Translate this page into:
Extending the longevity of a complicated arteriovenous fistula using endovascular intervention
Address for correspondence: Dr. Basant Pawar, Senior Specialist Renal Clinician, Alice Springs Hospital, Alice Springs, Northern Territory 0871, Australia. E-mail: basant.pawar@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
A brachiocephalic arteriovenous fistula was complicated by a central venous stenosis, which could not be relieved. A cephalojugular bypass was performed using an interpositoned graft, which later developed tight stenoses at both ends of the graft. This was successfully treated with endovascular intervention, extending the longevity of the vascular access.
Keywords
Central venous stenosis
cephalojugular bypass graft
endovascular intervention
Introduction
A patient with complex vascular access problems is reported. After a left-sided arteriovenous fistula (AVF) failed, a right-sided brachiocephalic AVF was constructed, which subsequently was complicated by complete central venous stenosis. A right cephalic vein to internal jugular veno-venous bypass using an interpositioned Goretex graft was performed. Subsequently, the patient developed tight stenoses at both ends of the graft. These stenotic lesions were successfully relieved with percutaneous transluminal angioplasty.
Case Report
A 45-year-old gentleman of Australian indigenous ethnicity has been on maintenance hemodialysis since 2010 for chronic kidney disease, presumed to be secondary to diabetic nephropathy. He had long-standing diabetes mellitus complicated by diabetic proliferative retinopathy and hypertension. In the past, he was treated for a posttraumatic urethral stricture, with an optical urethrotomy.
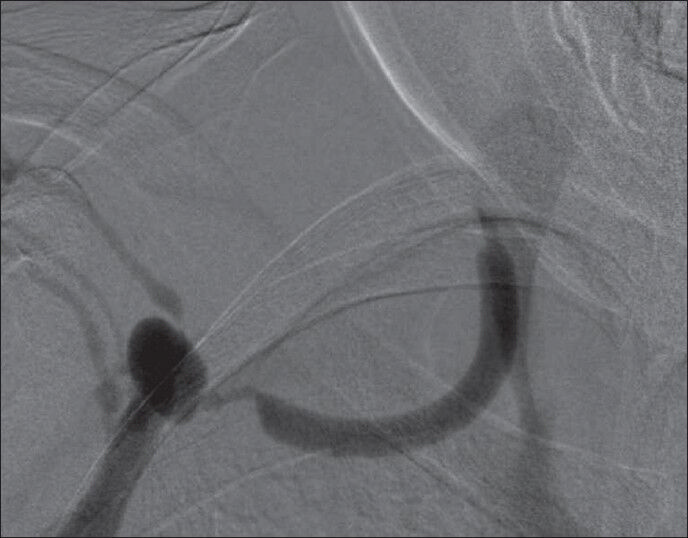
His initial dialysis vascular access was a left brachiocephalic AVF, which was lost to thrombosis which could not be surgically rescued. A right-sided internal jugular tunnelled line was used to sustain dialysis. A right brachiocephalic AVF was successfully constructed on 11/01/11. Over the ensuing months, he developed increasing venous pressures and deteriorating clearances. A digital subtraction arteriovenous fistulogram done on 15/06/11 revealed the presence of collateral veins and a complete stenosis of the distal subclavian vein [Figure 1], which could not be negotiated using endovascular techniques.
A right cephalic vein to internal jugular veno-venous bypass using an interpositioned Goretex graft was performed by vascular surgeons on 10/08/11. Hemodialysis was continued using the right brachiocephalic AVF. His venous pressures on dialysis, urea reduction ratios, and KT/V remained satisfactory.
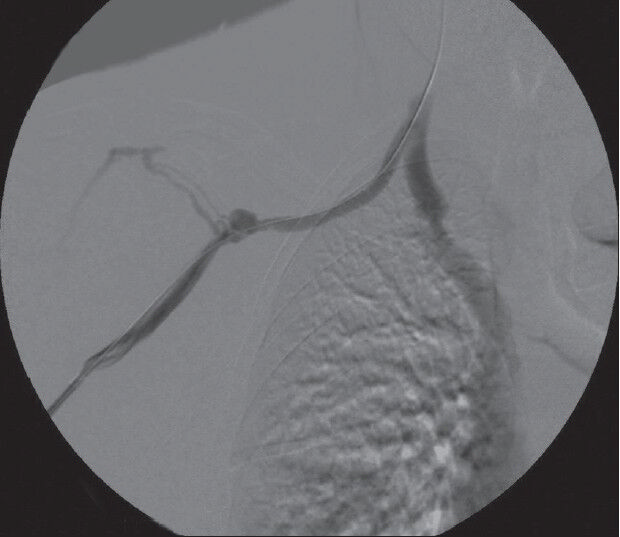
A surveillance fistulagram was performed on 15/06/12 because of rising venous pressures, revealed the presence of significant stenosis (>50%) at both ends of the veno-venous graft [Figure 2]. The stenotic segment could not be negotiated using standard 0.035 guide wire. Hence, a hydrophilic glidewire was guided over a Vanshie guiding catheter to cross the stenotic segment. A No. 8 Bard Conquest high pressure balloon was passed over the guide wire, and the stenotic segments at both ends of the graft were sequentially dilated [Figure 3]. Postdilatation contrast runs showed that the stenoses were satisfactorily relieved [Figure 4]. Since then, the patient has been undertaking hemodialysis without problems.

