Translate this page into:
High Neutrophil-to-Lymphocyte Ratio as a Predictor of All-Cause and Cardiovascular-Related Mortality in Hemodialysis Patients: A Systematic Review and Meta-Analysis of Cohort Studies
Corresponding author: Agnestia Selviani Tanic, Department of Internal Medicine, Karel Sadsuitubun Hospital, Maluku, Indonesia. E-mail: agnestiaselviani05@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Tanic AS, Rinaldi FX, Polanit VL, Kalaij AGI. High Neutrophil-to-Lymphocyte Ratio as a Predictor of All-cause and Cardiovascular-Related Mortality in Hemodialysis Patients: A Systematic Review and Meta-Analysis of Cohort Studies. Indian J Nephrol. doi: 10.25259/IJN_470_2024
Abstract
Background
Chronic kidney disease (CKD) remains a major cause of mortality. Recent studies have demonstrated a correlation between the neutrophil-to-lymphocyte Ratio (NLR), which is an inflammatory biomarker, and various chronic diseases. This study aims to assess high NLR as a prognostic indicator for all-cause and cardiovascular (CV)-related mortality in patients with CKD undergoing hemodialysis (HD).
Materials and Methods
This systematic review (SR) and meta-analysis (MA) were done based on preferred reporting items for systematic reviews and meta-analyses statements 2020. The literature review identified 555 studies up to August 2023 from PubMed, EBSCOHost, ProQuest, Cochrane, and Google Scholar databases using predetermined keywords. Newcastle-Ottawa Scale (NOS) was used to assess the bias of these studies. Data were extracted and MA was done using RevMan.
Results
Nine and six relevant studies were included for SR and MA, respectively. According to NOS risk of bias, all studies showed overall good quality. HD patients with high NLR had a significantly increased risk of all-cause mortality (3.83 times higher) than those with low NLR (95% CI: 1.85-7.93; p=0.0003; I2=83%). Similarly, HD patients with high NLR had an increased risk of CV-related mortality (1.19 times) than those with low NLR, though not significant (95%CI: 0.82-1.72; p=0.37; I2=60%).
Conclusion
This study shows a correlation between high NLR values and increased risk of all-cause and CV-related mortality in CKD patients undergoing HD (higher ratio than low NLR values).
Keywords
Neutrophil-to-lymphocyte ratio
Mortality
Hemodialysis
Introduction
Chronic kidney disease (CKD) has emerged as one of the most prominent causes of death and suffering in the 21st century. Although mortality has declined in patients with end-stage kidney disease (ESKD), the Global Burden of Disease (GBD) studies have shown CKD to be a leading cause of worldwide mortality.1,2 Several reports suggest a wide variation in CKD prevalence across the region (4.7%–17.4%).3-6 Untreated, CKD can worsen and lead to kidney failure requiring dialysis or transplantation. According to the United States Renal Data System 2020 Annual Data Report, nearly 808,000 people in the United States are either on dialysis (69%) or with kidney transplants (31%) due to ESKD.7,8 CKD causes fatigue, fluid retention, and sleep disturbances. Patients undergoing dialysis have restricted diets and cannot travel, and this, along with financial and spiritual challenges, significantly impacts their quality of life.9
HD improves survival in CKD by lowering the inflammatory response and the risk of comorbidities, resulting in a better prognosis. Even with significant technical advancements, the mortality rate remains 10 to 30 times higher than that of the general population.10 This elevated mortality is partly attributable to the prevalence of comorbidities, including cardiovascular (CV) disease, diabetes, and advanced age.7 Investigating inflammatory biomarkers in patients undergoing HD will help evaluate disease progression and prognosis.
Neutrophil-to-lymphocyte (NLR) is a simple biomarker that can describe a functional relationship between neutrophils and lymphocytes.11 Neutrophils and lymphocytes provide an overview of the innate and adaptive immune systems, respectively. Hence, NLR represents systemic infection.12-14 Higher NLR values are associated with greater inflammation and worse prognosis in chronic diseases.15,16 Theoretically, HD may inhibit the inflammatory process. Comorbid conditions and the aging process can decrease inflammation in clinically insignificant amounts. Therefore, assessing NLR as an inflammatory biomarker in HD patients may be valuable for predicting disease progression and mortality outcomes.
