable.
Although the manuscript does not throw new light on the factors affecting the immediate and delayed graft function (DGF) (48.5%), it emphasizes the importance of cold ischemia time, recipient age, and immediate graft function as independent predictors of patient and graft survival. The manuscript also mentions extended criteria donors (ECD) who formed 11.5% of the donations. In India, where DDT form only 4% of the total transplants, ECD may be a feasible option.[4]
Given the widespread organ shortage, the transplant units may use organs from cobra bite victims or other poisoned donors, controlled donation after cardiac death and older donors with good functioning kidneys can be considered as prospective organ donors. However, as a substantial number of donors are victims of road traffic accidents with multiple injuries with underlying sepsis, extreme caution should be exercised before retrieving organs for transplantation. As rabies-related brain deaths are common in India, donor selection should be done cautiously and meticulously to avoid mishaps.
The incidence of DGF is much higher when compared to developed countries emphasizing the need for better immunological monitoring, superiority of deceased donor management in Intensive Care Unit (ICU) and better organ retrieval techniques.
They have also highlighted the lack of gender disparity that exists in the donations compared to other parts of India. The patient and graft survival rates are comparable to other studies done in India.
One of the pressing problems related to DDT in developing countries is the high infection-related mortality which has been demonstrated by the authors also with sepsis (bacterial followed by fungal) being the major cause of death in patients with a nonfunctioning and functioning graft in both the early and late posttransplant period.
Although this manuscript has limitations, this is an important article from a free of cost government teaching hospital in India, which serves the poor through organ transplantation and follow-up.
The highlights of the article include that of transplant coordination and the beneficial impact of the same which provides an insight for all developing countries in South Asia.
Figure 1 shows the prevalence of DDT from 2012 to 2014 in various states in India which is quite encouraging in a country where live transplantations was the norm.
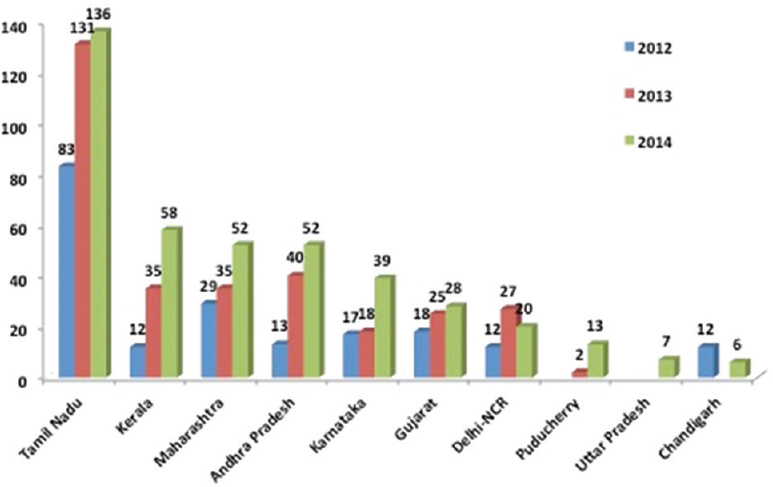
- Number of renal transplants done in different states and union territories of India from 2012 to 2014
In 2015, Professor Amalorpavanathan, the Tamil Nadu state coordinator, stated that there were 155 organ donors in the state of Tamil Nadu compared to 136 in 2014, which only demonstrates the increasing trend in DDT due to an effective counseling, coordination, and planning supported by the state government.[5]
The nongovernmental organizations, especially Multi-Organ Harvesting Aid Network (MOHAN) foundation, play a key role in propagating DDT in Tamil Nadu and other states through programs involving government authorities joining hands with like-minded organizations. The other key contribution by MOHAN foundation is the training of transplant coordinators across India to facilitate grief counseling and organ donation.[6] Persuasive and constant communication with the families of the deceased donors and transplant unit through the skilled coordinators will go a long way in increasing the donations. The ICU teams in the hospitals with and without an active transplantation program should establish performance measures, which should be periodically updated to increase deceased donations.
