Head Drop and Flaccid Weakness in Infantile Nephrotic Syndrome
Address for correspondence: Dr. G. S. Dhooria, Department of Pediatrics, Dayanand Medical College and Hospital, Ludhiana, Punjab, India. E-mail: gurdeep2005123@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Dropped head syndrome (DHS) is a relatively rare condition, with a broad differential diagnosis. We report here a case of infantile nephrotic syndrome with DHS caused by severe hypokalemia. Electrocardiogram showed flat T- and U-waves. Multiple factors including recurrent diarrhea, prolonged diuretic and corticosteroid use, hypomagnesemia, poor intake, and malnutrition caused hypokalemia in the case. Head drop and flaccid weakness resolved completely after potassium and magnesium supplementation. Potassium levels should be monitored and corrected promptly in these settings.
Keywords
Hypokalemia
nephrotic syndrome
paralysis
Introduction
Dropped head syndrome (DHS) is characterized by severe weakness of the cervical paraspinal muscles, most commonly associated with neuromuscular disorders.[1] Although hypokalemia has been listed as a cause of DHS,[2] very few cases of hypokalemic weakness have been reported in children with nephrotic syndrome. Here, we report a case of infantile nephrotic syndrome who presented with sudden onset head drop and flaccid weakness due to hypokalemia. In this case, recurrent diarrhea, prolonged diuretic and corticosteroid use, poor intake, and malnutrition causing hypokalemia have been explained. The condition was rapidly reversed by potassium and magnesium supplementation.
Case Report
An 18-month-old male infant, diagnosed as a case of steroid-resistant nephrotic syndrome, born of nonconsanguineous marriage, was admitted with complaints of not able to sit and head drop for 1 day.
The patient was diagnosed to be a case of infantile nephrotic syndrome at the age of 1 year with puffiness of face, edema feet, and oliguria. There was no renal dysfunction, hematuria, or hypertension. Family history of kidney disease was absent. He was treated with full dose steroid (2 mg/kg/day) for 4 weeks and additional 2 weeks with no remission. Renal biopsy showed minimal change disease with no deposits on immunofluorescence. He was started with cyclosporine A (6 mg/kg/day), alternate day steroids (1.5 mg/kg/day), oral enalapril and furosemide. Trough cyclosporine (C0) blood level after 4 weeks of initiation was 95 (target: 80–120 ng/ml). In the subsequent months, the patient was admitted twice, 5–7 days each with an interval of 2 weeks for infective diarrhea and treated with antibiotics, zinc, and fluid management. Diuretics were intentionally withheld and not restarted. Serum electrolytes at the time of last discharge were normal. The infant intake reduced to predominantly milk, due to cough, cold, and wheezing, few days before the weakness developed. There was no history of fever, dysuria, or vomiting. There was no history of weakness in the past. There was weight loss of 800 g (10% body weight) from previous hospital visit.
On admission, the infant was limp but conscious. General examination showed mild pallor and minimal pedal edema. Weight of the child was 7.4 kg (expected 10.5 kg, <3rd percentile WHO standards, Grade II malnutrition of Indian Academy of Pediatrics classification). Urine output was normal with approximately 1 ml/kg/h. Vital parameters were normal. Neurologically, the infant was conscious, but irritable. There was no cranial nerve palsy. There was head drop with weakness of extensors of neck. Tone was decreased in all the four limbs. He was able to sit only with support in tripod position [Figure 1]. Deep tendon reflexes were depressed and planters were absent. Other systemic examinations were normal.

- Head drop in the infant completely recovered after potassium supplementation. (a) Before correction. (b) After correction
Suspecting hypokalemic paralysis, electrocardiogram (ECG) was done which showed flat T- and U-waves [Figure 2]. Investigations revealed hypokalemia (serum K+ = 2.1 mEq/L), hypocalcemia (corrected serum Ca = 6.9 mg/dl), hypomagnesemia (serum Mg = 1.6 mg/dl), hypoalbuminemia (serum albumin = 2.0 g/dl), and hypercholesteremia (serum cholesterol = 216 mg/dl) with blood urea of 3 mg/dl and serum creatinine of 0.12 mg/dl. Random blood sugar was 106 mg/dl and complete blood count was normal. Thyroid profile was normal.
