Translate this page into:
Embolic occlusion of arteriovenous fistula due to infective endocarditis
Address for correspondence: Dr. Rapur Ram, Nephrology, Sri Venkateswara Institute of Medical Sciences, Tirupati, Andhra Pradesh, India. E-mail: ram_5_1999@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
A 45-year-old male on maintenance hemodialysis through right radio cephalic arteriovenous fistula (AVF) also had mitral regurgitation. He presented with fever and chills of 2 days duration along with pain and swelling at median cubital fossa of right upper limb. Local examination revealed warmth, redness, and tenderness at median cubital fossa. AVF thrill was absent. Echocardiography revealed vegetations on the mitral valve. An extensive search of literature did not reveal an instance of embolic occlusion of AVF due to vegetations of infective endocarditis.
Keywords
Arteriovenous fistula
embolism
infective endocarditis
vegetation
Introduction
Systemic embolization occurs in 22-50% of patients of infective endocarditis (IE).[1] Emboli often involve major arterial beds, including lungs, coronary arteries, spleen, bowel, and extremities. There were reports of embolization even to coronary arteries.[2] We report a case of embolic occlusion of arteriovenous fistula (AVF) due to embolism from vegetations of.
Case Report
A 45-year-old male has been on regular follow-up for hypertension induced chronic renal failure for the last 10 years. He was also diagnosed with mitral regurgitation secondary to rheumatic heart disease. A right radio cephalic AVF was secured about 3 years back when the serum creatinine was 4.5 mg/dl. He was initiated on maintenance hemodialysis 6 months ago through AVF. During the 3rd month of hemodialysis, he presented with fever and chills of 2 days duration. The fever was continuous. He also complained of headache, myalgia, night sweats, shortness of breath, and cough. The blood pressure was 140/60 mm Hg and pulse rate 120 beats/min. The oral temperature was 104°F. Cardiovascular system examination revealed absent first heart sound, a third heart sound and a holosystolic murmur of grade III. The murmur was most prominent at the apex and radiated to axilla. Respiratory system examination revealed bilateral diffuse coarse crackles. He immediately underwent hemodialysis through AVF. There was no swelling, warmth or redness of AVF or right upper limb on that day. Next morning, he complained of pain and swelling of right upper limb. Examination revealed warmth, redness and tenderness at median cubital fossa. The thrill of radiocephalic AVF was absent. The Doppler of right upper limb revealed echogenic thrombus at proximal radial artery extending 2.8 cm from the bifurcation, and there was another thrombus at proximal ulnar artery. On color Doppler, there was no blood flow at fistula.
Echocardiography revealed mitral regurgitation with jet area >8 cm2 and vena contracta width >7 mm, a large vegetation >10 mm in diameter on posterior leaflet of mitral valve [Figure 1], the leaflet was thickened and had restricted movement. Aortic and tricuspid valves were normal, mild tricuspid regurgitation, and mild pulmonary arterial hypertension were recorded. Blood cultures grew coagulase-negative Staphylococcus aureus. He was treated with vancomycin (20 mg/kg after dialysis once in 3 days for 6 weeks) and gentamicin (loading dose: 1.5 mg/kg followed by 1 mg/kg/after every dialysis session for 2 weeks). On the day 2 of admission, AVF was explored.
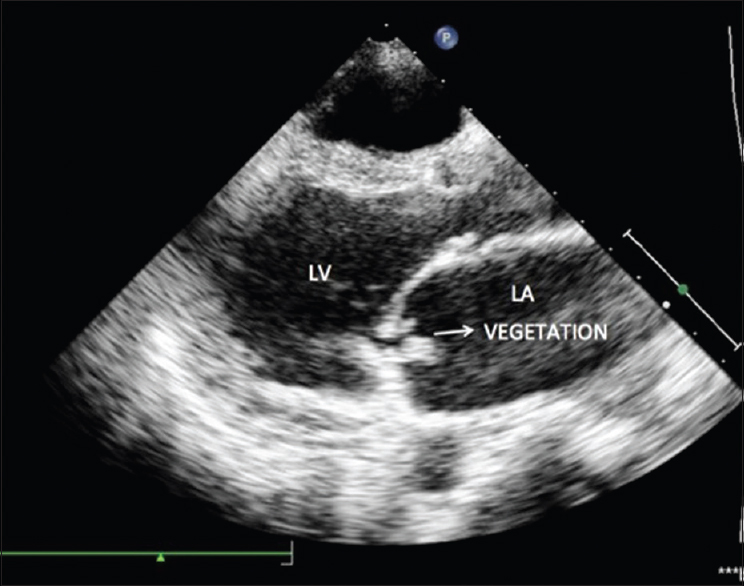
- Echocardiography: Large vegetations on posterior leaflet of mitral valve on its atrial surface. LA: Left atrium, LV: Left ventricle
On exploration [Figure 2], septic emboli were found lodged at the bifurcation of the brachial artery. The proximal radial artery was necrosed and friable. The ulnar artery, having luminal continuity with the brachial artery at bifurcation, contained septic emboli. The walls of the distal brachial artery and proximal ulnar artery were glistening off white in color and firm in consistency. Thrombectomy of the brachial artery proximal to the bifurcation was done through a transverse arteriotomy. A Fogarty catheter was passed into the ulnar artery through the arteriotomy and the embolus removed. The rent at the origin of the radial artery were repaired and distal end ligated. The culture of emboli also showed growth of coagulase-negative S. aureus.
