Genetic Rarity: The First Case Report of TMPRSS3 Mutation Coinciding with Multicystic Dysplastic Kidney
Corresponding author: Nitish Kumar, Division of Pediatric Nephrology, Department of Pediatrics, Institute of Medical Sciences, Banaras Hindu University, Varanasi, U.P., India. E-mail: doctornitishkumar@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Abhinay A, Kumar N, Panda S, Singh A. Genetic Rarity: The First Case Report of TMPRSS3 Mutation Coinciding with Multicystic Dysplastic Kidney. Indian J Nephrol. doi: 10.25259/IJN_462_2024
Dear Editor,
A 9-month-old male born to a non-consanguineous marriage was admitted with complaints of fever, lethargy, and reduced urine output. There was a history of two infant deaths in the family. He had hypoglycemia and severe hypernatremic dehydration. Physical examination revealed signs of dehydration. Blood gas analysis and renal function revealed severe metabolic acidosis and hypernatremia, and urea and creatinine levels were 144 and 3.5 mg/dL, respectively. His clinical and laboratory parameters improved with supportive management, and the hemogram and peripheral blood smear findings were normal. Urinalysis demonstrated nephrotic range proteinuria and microscopic hematuria. A sonogram of the abdomen and kidney–ureter–urinary bladder demonstrated a multicystic dysplastic kidney (MCDK) on the left side. He had persistent hypertension, which was managed with enalapril. Ocular and auditory evaluation did not reveal any abnormality. Genetic analysis was performed to look for inborn error of metabolism. It revealed a heterozygous variant (c.413C>A, p.Ala138Glu) in the TMPRSS3 gene, pathogenic as per the American College of Medical Genetics and Genomics, and confirmed with Sanger sequencing [Figure 1, Supplementary Files]. Genetic counseling and surgical options were explained to the parents. Screening of the family members was normal.
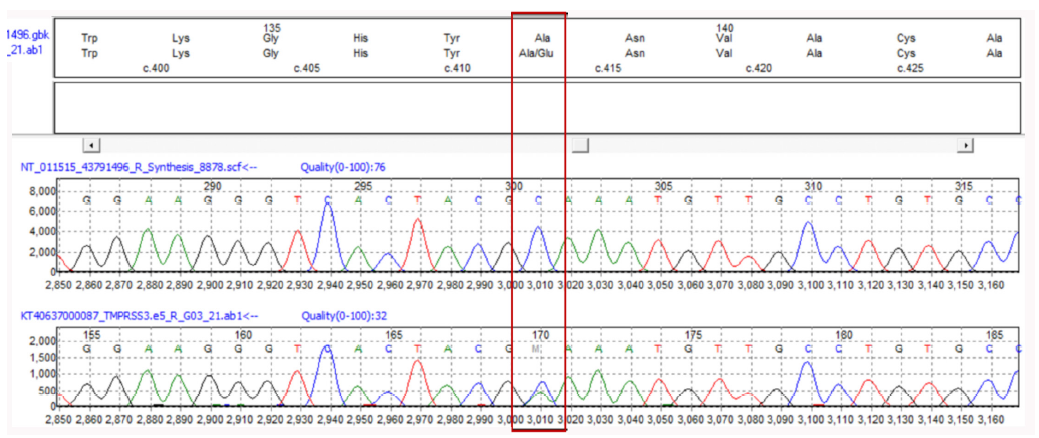
- Sanger sequencing data (electropherogram) for the provided sample showing nucleotide change at chr21: c.413C>A,, (p.Ala138Glu) in TMPRSS3 gene. Red, green, black, and blue colored peaks show thymine, adenine, guanine, and cytosine bases, respectively. The red rectangle in the image highlights a specific nucleotide change in DNA sequencing data (electropherogram).
Mutations in TMPRSS3 are usually associated with autosomal recessive deafness in infants in heterozygous state.1 TMPRSS3 mutations have been reported to express themselves with nonsyndromic hearing loss previously in the heterozygous state.2 Though the expression of TMPRSS3 in the human kidneys has been less studied, this mutation has also been seen to play a role in pseudo-hypoaldosteronism type 1 and Liddle syndrome.3 A splice variant of TMPRSS3, TMPRSS3f, has also been found in the kidneys of mice, which share 89% identity with the human TMPRSS3f.4 So, it is likely that a mutation in TMPRSS3 might produce structural renal anomalies along with deafness.
Acknowledgement
We thank all the residents and staff who were involved in the care of this patient.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
References
- Non-surgical management of multicystic dysplastic kidney. BJU Int. 2008;101:804-8.
- [CrossRef] [PubMed] [Google Scholar]
- Role of transcription factor hepatocyte nuclear factor-1β in polycystic kidney disease. Cell Signal. 2020;71:109568.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cytogenomic aberrations in isolated multicystic dysplastic kidney in children. Pediatr Res. 2022;91:659-64.
- [CrossRef] [PubMed] [Google Scholar]
- Insertion of beta-satellite repeats identifies a transmembrane protease causing both congenital and childhood onset autosomal recessive deafness. Nat Genet. 2001;27:59-63.
- [CrossRef] [PubMed] [Google Scholar]







