Translate this page into:
Direct costs associated with chronic kidney disease among type 2 diabetic patients in India
Address for correspondence: Dr. Vijay Viswanathan, M.V. Hospital for Diabetes and Prof. M. Viswanathan Diabetes Research Centre (WHO Collaborating Centre for Research, Education and Training in Diabetes), No. 4, West Madha Church Street, Royapuram, Chennai - 600 013, Tamil Nadu, India. E-mail: drvijay@mvdiabetes.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The aim of this study was to estimate the direct costs of medical care among hospitalized type 2 diabetic patients with chronic kidney disease (CKD). A total of 209 (M:F, 133:76) patients were divided into groups based on the severity of kidney disease. Group 1 subjects had undergone renal transplantation (n = 12), group 2 was CKD patients on hemodialysis (n = 45), group 3 was patients with CKD, prior to end-stage renal disease (ESRD) (n = 66), and group 4 (n = 86) consisted of subjects without any complications. Details about expenditure per hospitalization, length of stay during admission, direct medical and nonmedical cost, expenditure for the previous two years, and source of bearing the expenditure were recorded in a questionnaire. Diabetic patients with CKD prior to ESRD spend more per hospitalization than patients without any complications. [Median ₹ 12,664 vs. 3,214]. The total median cost of CKD patients on hemodialysis was significantly higher than other CKD patients (INR 61,170 vs. 12,664). The median cost involved in kidney transplantation was ₹ 392,920. The total expenditure for hospital admissions in two years was significantly higher for dialysis than transplantation. Patients on hemodialysis or kidney transplantation tend to stay longer as inpatient admissions. The source of funds for the expenditure was mainly personal savings (46%). The expenditure on hospital admissions for CKD was considerably higher, and so, there is a need to develop a protocol on a cost-effective strategy for the treatment of CKD.
Keywords
Chronic kidney disease
cost estimates
India
type 2 diabetes
Introduction
Diabetes is a major public health problem associated with premature death with high costs of treating complications.[12] It is estimated that globally, the total number of people with diabetes will rise from 366 million in the year 2011 to more than 550 million in 2030.[3] In India, more than 60 million people suffer from diabetes, that is, almost 8.3% of the adult population, and by 2030, around 9.4% of the adult population will suffer due to rise in life expectancy and urbanization.[3] Diabetes is a chronic disease that requires lifelong continuous medical care. It is well established that the care and treatment of diabetes patients consumes large amounts of health-care resources. The care of diabetes and its complications presents a challenge for most health-care professionals in developing countries like India.
The average annual direct costs of hospitalized patients are more than double of those not hospitalized.[4] It was also reported that inpatients having diabetes without complications spent 11-75% of their income on hospital admission, whereas patients having diabetes with complications spent 6-300% of their income in the same hospital.[5] The burden of chronic kidney disease (CKD) among the diabetic population remains to be a global threat as the treatment is expensive and lifelong. There is a widespread increase in the percentage of expenditure on long-term treatment of complications like CKD in diabetes. In 1997, the direct cost spent on diabetes was found to be US dollars (USD) 44.1 billion in the United States, of which 27% of the expenditure was related to treat cardiovascular, renal, and ophthalmic complications.[1]
Diabetes is the leading cause of end-stage kidney failure necessitating dialysis or transplantation. Almost 70% of the Indian population is in the below-poverty-line category, and although the cost spent on dialysis is comparatively cheaper than other countries, 90% of the Indians cannot afford it.[6] In India, around 3,500 transplants are being done each year.[7] According to the Dialysis Outcomes and Practice Patterns Study (DOPPS), the long-term cost involved in kidney transplantation was comparatively lesser than in dialysis treatment, and the survival rate of patients who underwent kidney transplantation was also higher than that of dialysis treatment.[8]
The economic consequences of CKD have not been well enumerated. Due to lack of information on costs involved for diabetic subjects with renal disease in developing nations like India, this study was planned with an aim to assess the direct expenditure involved for treating hospitalized type 2 diabetic subjects with CKD in comparison with diabetic subjects without any complications.