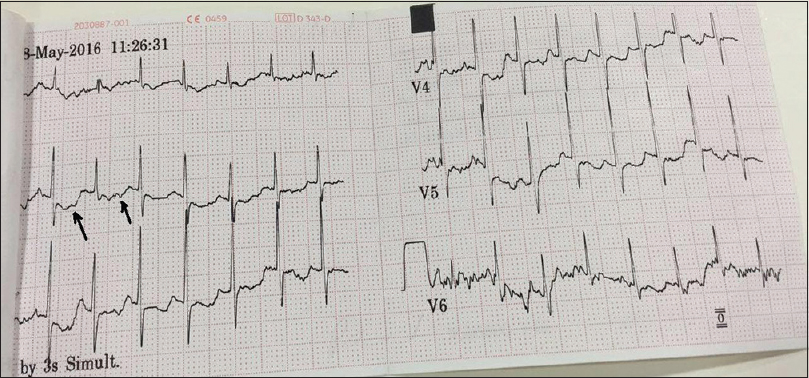
- Electrocardiogram showing flat T- and U-waves (arrows) in the infant with hypokalemia
Arterial blood gas analysis was normal (pH = 7.40, HCO3− = 22.3 mmol/L, PCO2 = 36 mmHg, PO2 = 83.3 mmHg, and SaO2 = 95%) and urinary electrolytes (mEq/L) were Na: 9, K: 2.2, Cl: 12, creatinine: 5. Urinary K was <20 mEq/L with FeK of 2.5% (average 10%). Transtubular potassium gradient (TTKG) calculated was 0.5 (<4) ([urinary K × serum osmolality/serum K × urinary osmolarity] ×100), suggesting extrarenal losses. Spot urine protein creatinine ratio was 0.34 (normal <0.2). Spot calcium creatinine ratio was 0.34 (normal <0.8 for infants) and FeNa was 0.34 (normal <2). Urine routine and microscopy showed trace proteins and no white blood cells or red blood cells. Serum 25-hydroxyvitamin D3 level was 3 (normal = 9–37.6 ng/ml).
The patient was started on KCl infusion (4 mEq KCl in 100 ml fluid) along with injection MgSO4 50% 0.2 ml/kg intramuscular for 2 days; head drop improved rapidly and the patient completely recovered within 48 h. Repeat serum K+ level was normal (3.7 mEq/L). The patient was discharged on oral potassium supplement (syrup Potclor 20 mEq/15 ml) of 1 mEq/kg.
Discussion
Hypokalemic paralysis is defined as an acute-onset flaccid paralysis associated with low plasma potassium (<3.5 mEq/L).[3] The most common causes of hypokalemia are gastrointestinal loss (diarrhea, laxatives), renal loss (hyperaldosteronism, severe hyperglycemia, potassium-depleting diuretics, carbenicillin, sodium penicillin, and amphotericin B), intracellular shift (alkalosis), and malnutrition.[3] In the presence of hypokalemia, low urinary potassium <20 mmol/day suggests extrarenal loss or could be due to malnutrition (decreased oral intake), whereas urinary potassium >20 mmol/day suggests renal loss.[4] In the index case, urinary potassium and TTKG were low with no acidosis or alkalosis, ruling out renal losses such as renal tubular acidosis, Bartter syndrome, or primary hyperaldosteronism.
The major consequences of severe hypokalemia result from its effects on nerves and muscles (including the heart). Symptoms of mild hypokalemia are weakness, fatigue, paralysis, respiratory difficulty, constipation, paralytic ileus, and leg cramps; more severe hypokalemia will alter cardiac tissue excitability and conduction. Hypokalemia can produce ECG changes such as U-waves, T-wave flattening, and arrhythmias, particularly ventricular arrhythmias.[3] This infant had flat T- and U-waves on ECG, and head drop and flaccid weakness. The cause of hypokalemia was multifactorial as the patient had repeated episodes of diarrhea, poor intake/malnutrition, and was on medications such as loop diuretics and corticosteroids. The infant had a viral-induced wheeze, the possible use of oral salbutamol caused shift of potassium to precipitate the weakness in an already depleted infant.