Unfortunately, there are currently no systematic studies and meta-analyses regarding this. It is reasonable to hypothesize that elevated NLR values could be linked to the prognosis of CKD patients undergoing HD. This study aims to fill this gap by conducting an MA of relevant cohort studies to evaluate the association between elevated NLR and mortality outcomes in CKD patients on HD.
Materials and Methods
This SR was carried out according to a predetermined methodology and submitted under the identification number CRD42024569293 in the International Prospective Register of Systematic Reviews (PROSPERO). The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement’s recommendations were followed in the production of this review. Since, this is systematic review and meta-analysis study, it only needs to be registered in PROSPERO, and does not require any ethical approval or patient consent.
The following electronic databases, Pubmed, EBSCOHost, ProQuest, and Cochrane, were searched for indexed studies from inception to August 24, 2023. The following keywords, their synonyms, and subject headings were used to strategize the search: “the neutrophil to lymphocyte ratio’ OR ‘the ratio of neutrophil to lymphocyte’ OR ‘NLR’ or ‘neutrophil/lymphocyte ratio’, and ‘end-stage renal disease’, or ‘hemodialysis’ or ‘hemodialysis on chronic kidney disease,” [Supplementary Table 1]. We also manually screened references and citation list of the studies to find additional ones that could have been missed. Unpublished articles were screened from Google Scholar.
This review includes only cohort studies of CKD in adult patients (≥18 years) on HD. Studies with high NLR as their intervention (thresholds were defined as high and low according to included studies), low NLR as their comparison, and mortality rate (all-cause and CV-related) as their outcome were also allowed. Studies including patients with ESRD on peritoneal dialysis or intermittent HD were excluded. Studies having subjects with a prior history of fever and infections at baseline measurement time were excluded to minimize the confounding factors affecting NLR value. Studies other than English and Bahasa were also excluded.
All-cause and CV-related mortality rates in patients with CKD on HD were assessed as primary and secondary efficacy outcomes, respectively.
Studies were compiled in Endnote 20, which automatically removed duplicates. Two reviewers independently selected studies, extracted data, and assessed the risk of bias, and a third would resolve any discrepancies. The full-text reports were sought if the title and abstract of articles were deemed eligible on screening. These reports were then re-screened for eligibility. Abstract-only publications in conference proceedings were included.
Using a standardized extraction form, the following key information was gathered: author (year) as study identifier; high and low NLR cut-off for all-cause and CV-cause mortality in HD patients; baseline characteristics of participants such as number of subjects and age; and outcome as described above.
The modified NOS version, with a maximum of nine points, was used to assess studies for their risk of bias. The tool evaluated selection, comparability, and outcome for bias. The overall risk of bias was determined, considering the results in each domain using agency for healthcare research and quality (AHRQ) standard. Disagreements between the three reviewers were resolved through discussion with a fourth reviewer.
Data synthesis and statistical analysis
Meta-analysis was done using the Review Manager 5.4.1 provided by the Cochrane Collaboration Network. The outcomes were analyzed as dichotomous variables and pooled by risk ratio (RR) with 95% confidence interval (CI). The inverse variance random-effect model was used, accounting for the heterogeneity in the studies. The I2 statistics and the Cochran Q’s test were used to assess the statistical between-study heterogeneity. A P<0.05 and I2>50% are indicative of statistically significant heterogeneity. The value of I2<50% indicated a lack of heterogeneity in this study, and a fixed-effects model was used. According to potential heterogeneity variables, subgroup analysis was done to eliminate heterogeneity. If statistical heterogeneity persisted, a random effect model was carried out. Statistical significance was considered for p-values <0.05.
Results
The initial search yielded 555 studies: 316 from PubMed, 123 from EBSCOhost, 92 from ProQuest, 17 from Cochrane, and 7 from Google Scholar. Duplicates were removed, and titles and abstracts were screened, giving 29 studies that were screened based on full-text articles. Moreover, 20 studies were excluded on the basis of the inclusion and exclusion criteria: 11 studies lacked sufficient data, 7 involved non-HD patients, and 2 studies included only patients with a history of prior infection. Nine and six studies were included for SR and MA, respectively17-25 [Supplementary Figure 1].