- Fistulagram demonstrating central venous stenosis with collaterals
- Fistulagram showing stenosis at both ends of the interpositioned veno-venous graft

- Balloon angioplasty of the stenosis with a tight “waist”
- Postpercutaneous angioplasty fistulagram with satisfactory relief of the stenoses at both ends of the graft
Discussion
The first report related to endovascular treatment of dysfunctional AVF has been attributed to Glanz et al.,[1] when in 1984 they reported their experience with a high rate of technical success.
The risk factors for central venous stenosis include central venous catheter insertions with a long dwell time.[23] The location of the catheter is important, subclavian placements result in a much higher incidence as compared with internal jugular catheters 42% versus 10%.[4567] This has resulted in most units encouraging the use of the internal jugular over the use of the subclavian vein. The increased use of peripherally inserted central catheters has also contributed to an increase in the incidence of central venous stenosis,[8] as have the use of pacemaker and defibrillator wires, and the subsequent placement of AVF.[91011]
The diagnosis of central venous stenosis is based on a number of clinical and radiological findings. These include: History of previous central venous catheter placement, with ipsilateral arm, breast, face, or neck swelling, or ipsilateral pleural effusions. Many patients will have evidence of AV access dysfunction. On physical examination, there may be numerous dilated collaterals in the neck or chest and arm edema, on the side of the central stenosis. The vascular access itself may become tortuous and aneurysmal, with multiple collaterals arising from it. There may be decrease in access flow, increased recirculation, increased venous pressures, and increased bleeding while removing dialysis needles.[121314]
Central venous stenosis can be diagnosed by duplex ultrasound, which may demonstrate an absence of normal respiratory variation in the diameter of central veins and polyphasic atrial waves.[15] Digital subtraction central venography is the gold standard for the diagnosis of central venous stenosis and is more sensitive than duplex ultrasound.[16] All patients undergoing diagnostic fistulagraphy for AV access dysfunction should undergo complete access circuit venography, to rule out central venous stenosis. Magnetic resonance venography is an alternative to conventional venography, with no significant literature to date on the assessment of central venous stenosis. However, it should be noted that patients with decreased glomerular filtration rate are at risk of developing nephrogenic systemic fibrosis.[17]
Endovascular treatment is now the mainstay of treatment. The K/DOQI guidelines recommend percutaneous angioplasty (PTA), with or without stent placement as the preferred treatment approach.[19] PTA has demonstrated a variable technical success rate ranging from 70% to 90%.[20] Bare metal stents (BMSs) were first placed in the dialysis access circuit, for refractory stenoses by Günther et al., in 1989.[16] The use of a BMS in HD access PTA interventions has significantly increased from 0% in 1991 to over 9% in 2001 according to the United States Renal Data System. The exponential increase in BMS usage in HD access procedures has led to the development of guidelines for its applications. The Society of Interventional Radiology Quality Improvement Guidelines recommend BMS be reserved for central vein lesions in which PTA has failed or that recur within 3 months after initially successful PTA; or rupture after PTA.[2122] There is minimal literature on covered stent usage in the hemodialysis access circuit. Most of the literature to date has been on the treatment of graft or outflow vein aneurysms and refractory venous outflow stenoses.[232425]
In a patient where endovascular options have run out, surgery must be considered. Central venous stenosis can be treated by extraanatomic bypass, including jugular vein turn down procedures, subclavian vein to external or internal jugular vein bypass, or axillary to femoral vein bypass. Surgical options for central venous stenosis are associated with significant morbidity in patients and are a second-line treatment alternative in patients refractory to percutaneous endovascular treatment options.[26]
This patient had failure of his first access, a left-sided brachiocephalic AVF, which was lost to thrombosis of the access. Following which he required a tunnelled dialysis catheter as a bridge to dialysis till the right-sided AVF matured. Unfortunately, after only a few months, he developed a very tight subclavian stenosis [Figure 1], which was not amenable to endovascular treatment. A veno-venous Goretex graft was surgically placed to connect the cephalic to the internal jugular vein. The patient developed stenoses at both ends of the graft, which were successfully treated with PTA [Figures 2–4]. The patient continues to receive hemodialysis using the same vascular access and undergoes surveillance fistulagrams every 3-4 months. We recommend that patients who have had surgery, to bypass vascular stenosis, must be under surveillance to diagnose new stenotic lesions, which in turn can be successfully treated using endovascular techniques. In this patient, the longevity of the right-sided AVF was considerably extended by using a veno-venous graft and subsequently by PTA.