The initiatives taken by the Ministry of Health and Family Welfare, Tamil Nadu, in promulgating government orders on the platform of the Transplantation of Human Organs Act of India facilitated the organ donation and simplified medicolegal issues delaying transplantation.[7]
However, despite all the efforts, the program lacks in the following key aspects. There is lack of accessible centralized immunology laboratory for tissue typing and advanced immunological workup. Lack of tissue typing and hence allocation of organs as per best match is not being done, which may impact rejection and long-term survival of the allograft.
Sensitive immune surveillance techniques such as single bead Luminex assays, flow cytometry for detection of antihuman leukocyte antigen (HLA) antibodies which offers major advantages including T- and B-cell crossmatch, detection of noncomplement fixing antibodies, panel reactive antibody, and detection and monitoring of rejections by donor-specific antibody are not currently practiced as a result of financial constraints.
A combination of methodologies, monitoring the humoral and cellular immune arms should ideally be used to enhance better short- and long-term graft outcomes. An example of this would be the choice of using the donor lysate on the Luminex platform rather than the single antigen bead assay and the concern as to whether the HLA antigen profiles representative of the diverse populations in India are covered.[8]
It is critical that we innovate, adapt and build on the lessons learnt to enhance quality of care in renal transplantation.
The other critical challenge is diagnosis and management of infections in the recipient.[9] As already highlighted both by Gopalakrishnan et al. and us, infection continues to be a daunting task to combat. This issue has been brought to the notice of the state health ministry requesting them to speed up the establishment of a state-of-the-art infection monitoring facility under the government agencies. The need of the hour is a central infection control agency with satellite facilities in major transplant localities to enhance infection control activities and monitoring.
The cost of transplantation in the government-run programs is made free through government funding, which is a model for other states. However, the varying cost of transplantation for the same organ in private corporate facilities is not uniform despite sharing of the organs which is a stumbling block for prospective recipients who are waiting for a deceased donor. It is high time that the state and central governments enact laws to have uniformity in the cost of transplantation to prevent undue financial stress on the recipient.[710]
Like UNOS which oversees DDT in the fair distribution of organs in US, we need to have a centralized organ distribution system, which can cater to the remote localities in India.
The message emphasized is the need for organized bodies to augment the rate of organ donation as shown by the Tamil Nadu model. The other aspect is the need for prospective randomized controlled trials to determine the induction strategies, organ harvesting protocols, and graft and patient outcomes in DDT in India.
This paper is a testimony to the fact that DDT to the marginalized sections of the society is on par with any developed country. DDT is the way to go in the present era as discussed by the authors rightly and more efforts culminating in its propagation and better outcomes will improve the lives of end-stage renal disease patients.
References
- Cadaver organ donation and transplantation-an Indian perspective. Transplant Proc. 2003;35:15-7.
- [Google Scholar]
- Deceased donor renal transplantation: A single center experience. Indian J Nephrol. 2017;27:4-8.
- [Google Scholar]
- Outcome of deceased donor renal transplantation – A single-center experience from developing country. Saudi J Kidney Dis Transpl. 2013;24:403-7.
- [Google Scholar]
- Available from: http://www.dmrhs.org/tnos/last
- INOS and the Essence of Organ Sharing. Editorial. Indian Transplant Newsletter 2001:3.
- How deceased donor transplantation is impacting a decline in commercial transplantation – The Tamil Nadu experience. Transplantation. 2012;93:757-60.
- [Google Scholar]
- Donor-specific antibody detection: comparison of single antigen assay and Luminex crossmatches. Tissue Antigens. 2010;76:398-403.
- [Google Scholar]
- Post-transplant infections: An ounce of prevention. Indian J Nephrol. 2010;20:171-8.
- [Google Scholar]
- Evolution of renal transplantation in India over the last four decades. NDT Plus. 2010;3:203-7.
- [Google Scholar]






