Translate this page into:
Filariasis-Associated Secondary Membranous Nephropathy: A Rare Presentation
Corresponding author: Rohit Badge, Department of Nephrology, AIIMS Raipur, Chhattisgarh, India. E-mail: rohitbadge29@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Badge R, Rathore V, Aggarwal J. Filariasis-Associated Secondary Membranous Nephropathy: A Rare Presentation. Indian J Nephrol. 2024;34:385-7. doi: 10.25259/ijn_363_23
Abstract
Parasitic infections like filariasis are uncommon causes of secondary membranous nephropathy (MN) which requires serological tests to detect circulating Wuchereria bancrofti antigens for its diagnosis or the identification of microfilariae in the capillary lumen on kidney biopsy. The immunochromatographic card tests is simple, non invasive and has high sensitivity and specificity. We report a case of 30 year old lady who presented to us with nephrotic syndrome which on kidney biopsy showed features of membranous nephropathy with negative staining for Anti PLA2R, THSD7A and exostosin. A thorough workup was done to find out any secondary cause of MN where she was found positive with filiarial antibody test. Hence, a diagnosis of secondary membranous pattern nephropathy was considered for which she was treated with diethylcarbamazine (DEC) and other supportive medications which on follow up showed marked resolution of proteinuria.
Keywords
Secondary membranous nephropathy
Nephrotic syndrome
Filariasis
Introduction
Filariasis is a major health problem in the developing parts of the world such as Africa, Southeast Asia, and South America. India contributes to approximately 40% of the total global clinical burden. The disease is predominantly caused by the parasites Wuchereria bancrofti and Brugia malayi, which get transmitted through mosquito bite. The most common clinical features due to lymphatic obstruction are chyluria, hydrocoele, lymphedema, and elephantiasis.1,2 The histopathological lesions on kidney biopsy in filariasis are membran oproliferative (MPGN) and mesangioproliferative glomerulonephritis, and membranous pattern nephropathy (MN) is seen rarely.3 We present a case of a 30-year-old lady with nephrotic syndrome, which on kidney biopsy showed features of MN. She was found positive for filiarial antibody was treated with diethylcarbamazine (DEC) and showed marked resolution of proteinuria.
Case Report
A 30-year-old lady presented with facial puffiness and lower-limb swelling for 1 month. She had bilateral pitting pretibial edema, and her BP was 120/90 mm Hg; the rest of the examination was unremarkable. Laboratory tests showed Hb 14.3 g/dL, WBC 8240/mm3, platelets 2.43/mm3, eosinophil count 4.4%, blood urea 21 mg/dL, creatinine 0.65 mg/dL, uric acid 7.4 mg/dL, total protein 6.4 g/dL, serum albumin 2.6 g/dL, triglyceride 483 mg/dL, total cholesterol 235 mg/dL, blood sugars 112 mg/dL, and TSH 8.65 mIU/L. Serology for hepatitis B surface antigen, hepatitis C virus, and human immunodeficiency virus was negative. Serum C3 was 110 (79–152 mg/dL), and C4 was 28 (16–38 mg/dL). Urinalysis showed 3 + albumin, pus cells 1–2, RBC nil, no cast, and 24-h urinary protein was 17.2 g/24 h. Anti-nuclear antibodies (ANA) were negative. The patient underwent renal biopsy, which on light microscopy showed 15 glomeruli with diffuse thickening of capillaries with membrane texture alterations and intramembranous mottling. There was no evidence of tuft necrosis, segmental tuft sclerosis, thrombi, or crescents. IFTA was seen in <10% of the cortex. Arteries and arterioles were unremarkable [Figure 1]. Immunofluorescence study showed positive staining for IgG (2+), trace C1q, kappa (3+), lambda (3+) light chains, and negative staining for IgA, IgM, and C3. On Immunohistochemistry (IHC), staining for anti-PLA2R, exostosin, and thrombospondin (THSD7A) were negative. The patient was initiated treatment with angiotensin receptor blockers (ARBs), diuretics, statins, and other supportive therapy. Workup for secondary causes of MN was carried out. The patient did not give any past or family history of filariasis. A patient consent was obtained. She was not on any painkillers or alternate medicines. Papanicolaou (PAP) test smear to screen cervical cancer was negative, peripheral smear for malarial parasite was negative, ultrasound of whole abdomen and chest x-ray was normal, and tumor markers such as human chorionic gonadotropin (HCG), cancer antigen (CA-125), and alpha-fetoprotein (AFP) were negative. Rheumatoid factor (RA) and C-reactive proteins (CRP) were within normal range. However, filiarial antibody test for IgM and IgG by immuno dot was positive. On clinical suspicion and because the patient belongs to the state of Bihar, which is an endemic area for filariasis, the patient was treated with diethylcarbamazine (DEC) 6 mg/kg/day for 21 days, and lymphangioscintigraphy did not show any evidence of lymphatic obstruction. After treatment with DEC and other supportive therapy, her clinical symptoms and proteinuria started resolving. The trend of serum albumin, creatinine, and 24-h proteinuria is shown in Table 1. After 2 years of follow-up, she is asymptomatic, and her BP, renal functions, and proteinuria are within normal limits.