Materials and Methods
This cross-sectional study was done at two centers between August 2008 and January 2010: One a specialized diabetes care center, exclusively treating diabetic patients, and another private hospital. A total of 209 (M:F = 133:76) type 2 diabetic subjects were included. The recruited study subjects were randomly selected type 2 diabetic patients with CKD and were compared with a group of subjects without any diabetic complications seeking treatment for the management of diabetes. Subjects with the presence of two or more complications were excluded from the study. We defined stages of renal disease (CKD stages I-IV) as end-stage renal disease (ESRD),[9] long-term hemodialysis, or renal transplantation, and based on the severity of renal disease, the subjects were stratified into the following groups: Group 1 (n = 12; M:F = 7:5) were patients who had undergone renal transplantation, group 2 (n = 45; M:F = 27:18) were CKD diabetic patients who were on hemodialysis, group 3 (n = 66; M:F = 50:16) were patients with CKD prior to ESRD, and group 4 (n = 86; M:F = 49:37) were type 2 diabetic patients without any complications. All the subjects were enrolled at the specialized diabetes care center. Group 1 and group 2 subjects were referred to the private hospital for transplantation and hemodialysis, respectively. Group 3 patients were admitted at the specialized diabetes care center to manage both diabetes and CKD, and group 4 was admitted in the same center to manage diabetes. The study was approved by the ethics committee of the institution and written informed consent was obtained from the recruited patients.
A pretested questionnaire consisting of the details on expenditure toward the care and management of CKD and diabetes was administered by interviewing the patient. The subject's anthropometric and demographic details like gender, age, body mass index (BMI: Kg/m2), and family history of diabetic nephropathy were recorded. Other details like locality (urban or rural), educational status and occupation details, and habits were also noted for all the four groups. Biochemical parameters like fasting plasma glucose, postprandial plasma glucose, glycosylated hemoglobin, and renal function were recorded. Urea and creatinine values reported for subjects in group 1 (transplantation) were measured before transplantation. Socioeconomic status and cost of all inpatient care, which include direct medical and nonmedical costs in Indian currency, were recorded. The details of direct cost per unit per patient were assessed based on the expenditure on laboratory charges (initial admission), medical consultations (initial admission), medicines cost (monthly), and expenditure per hospitalization (surgery cost, bed charges, nursing charges, etc.) for group 1, dialysis charges, bed charges, and nursing charges for group 2, and bed charges and nursing charges for groups 3 and 4. Transportation cost was also recorded for each group. The reason for hospitalization, the length of stay during admission, and total expenditure for the past two years to manage both CKD and diabetes and mode of payment of hospital bills were also documented. The data on expenditure were obtained from the hospital bills and expenditure details of the previous two years were obtained from the records maintained by the patients. The cost involved for treating CKD and managing diabetes were recorded separately from the hospital bills. The questionnaire was administered by a single research officer who was well trained, and the entire process of data collection took about 45 minutes per patient.
Statistical analysis
Mean ± standard deviation (SD) and proportions are reported for the variables. Due to the skewed distribution of the cost variables, the median values and ranges are reported. Median test was used for intergroup comparisons. For other multiple-group comparisons, analysis of variance (ANOVA) posthoc testing with Tukey HSD (honestly significant difference) procedure was used, and χ2 test with Yates's correction was used for comparison of proportions. A P < 0.05 was considered as statistically significant. The SPSS package version 16.0 (Illinois, USA) was used for statistical analysis.
Results
Table 1 shows the demographic, anthropometric, and clinical details of the study groups. Group 3 patients with different CKD stages were older compared to the other three study group patients (P < 0.0001). Group 1 and group 2 patients had similar BMI. Group 3 and group 4 patients had a significantly higher BMI than group 1 and group 2 patients. The presence of positive family history of diabetic nephropathy differed between the study groups (P < 0.0001). Occupation and educational status showed differences between the study groups. Majority of the study subjects belonged to the urban location. Total family income varied among study groups (χ2= 17.4; P = 0.008). Approximately 40% of the patients in the transplantation group had a family income of more than 20,000 ₹/month and it was less than 25% in the remaining study groups. Smoking and alcohol consumption habits were similar among the study groups (χ2= 11.7; P = 0.699). More than 70% of the study subjects were nonvegetarians.

Table 2 shows the biochemical details of the study groups. Plasma glucose levels and glycated hemoglobin (HbA1c) percentage did not differ between the study groups. Plasma urea and creatinine levels showed a statistically significant difference between the study groups (P < 0.0001).