Some patients will require a multidisciplinary approach and strategy to increase the longevity of their vascular access to maintain them on hemodialysis.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Dialysis access fistulas: Treatment of stenoses by transluminal angioplasty. Radiology. 1984;152:637-42.
- [Google Scholar]
- Central venous stenosis in hemodialysis patients is a common complication of ipsilateral central vein catheterization. J Am Soc Nephrol. 2004;15:368A-9A.
- [Google Scholar]
- Subclavian vein thrombosis: A frequent complication of subclavian vein cannulation for hemodialysis. Clin Nephrol. 1986;26:235-8.
- [Google Scholar]
- Subclavian stenosis: A major complication of subclavian dialysis catheters. Nephrol Dial Transplant. 1988;3:423-5.
- [Google Scholar]
- Superiority of the internal jugular over the subclavian access for temporary dialysis. Nephron. 1990;54:154-61.
- [Google Scholar]
- Post catheterisation vein stenosis in haemodialysis: Comparative angiographic study of 50 subclavian and 50 internal jugular accesses. Nephrol Dial Transplant. 1991;6:722-4.
- [Google Scholar]
- Incidence of central vein stenosis and occlusion following upper extremity PICC and port placement. Cardiovasc Intervent Radiol. 2003;26:123-7.
- [Google Scholar]
- Subclavian vein stenosis, permanent cardiac pacemakers and the haemodialysed patient. Nephron. 1991;58:103-5.
- [Google Scholar]
- Unilateral breast enlargement secondary to hemodilaysis arterivenous fistula and subclavian vein occlusion. Nephron. 1993;63:351-3.
- [Google Scholar]
- Pleural effusion associated with ipsilateral breast and arm edema as a complication of subclavian vein catheterization and arteriovenous fistula formation for hemodialysis. Chest. 1994;106:950-2.
- [Google Scholar]
- Importance of Doppler analysis of transmitted atrial waveforms prior to placement of central venous access catheters. J Vasc Interv Radiol. 1998;9:927-34.
- [Google Scholar]
- Central venous stenosis in the hemodialysis patient: Incidence and efficacy of endovascular treatment. Cardiovasc Surg. 1997;5:504-9.
- [Google Scholar]
- NKF-K/DOQUI clinical practice guidelines for vascular access: Update 2000. Am J Kidney Dis. 2001;37:S137-81.
- [Google Scholar]
- Long-term outcomes of primary angioplasty and primary stenting of central venous stenosis in hemodialysis patients. J Vasc Surg. 2007;45:776-83.
- [Google Scholar]
- Venous stenoses in dialysis shunts: Treatment with self-expanding metallic stents. Radiology. 1989;170:401-5.
- [Google Scholar]
- United States Renal Data System USRD 2003 Annual Data Report: Atlas of End-Stage Renal Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2003.
- Society of Interventional Radiology Standards of Practice Committee. Quality improvement guidelines for percutaneous management of the thrombosed or dysfunctional dialysis access. J Vasc Interv Radiol. 2003;14:S247-53.
- [Google Scholar]
- Use of stent grafts to repair hemodialysis graft-related pseudoaneurysms. J Vasc Interv Radiol. 2005;16:1301-7.
- [Google Scholar]
- The use of covered nitinol stents to salvage dialysis grafts after multiple failures. Vasc Endovascular Surg. 2006;40:275-9.
- [Google Scholar]
- Utility of covered stents for revision of aging failing synthetic hemodialysis grafts: A report of three cases. Cardiovasc Intervent Radiol. 2003;26:550-3.
- [Google Scholar]
- An occult cause of arteriovenous access failure: Central vein stenosis from permanent pacemaker wire. Report of three cases and review of the literature. Am J Nephrol. 2001;21:406-9.
- [Google Scholar]
- Prevalence of central venous occlusion in patients with chronic defibrillator leads. Am Heart J. 2001;141:813-6.
- [Google Scholar]
- Nephrogenic systemic fibrosis: Suspected causative role of gadodiamide used for contrast-enhanced magnetic resonance imaging. J Am Soc Nephrol. 2006;17:2359-62.
- [Google Scholar]
- Subclavian vein repair in patients with an ipsilateral arteriovenous fistula. Ann Vasc Surg. 1994;8:549-56.
- [Google Scholar]
- Surgical bypass for subclavian vein occlusion in hemodialysis patients. J Am Coll Surg. 2002;194:416-21.
- [Google Scholar]