Typically, furosemide-induced hypokalemia is characterized by metabolic alkalosis, hypocalcemia, hypomagnesemia, high urine calcium creatinine ratio, and high urine sodium excretion, also termed “Pseudo–Bartter syndrome.”[5] Loop and thiazide diuretics deplete not only potassium but also magnesium. Oral potassium supplementation and/or potassium-sparing diuretics are used to recover from these losses.[6] Magnesium deficiency was also found in this case which could be explained with malnutrition, diuretic, and cyclosporine use. Renal allograft recipients receiving cyclosporine showed a significant reduction in serum magnesium levels and increased fractional excretion of magnesium, suggesting renal wasting.[7] Glucocorticoids, used in this patient for nephrotic syndrome, also cause renal sodium retention and potassium excretion with no increase in hydrogen excretion.[8]
Under normal circumstances, only minimal amounts of potassium are excreted through the intestine. In severe diarrhea, 90 mmol/24 h (<4 g of potassium) can be lost in stools, and in infants suffering from protein–energy malnutrition, potassium deficiency occurs when 10%–30% of body potassium is lost.[9] Repeated episodes of diarrhea, past diuretic use, and malnutrition might have caused chronic depletion of potassium stores.
Potassium content of human milk is 15 mmol/L. Cow's milk contains 38 mmol/L of potassium and commercial formulae have around 18 mmol/L. The recommended adult potassium intake is 1875–5625 mg daily (10–28 g of KCl), while in infants <6 months, it is 350–925 mg (1.8 g of KCl) and in >6 months, it is 475–1275 (2.5 g of KCl). In children from 1 to 3 years, the recommended potassium intake is 550–1650 mg (3.2 g of KCl), and in 4–6 years, it is 775–2325 mg (4.5 g of KCl).[9] Our patient took only about 400 ml/day cow's milk (approximately 14 mmol/L) which was insufficient for his needs.
To our knowledge, only two cases of hypokalemia paralysis with nephrotic syndrome have been reported in literature till date, one had unusual combination of distal renal tubular acidosis with membranous nephropathy coupled with hypokalemic paralysis and medullary nephrocalcinosis.[410]
Our case was an infant with steroid-resistant nephrotic syndrome who developed hypokalemic paralysis in the form of head drop and flaccid weakness secondary to multiple factors. The case highlights the need to monitor potassium levels with prolonged use of diuretics and steroids. Potassium deficiency should be anticipated, especially in cases with recurrent diarrhea and malnutrition.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We acknowledge Professor Daljit Singh for his constant guidance and support.
References
- Dropped head syndrome: Etiology and management. J Am Acad Orthop Surg. 2012;20:766-74.
- [Google Scholar]
- Dropped head syndrome: Diagnosis and management. Evid Based Spine Care J. 2011;2:41-7.
- [Google Scholar]
- Etiological spectrum of hypokalemic paralysis: A retrospective analysis of 29 patients. Ann Indian Acad Neurol. 2013;16:365-70.
- [Google Scholar]
- A rare case of type I renal tubular acidosis with membranous nephropathy presenting as hypokalemic paralysis. Case Rep Nephrol Urol. 2013;3:91-8.
- [Google Scholar]
- Furosemide-induced severe hypokalemia with rhabdomyolysis without cardiac arrest. BMC Womens Health. 2013;13:30.
- [Google Scholar]
- Clinical use of diuretics in heart failure, cirrhosis, and nephrotic syndrome. Int J Nephrol. 2015;2015:975934.
- [Google Scholar]
- Hypomagnesemia and renal magnesium wasting in renal transplant recipients receiving cyclosporine. Am J Med. 1987;83:693-9.
- [Google Scholar]
- Physiologic and pharmacologic effects of corticosteroids. In: Kufe DW, Pollock RE, Weichselbaum RR, Bast RC, Gansler TS, Holland JF, eds. Holland-Frei Cancer Medicine (6th ed). Hamilton, ON: BC Decker; 2003.
- [Google Scholar]
- Indian Council of Medical Research. Jamai-Osmania, Hyderabad: National Institute of Nutrition; Nutrient Requirements and Recommended Dietary Allowances for Indians; A Report of the Expert Group of the Indian Council of Medical Research 2009-2010; 2009-2010.
- Nephrotic syndrome and hypokalemic paralysis. J Assoc Physicians India. 1998;46:401.
- [Google Scholar]