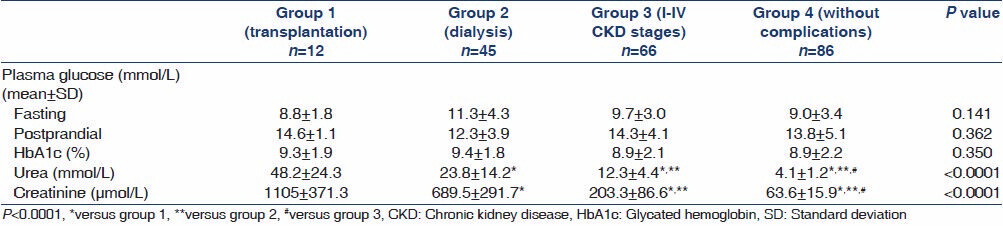
Table 3 summarizes the total costs associated with CKD among type 2 diabetic patients. The diabetic patients on dialysis (median: 5; range: 2-25 days) or kidney transplantation (median: 12; range: 4-20 days) tend to stay longer as inpatient admissions. Patients on transplantation spent more on initial and monthly maintenance medicine cost [initial 32,500 INR vs. monthly maintenance 7,500 ₹] than patients on dialysis [initial 4,500 ₹ vs. monthly maintenance 2,000 INR]. The total medicine cost in treating both diabetes and CKD was significantly higher for patients on renal transplantation (40,400 ₹). The laboratory charges for patients on renal transplantation (59,500 ₹) were also higher compared to patients on hemodialysis (2000 INR). The consultation fee was significantly higher for patients on transplantation (62,500 ₹) when compared to patients on dialysis (30,000 ₹). The total consultation fees for treating diabetes and CKD was highest for patients on transplantation (67,000 ₹). The transportation charges was high for patients on hemodialysis (3,480 ₹) followed by patients on transplantation (3,250 ₹), and it was much lesser for patients without any complications (300 ₹). The hospitalization charges, which included surgery cost and so on, were significantly higher for the transplantation group (215,000 ₹) than the dialysis group (22,000 ₹). The hospitalization charges were lesser for patients without any complications (1,082 ₹).

On an average, diabetic patients with CKD prior to ESRD spent more per hospitalization than patients without any complications. Median was INR 12,664 (range: ₹ 4465-57,400) versus 3,214 ₹ (USD 69) (range: 250-10,000 ₹). The total median cost for CKD patients on dialysis was significantly higher than other CKD patients (₹ 61,170 vs. 12,664). The cost for a person on hemodialysis was four times higher than for persons with CKD only. The median cost involved in renal transplantation was ₹ 392,920 (range 50,800-527,000 ₹). The total median expenditure for previous two years showed significant differences between the study groups (group 1: ₹ 345,000; group 2: ₹ 500, 000; group 3: ₹ 100,000; group 4: ₹ 30,000). The total median expenditure for hospital admissions in two years was significantly higher for patients on hemodialysis than transplantation (P < 0.0001). Overall, the cost of care associated with early signs of renal disease to the onset of chronic renal failure increased dramatically. In general, the source of funds for the expenditure in treating CKD was mainly personal savings (46%), followed by medical insurance (23%), mortgage (12.4), loan (10.0%), company reimbursement (6.2%), and sale of property in 2.4% patients.
The reasons for hospitalization were either to undergo a renal transplantation or hemodialysis. The CKD patients were admitted due to elevated renal parameters. The group of patients without any complications was admitted to have a general checkup, due to severe hyperglycemia or because of frequent hypoglycemic symptoms. A small proportion of subjects was admitted due to several other reasons related to diabetes. The presence of other complications in the study groups were as follows: Four patients in group 1 had hypertension. In group 2, 10 patients had hypertension, 12 patients had the presence of retinopathy, and five had heart problems. In group 3, one patient had foot infection, one had hypertension, and one patient had retinopathy.