Description of included studies
This meta-analysis yielded six studies assessing NLR as a predictor of mortality in patients undergoing HD. The studies were from several countries (America, Turkey, Poland, China, and Romania) and were published in the years 2016 (1 study), 2019 (2 studies), 2022 (1 study), and 2023 (2 studies). In addition, study outcomes were followed up from 1 to 60 months. Patients >17 years old with CKD, and on regular HD were included in this study. Studies that had patients with infection were excluded. Detailed characteristics and a qualitative summary of the included studies is illustrated in Table 1.
| Author | Year | Study design | Subject | Mean follow-up duration (months) | Minimum duration of HD at baseline | NLR value cut-off | ||
|---|---|---|---|---|---|---|---|---|
| Sample size | Mean age (years) | Low NLR | High NLR | |||||
| Neuen et al.17 | 2016 | Cohort | 207 | 54 ± 11 | 37 | NM | < 3.3 | ≥ 3.3 |
| Yaprak et al.18 | 2016 | Cohort | 80 | 56.8 ± 18.1 | 24 | 3 months | < 2.5 | ≥ 2.52 |
| Li H et al.19 | 2017 | Cohort | 268 | 48.7 ± 10.9 | 36 | 3 months | < 3.5 | ≥ 3.5 |
| Woziwodzka et al.20 | 2019 | Cohort | 84 | 61.5 | 60 | NM | < 3.9 | ≥ 3.9 |
| Diaz-Martinez et al.21 | 2019 | Cohort | 77 | 63.2 ± 15.7 | 12 | 3 months | ≤ 1.75 | >1.75 |
| Balboul et al.22 | 2020 | Cohort | 554 | 67.6 ± 14.2 | 14 | 2 months | NM | |
| Lano et al.23 | 2022 | Cohort | 183 | 65.5 ± 16.3 | 10 | 3 months | < 3.49 | ≥ 3.49 |
| Mureșan et al.24 | 2022 | Cohort | 461 | 64.36 ± 12.14 | 1 | 6 months | < 8.19 | ≥ 8.19 |
| Wang J et al.25 | 2023 | Cohort | 240 | 63.7 ± 13.85 | 58 | 6 months | < 4 | ≥ 4 |
NLR: Neutrophil-to-lymphocyte ratio, NM: Not mentioned, HD: Hemodialysis.
Publication bias
Each study included for systematic review and meta-analysis was assessed for quality using the NOS tool. Of nine studies, six achieved eight points, and three achieved seven out of a nine point maximum score. For selection, only one study achieved the full score, and the remaining studies achieved three points out of four. For comparability, three studies got only one star due to unclear blood sampling time. For outcomes, one study did not score full points due to the short follow-up duration. Overall, nine studies showed good quality based on AHRQ standards [Table 2].
| Author | Selection | Comparability of cohort on the basis of the design or analysis | Outcome | Score | AHRQ Standard | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Representativeness of the exposed cohort | Selection of the non-exposed cohort | Ascertainment of exposure | Demonstration that outcome of interest was not present at start of study | Assessment of outcome | Was follow-up long enough for outcomes to occur | Adequacy of follow up of cohorts | ||||
| Neuen et al. 201617 | - | * | * | * | ** | * | * | * | 8 | Good quality |
| Yaprak et al. 201618 | - | * | * | * | ** | * | * | * | 8 | Good quality |
| Li H et al. 201719 | - | * | * | * | ** | * | * | * | 8 | Good quality |
| Woziwodzka et al. 201920 | * | * | * | * | * | * | * | 7 | Good quality | |
| Diaz-Martinez et al. 201921 | - | * | * | * | * | * | * | * | 7 | Good quality |
| Balboul et al. 202022 | - | * | * | * | ** | * | * | * | 8 | Good quality |
| Lano et al. 202223 | - | * | * | * | ** | * | * | * | 8 | Good quality |
| Mureșan et al. 202224 | - | * | * | * | ** | * | - | * | 7 | Good quality |
| Wang J et al. 202325 | * | * | * | * | * | * | * | * | 8 | Good quality |
AHRQ: Agency for healthcare research and quality. *: indicates one point, **: indicates two points
Systematic review outcomes
Most studies had a follow-up period >12 months, with the longest extending to five years. Only two studies had a follow-up duration <12 months. The cut-off values for high and low NLR varied among the studies, possibly due to differences in the timing of blood collection. Additionally, two studies excluded factors like malignancies, hematological disorders, connective tissue disorders, and other systemic inflammatory conditions that could potentially influence NLR values. All studies demonstrated a greater all-cause mortality rate in the high NLR group than the low NLR group, with eight showing p<0.05 and one showing p = 0.059. Five studies demonstrated an increased all-cause mortality risk in the high NLR group, as measured by the HR. Six studies looked at the mortality rates from CV. All studies indicated greater mortality rates in the high NLR group than in the low NLR group, with four of these studies showing p<0.05 and two showing p>0.05. The details of outcomes of included studies have been illustrated in Table 3.
