Translate this page into:
Digital Gangrene in a Dialysis Patient Due to Calciphylaxis and Systemic Polyarteritis Nodosa: A Diagnostic Dilemma
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Calciphylaxis or calcific uremic arteriolopathy (CUA) is a potentially life-threatening vasculopathy of the skin and subcutaneous tissues reported in association with chronic kidney disease (CKD). Risk factors include obesity, diabetes mellitus, female sex, white ethnicity, time on renal replacement therapy, and the use of coumarin anticoagulants.[1] CUA most frequently affects the lower limbs, mainly the buttocks and thighs. Digital necrosis due to CUA is very rare.[2] We describe an unusual case of polyarteritis nodosa (PAN) in a CKD patient with hyperparathyroidism and CUA presenting with digital gangrene.
A 26-year-old female of end-stage renal disease (basic disease unclassified) on irregular hemodialysis for 2 years presented with complaints of severe painful bluish-black discoloration of hands and feet and low-grade fever, which was noticed 1 month before the admission [Figure 1]. The patient was diagnosed as end stage renal disease 2 years ago when she presented with advanced azotemia. The patient did not smoke and there was no history of jaundice, abdominal pain, melena, weakness, altered sensorium, Raynaud's phenomenon, joint pains or recurrent fetal loss. Physical examination revealed pulse rate of 96/min, blood pressure of 150/90 mmHg, respiratory rate of 16/min, and temperature of 38.4°C. Bilateral radial and dorsalis pedis pulses were absent, rest pulses were present and symmetrical with a left side radiocephalic arteriovenous fistula. A tender blackish nodule was present on the index finger of right hand and all the toes of both feet showed redness, swelling with gangrenous changes. Neurological examination revealed lower extremity bilateral distal sensorimotor neuropathy. Rest cardiovascular and abdominal examination was normal. Laboratory parameters revealed hemoglobin of 6.5 gm/dl, total leucocyte count 9,300/mm3, platelet count 3.6 × 109/L, serum urea 140 mg/dl, serum creatinine 8 mg/dl, serum calcium 8.5 mg/dl, serum phosphorus 10.8 mg/dl, intact PTH 2339 IU/ml, serum albumin 3 gm/dl, alkaline phosphatase 439 IU/ml, and normal prothrombin/activated thromboplastin time. Erythrocyte sedimentation rate and C-reactive protein were 80 mm in 1st h and 186 mg/l, respectively, suggestive of inflammatory etiology. ANA, ANCA, hepatitis B surface antigen by ELISA, cryoglobulin, antiphospholipid antibody were negative. Two-dimensional echocardiography revealed concentric left ventricular hypertrophy and diffuse myocardial calcification with an ejection fraction of 60%. Computed tomography angiography revealed extensive calcifications of bilateral internal iliac, femoral, popliteal, mesenteric arteries along with beading, and irregular outline of bilateral upper limb and mesenteric arteries [Figure 2a–d]. However, bilateral renal arteries did not show any stenosis or microaneurysm. Soft tissue calcification was observed in the gluteal region. Nerve conduction study showed sensorimotor neuropathy affecting bilateral sural and peroneal nerves. Skin biopsy done from the edge of the black nodule revealed no features of vasculitis or calcium deposition, however, biopsy core was inadequate and did not contain deeper dermis. Sestamibi parathyroid scintigraphy revealed left inferior and right superior parathyroid adenoma. The clinical presentation and investigations confirmed systemic polyarteritis nodosa with CUA. Sixty milligram of prednisolone was commenced along with intensive hemodialysis, sevelamer carbonate and cinacalcet. After 1 month of follow-up, fever subsided, skin ulcers of toes healed, neuropathy improved on examination and intact PTH decreased to 843 IU/ml. However, gangrenous changes of two toes of left foot progressed and required amputation.

- Left foot with gangrenous changes and redness, swelling of all toes with ulcer on the dorsal aspect
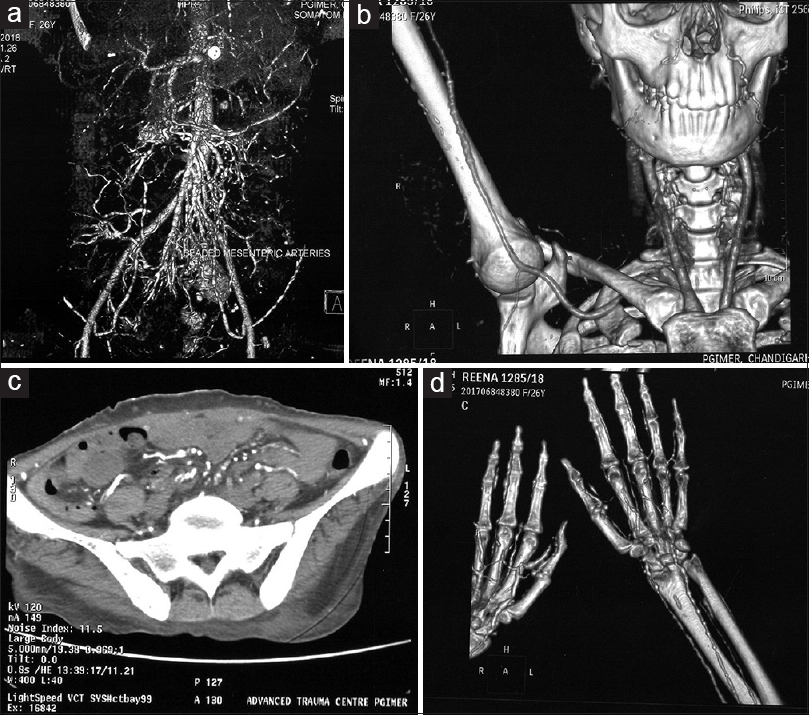
- (a) Reconstructed computed tomography angiography showing beading of mesenteric vessels. (b) Reconstructed computed tomography angiography showing beading of right upper limb arteries. (c) Noncontrast computed tomography abdomen showing calcified abdominal aorta and major vessels. (d) Reconstructed computed tomography angiography showing beading of peripheral upper limb arteries
In the index patient, the extensive soft tissue and vascular calcification with extremely high calcium phosphate product and elevated PTH favored underlying CUA. However, sudden and rapid progressing ischemic lesions along with neuropathy, constitutional symptoms, elevated inflammatory markers, absent peripheral pulses, and angiographic evidence of beading of visceral and peripheral arteries suggested an additional diagnosis of PAN. Patient was fulfilling four out of the ten classification criteria of PAN.[3] Steroids are preferred therapy in PAN.[4] Treatment of CUA is mainly supportive that includes wound care, debridement, intensive dialysis, phosphate binders, and cinacalcet. The key message of this letter is that vasculitis should be considered as a differential of CUA in a patient of CKD with digital gangrene.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
References
- Calciphylaxis causing digital, gangrene in end stage renal disease: A case report and review. West Afr J Med. 2013;32:68-72.
- [Google Scholar]
- Calciphylaxis is usually nonulcerating: Risk factors, outcome and therapy. Kidney Int. 2002;61:2210-7.
- [Google Scholar]
- The American College of Rheumatology 1990 criteria for the classification of polyarteritisnodosa. Arthritis Rheum. 1990;33:1088-93.
- [Google Scholar]
- Cutaneous polyarteritis nodosa presented with digital gangrene: A case report. J Korean Med Sci. 2006;21:371-3.
- [Google Scholar]