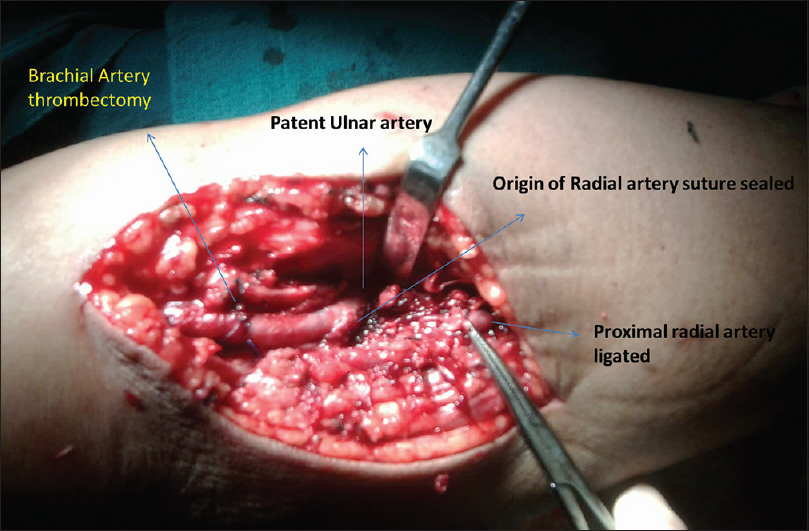
- Intraoperative photograph showing brachial artery thrombectomy, necrosed origin of radial artery suture sealed with the distal end of radial artery ligated
The fever subsided in 2 days. The pain, warmth and redness also subsided. Patient was continued dialysis through left internal jugular vein catheter. An echocardiogram after 4 weeks showed a reduction in the size of vegetation on the posterior mitral leaflet of mitral valve.
Discussion
Thrombosis is the important complication of hemodialysis AVF. The incidence of thrombosis is 0.5-2.5/patient/year.[3] The etiologies of vascular access thrombosis may be considered as those causing early (0-3 months) or late (>3 months) thrombosis. Early thrombosis is most commonly due to a technical error such as a choice of poor vein or narrowing of the lumen of the artery or vein during anastomosis. Thrombosis can also result from external compression for hemostasis, hypotension, dehydration, or early puncture of an immature vein. Late thrombosis can be due to repeated trauma from needle punctures with subsequent fibrosis and narrowing, hypotension, dehydration, compression, or trauma. However, it is most commonly due to an acquired stenosis of the runoff vein, attributed to mechanical endothelial damage from the shearing effect of the high pressure or the pulsatile arterial blood flow in the venous system leading to venous intimal hyperplasia. This patient highlights that when there was a thrombosis of an AVF with fever, IE should also be considered. The present patient had no other cause for sudden occlusion of AVF as successful dialysis was done a day before, and there were no signs of inflammation then. Thrombolytics are usually avoided in patients with septic embolization because of concerns about concurrent intracerebral mycotic aneurysms and the risk of hemorrhage.[4] After extensive literature search, we could not find a similar report.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Diagnosis and management of infective endocarditis and its complications. Circulation. 1998;98:2936-48.
- [Google Scholar]
- Infective endocarditis - An evolving disease. A review of endocarditis at the Columbia-Presbyterian Medical Center, 1968-1973. Medicine (Baltimore). 1978;57:105-27.
- [Google Scholar]
- Hemodialysis access imaging: Comparison of flow-interrupted contrast-enhanced MR angiography and digital subtraction angiography. Radiology. 2002;225:829-34.
- [Google Scholar]







