Translate this page into:
Factor V Leiden Heterozygous Mutation and Hyperhomocysteinemia Presenting with Vascular Rejection and Renal Allograft Infarction
Corresponding author: Raj Kanwar Yadav, Department of Nephrology, All India Institute of Medical Sciences, Ansari Nagar, New Delhi, India. E-mail: Rkyadavnephrology@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Pahuja T, Sangha SS, Sarkar A, Yadav RK. Factor V Leiden Heterozygous Mutation and Hyperhomocysteinemia Presenting with Vascular Rejection and Renal Allograft Infarction. Indian J Nephrol. 2025;35:117-8. doi: 10.25259/IJN_330_2024
Dear Editor,
A 40-year-old male was diagnosed with end-stage kidney disease in 2020. He developed lower limb edema following femoral catheterization which resolved spontaneously. He underwent a kidney transplant in 2022. In October 2023, he presented with macroscopic hematuria and graft dysfunction. Graft biopsy revealed acute T-cell-mediated rejection (TCMR).
He was treated with methylprednisolone pulse and rabbit anti-thymocyte globulin. After initial response, his creatinine started increasing again. Graft biopsy revealed acute cortical necrosis with residual inflammation of TCMR. Doppler graft kidney and MRI revealed multiple cortical wedge-shaped infarcts [Figure 1].
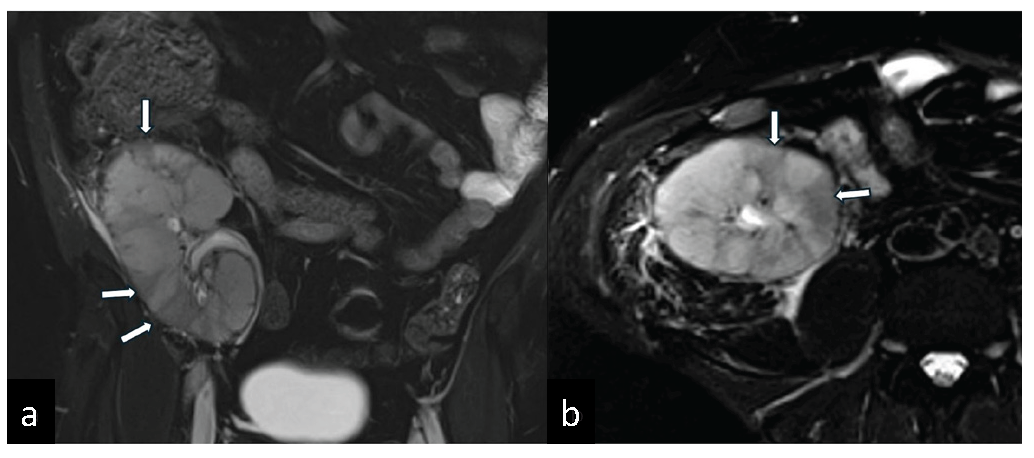
- A T2 weighted MRI images of the transplant kidney. (a) Coronal and (b) axial images shows multifocal, wedge-shaped areas of T2 hypointensities (white arrows) suggestive of cortical infarcts.
Workup was negative for ANA and APLA, and complement levels were normal. Thrombophilia workup revealed hyperhomocsyteinemia 31.3 (1–5) micromol/L and factor V Leiden heterozygous mutation. There were no mutations in prothrombin gene (PGM) and MTHFR gene. Protein C and Protein S levels were normal. He was managed with oral Apixaban and folate. He stopped anticoagulation after a month and presented with recurrent DVT right lower limb and pulmonary thromboembolism.
Several studies have described FVL mutation and increased risk of transplant RVT. FVL mutation leads to fourfold rise in allograft thrombosis.1 FVL mutation also predisposes to acute vascular rejection.2,3 Possible mechanism involves delayed inactivation of FVL leading to microthrombi formation in ischemic graft endothelium. There is a link between hypercoagulable state induced by FVL mutation and immunological injury to graft vasculature.
In our patient, thrombophilia profile led to vascular rejection and ACN. Any patient with history of DVT/PTE should be properly screened before transplant as thrombophilia can lead to RVT, microvascular thrombosis, and precipitate rejection. This can be prevented by pretransplant screening for FVL in high-risk patients and perioperative and posttransplant anticoagulation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
References
- The factor V Leiden (R506Q) mutation and risk of thrombosis in renal transplant recipients. Transplantation. 1997;64:604-7.
- [CrossRef] [PubMed] [Google Scholar]
- High rate of acute rejections in renal allograft recipients with thrombophilic risk factors. J Am Soc Nephrol. 1998;9:1309-13.
- [CrossRef] [PubMed] [Google Scholar]
- Factor V R506Q mutation (activated protein C resistance) is an additional risk factor for early renal graft loss associated with acute vascular rejection. Transplantation. 2000;69:1577-81.
- [CrossRef] [PubMed] [Google Scholar]