Discussion
The alarming increase in the prevalence of diabetes has an impact on the costs of management of diabetes and its complications in developing countries, especially India. This rise directly affects health-care costs. One of the recent population-based studies highlighted the median annual direct and indirect cost associated with diabetes care in India. The annual cost for diabetes was 1,541.4 billion INR in 2010, by extrapolating the direct and indirect cost estimates to the Indian population.[10] Therefore, the cost of diabetes care is high and it further escalates in the presence of complications. Thus, the complications of diabetes may involve expensive treatment in estimates of direct costs. One of the serious complications of diabetes is ESRD, and diabetic patients were found to face more expenses than nondiabetic patients for ESRD treatment.[11]
The current study evaluated the direct costs associated with CKD among type 2 diabetic patients. The patients with CKD spent more per hospitalization than patients without any complications. The study findings revealed that patients who had undergone renal transplantation or who were on hemodialysis tend to stay longer for inpatient admissions. The cost for a diabetic person on hemodialysis was four times higher compared to people prior to the ESRD stage. An earlier study from India reported that cost per dialysis in India ranges from 150 ₹ in government hospitals to 2,000 ₹ in private hospitals. In most of the private hospitals, the monthly average cost of dialysis is 12,000 ₹, and the yearly cost is 140,000 ₹ equivalent of USD 3,000, and this is in sharp contrast to the annual cost of USD 60,000 in the United States and the United Kingdom. The average cost of kidney transplant varies from 50,000 ₹ in a government setup to 300,000 INR in an average private hospital.[6] In the context of the public sector, a recent study from India also showed that the cost of having a kidney transplantation in a public sector hospital is far lesser than that reported anywhere else in the world.[12]
The present study has shown that the median cost for patients on dialysis was 49,500 ₹, which includes initial and monthly maintenance medicine cost, laboratory charges for CKD, consultation fees, transportation charges, and hospitalization charges. More than 70% of the patients in the dialysis group had dialysis eight times per month. Patients should undergo 12 dialysis sessions per month as per recommendation; because many of the patients in the study could not afford it, they voluntarily reduced the number of sessions. The cost of diabetes treatment is an out-of-pocket expenditure for many patients in developing countries such as India. In the absence of insurance policies for diseases such as diabetes and meager financial support from the public health-care sector, patients spend from their personal savings and face a huge financial crisis. Recently, in the state of Tamil Nadu in India, a scheme was launched by the government to provide some financial support to the patients undergoing renal dialysis, which could really help in reducing the economic burden of such patients. Nevertheless, the presence of such schemes in other parts of the country is doubtful, and not all patients tend to access such facilities in India.
The cost-effectiveness of three modalities of treatment was tested by Gonzalez-Perez et al.[13] Satellite hemodialysis was less costly than home dialysis; home dialysis was less costly than hospital dialysis. However, there are several issues, which need to be noted while interpreting the results of the above study. Transport costs were not included in the analysis, and the cost estimates for satellite hemodialysis do not include the costs of more skilled nurses or the training of additional nurses. If the above issues were considered, the results would have been different.[13] We could not compare such data because all our patients were on hospital dialysis. In another study in a large tertiary care hospital in Karnataka, India, it was reported that patients with diabetes and chronic renal failure requiring dialysis spent 14 times more than those without any associated complications.[14] The average length of stay in the hospital was 10.3 days, whereas it was 4 (1-12) days in our CKD (stage I-IV) study group.
The cost of renal transplant also varies between the government sector and the private sector. The cost of a renal transplant procedure is USD 700 to 800 in the government sector and USD 6,000 in the private sector.[15] Our findings are consistent with the above reports. The results of the current study reveal that the median cost involved in renal transplant was 392,920 INR (USD 8450). The transplant was from a living donor and the cost involved in monitoring the donor was not included in this study. The total medicine cost and consultation fees in treating both diabetes and CKD was significantly higher for patients on renal transplantation. Patients on transplant spent more for initial and maintenance medicine cost than patients on dialysis. The laboratory charges for patients on renal transplantation were also higher compared to patients on dialysis. The hospitalization charges were lesser for patients without any complications. The hospitalization charges, which include surgery cost also were significantly higher for the transplantation group than the dialysis group.
The total median expenditure for hospital admissions in two years was significantly higher for patients on dialysis than transplantation. Thus, on a long-term basis, renal transplant remains a cheaper option of treatment modality for ESRD in India in comparison with dialysis. Earlier reports also suggest that patients who undergo kidney transplantation have longer survival and better quality of life than patients on either hemodialysis or peritoneal dialysis.[1617] Furthermore, the long-term cost of transplantation is lower than remaining on a dialysis modality.[18] Transplantation is usually the favored option; however, as the number of donor kidneys are limited, many of the patients already on dialysis require lifelong dialysis.
The annual costs for dialysis at Taiwan for both inpatient and outpatient were USD 25,576 per patient-year.[19] Simpson et al., found that the direct expenditure used up for diabetes was USD 134.3 million, of which USD 10 million (7.5%) was associated with renal-related services. It was also evidenced that the cost spent on cardiovascular and renal complications was found to be higher among Indians registered in the study.[20] The cost of renal replacement therapy in New Zealand is conservatively estimated at NZ $ 90 million annually based on 2003 figures.[21] The total costs reported in this study cannot be compared with studies done in developed countries because of differences in economic and social settings between developing and developed countries.