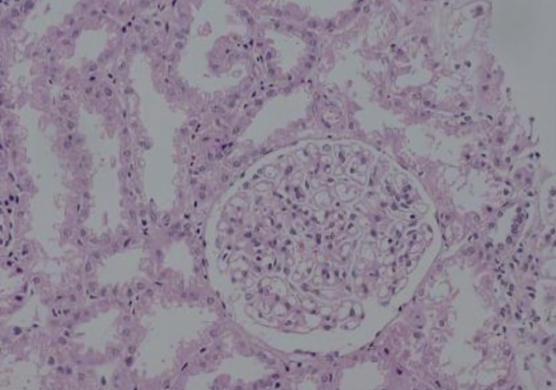
- Light microscopy showing diffuse thickening of capillaries with altered membrane texture (Periodic Acid-Schiff reaction × 400).
| 29/06/21 | 06/10/21 | 27/10/21 | 24/11/21 | 08/12/21 | 15/06/22 | 24/05/23 | |
|---|---|---|---|---|---|---|---|
| Creatinine (mg/dL) | 0.65 | 0.52 | 0.59 | 0.56 | 0.48 | 0.61 | 0.63 |
| S. albumin (g/dL) | 2.6 | 2.8 | 2.7 | 2.9 | 2.4 | 3.6 | 4.3 |
| 24-h urinary proteins (g/24 h) | 17.2 | 11 | 8 | 7.9 | 3.3 | 3 | 0.32 |
S.: Serum.
Discussion
Several studies have recently shown a clear association between filariasis and glomerular disease. Most of the studies and case reports describe MPGN or mesangioproliferative GN in filariasis. However, rarely, membranous pattern nephropathy has also been reported in the literature.2,3 In our case, on kidney biopsy, features were suggestive of membranous pattern nephropathy (MN) with negative staining for anti-PLA2R, THSD7A, and exostosin. After a thorough workup to see for any secondary cause, the patient was found positive with anti-filarial antibody test. Microfilariae can cause glomerular disease by direct physical invasion or as an immune-mediated disease. However, granulomatous inflammatory reaction associated with eosinophilia is also reported in the glomeruli and interstitium.4 One of the most common symptoms of filariasis is chyluria, which is the passage of intestinal lymph in urine. Our case has no chyluria, probably due to the absence of significant lymphatic obstruction, which was confirmed by lymphangioscintigraphy. The traditional method for diagnosis of filariasis is by detection of microfilaria in the peripheral smear. However, this method proved to be less sensitive. ELISA and a rapid format immunochromatographic card test detect circulating filarial antigens with high sensitivity and specificity.5
Conclusion
This case report shows the importance of considering parasitic infections in endemic areas as a rare cause of membranous nephropathy. Workup to look for secondary causes should include a search for viral, bacterial, and parasitic infections such as filariasis.
Conflicts of interest
There are no conflicts of interest.
References
- Filariasis, with chyluria and nephrotic range proteinuria. J Assoc Physicians India. 2013;61:487-9.
- [PubMed] [Google Scholar]
- Glomerulopathy associated with parasitic infections. Clin Microbiol Rev. 2000;13:55-66. table of contents
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Secondary membranous nephropathy. A narrative review. Front Med (Lausanne). 2020;7:611317.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Microfilariae-associated nephrotic range proteinuria. Kidney Int. 2011;79:1152.
- [CrossRef] [PubMed] [Google Scholar]
- Microfilaria Causing nephrotic syndrome: Highlighting the importance of diethylcarbamazine provocation test for diagnosis. J Family Med Prim Care. 2022;11:4002-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]