In the absence of medical insurance facilities for patients with CKD or ESRD in India, there are various other sources from which patients spent money for treatment. The source of funds for the expenditure for treating CKD was mainly from personal savings (46%).
The current study highlighted most of the components of direct costs involved in treating CKD, but indirect cost was not included, which further has an impact on the costs of CKD treatment in India. Thus, the inpatient costs tend to be the largest contributor to direct health-care costs. There are a few limitations to the present study. First, the sample size was small, and secondly, because the data were collected in a specialized diabetes care center and in a private hospital, generalizability of results may be limited to private health-care centers. The huge amount which is being spent on diabetes can be brought down by preventing patients from progressing to stage III chronic kidney disease and also to end-stage renal failure with postevent cardiovascular disease.[8] Improvement in diabetes control has the potential to reduce direct costs involved in the treatment of complications.[22]
In a developing country like India with the largest number of people with diabetes and its complications, the cost of treatment may further escalate unless intervention is initiated early to prevent or control diabetes complications. The plan has to be implemented by targeting good glycemic control, effective management of complications, and creating awareness about diabetes and its complications among the public.
In conclusion, our results showed that the direct health-care costs on hospital admissions for treating CKD are considerably greater than for those without any complications. Information on the length of stay for hospital admission and direct costs may help to emphasize the prevention of complications of diabetes; finally, there is a need to develop a protocol on a cost-effective strategy for treating complications such as CKD.
Acknowledgment
The authors acknowledge the help rendered by Ms. M. Dhivya in the preparation of the manuscript.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Economic consequences of diabetes mellitus in the U.S. in 1997. American Diabetes Association. Diabetes Care. 1998;21:296-309.
- [Google Scholar]
- Excess costs of medical care for patients with diabetes in a managed care population. Diabetes Care. 1997;20:1396-402.
- [Google Scholar]
- International Diabetes Federation Atlas (5th ed). Brussels, Belgium: International Diabetes Federation; 2011.
- Inpatient treatment of diabetic patients in Asia: Evidence from India, China, Thailand and Malaysia. Diabet Med. 2010;27:101-8.
- [Google Scholar]
- Chronic kidney disease in India: Challenges and solutions. Nephron Clin Pract. 2009;111:e197-203.
- [Google Scholar]
- Kidney transplantation and wait-listing rates from the international dialysis outcomes and practice patterns study (DOPPS) Kidney Int. 2005;68:330-7.
- [Google Scholar]
- National Institute for Health and Care Excellence. Chronic kidney disease: Early identification and management of chronic kidney disease in adults in primary and secondary care. Clinical guidelines 2008 September
- [Google Scholar]
- The socioeconomics of diabetes from a developing country: A population based cost of illness study. Diabetes Res Clin Pract. 2010;89:334-40.
- [Google Scholar]
- Kidney transplantation is associated with catastrophic out of pocket expenditure in India. PLoS One. 2013;8:e67812.
- [Google Scholar]
- Hemodialysis for end-stage renal disease: A cost-effectiveness analysis of treatment-options. Int J Technol Assess Health Care. 2005;21:32-9.
- [Google Scholar]
- A study of the direct cost incurred by Type-2 diabetes mellitus patients for their treatment at a large tertiary- care hospital in Karnataka, India. J Acad Hosp Admin. 2003;15:7-12.
- [Google Scholar]
- Chronic kidney disease and its prevention in India. Kidney Int Suppl. 2005;98:S41-5.
- [Google Scholar]
- Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation and recipients of a first cadaveric transplant. N Engl J Med. 1999;341:1725-30.
- [Google Scholar]
- Guided medication dosing for inpatients with renal insufficiency. JAMA. 2001;286:2839-44.
- [Google Scholar]
- The impact of diabetes on economic costs in dialysis patients: Experiences in Taiwan. Diabetes Res Clin Pract. 2001;54(Suppl 1):S47-54.
- [Google Scholar]
- The cost of major comorbidity in people with diabetes mellitus. CMAJ. 2003;168:1661-7.
- [Google Scholar]
- Preventable kidney failure: The cost of diabetes neglect? N Z Med J. 2006;119:U2338.
- [Google Scholar]
- Costs of temporary and permanent disability induced by diabetes. Diabetes Care. 1991;14:593-6.
- [Google Scholar]