| Author | Year | Mean Follow -up duration months) | Cut-off NLR value | Blood collected time | Outcome | |
|---|---|---|---|---|---|---|
| All-cause mortality | CV-cause mortality | |||||
| Neuen et al.17 | 2016 | 37 | High NLR ≥ 3.3 Low NLR < 3.3 | 3 months after HD | NLR was independently associated with all-cause mortality with HR of 1.4; 95% CI, 1.2–1.6; p=0.0001. | Kaplan-Meier analysis for high group NLR in cardiovascular-caused mortality showed P=0.0040 |
| Yaprak et al.18 | 2016 | 24 | High NLR ≥ 2.52 Low NLR < 2.52 | In the beginning of HD session in the middle of the week | All-cause mortality was higher in patients with a high NLR compared with a low NLR (18.8 vs. 7.5 %, P = 0.031) with a HR of 1.536 | NM |
| Li H et al.19 | 2017 | 36 | High NLR ≥ 3.5 Low NLR < 3.5 | Before initiation of the mid-week HD session | 88 of 268 (32.8%) patients died from overall causes with log rank 15.28 and P < 0.001 by Kaplan-Meier analysis in high group NLR with HR of 1.695 (1.288-2.23) | 62 of 88 (70.5%) patients died from cardiovascular causes with log rank 43.54 and P < 0.001 by Kaplan-Meier analysis in high group NLR with HR of 1.379 (1.162-1.637) |
| Woziwodzka et al.20 | 2019 | 60 | High NLR ≥ 3.9 Low NLR < 3.9 | NM | High NLR had higher mortality rate compared to low NLR (53.6 vs 30.4%; P = 0.039) with HR of 2.23 (1.10-4.50) | Low NLR had higher mortality rate for CV-cause compared to high NLR (25.0% vs. 42.9%; P = 0.10) |
| Diaz-Martinez et al.21 | 2019 | 12 | High NLR >1.75 Low NLR ≤ 1.75 | NM | Participants with NLR ≤ 1.75 had a 100% survival rate (log rank test, P = 0.059) compared with participants with NLR > 1.75 | NM |
| Balboul et al.22 | 2020 | 14 | NM | On a mid-week day predialysis | The fully adjusted all-cause mortality HR using Cox models with the time-varying risk effect was 1.034 (95% CI 1.01–1.059, P = 0.005). | The fully adjusted CV-cause mortality HR using Cox models with the time-varying risk effect was 1.039 (95% CI 0.997–1.084, P = 0.07). |
| Lano et al.23 | 2022 | 10 | High NLR ≥ 3.49 Low NLR < 3.49 | In the beginning of HD session in the middle of the week | The incidence of death from all-cause event was higher in high NLR group (38% versus 18% (P = 0.004)) | The incidence of death from cardiovascular event was higher in high NLR group (45% versus 26% (P = 0.01)) |
| Mureșan et al.24 | 2022 | 1 | High NLR ≥ 8.19 Low NLR < 8.19 | In the first 24 hours after admission | The mortality rate was higher in the high-NLR groups (40.12% vs. 1.97%; p < 0.0001) | NM |
| Wang J et al.25 | 2023 | 58 | High NLR ≥ 4 (G1 and G3 group) Low NLR < 4 (G2 and G4 group) | NM | Mortality rate of high NLR group were higher than low NLR group (mortality 31/ 69 vs 19/171), and the survival analysis indicated that patients with high NLR survival has lower survival rate than those with low NLR (P < 0.001) | Mortality rate of each group NLR: G1 (4%), G2 (6%), G3 (14%), and G4 (5%) and the survival analysis demonstrated a lower survival rate in G3 compared to G1, G2, and G4 (P < 0.001) |
NLR: Neutrophil-to-lymphocyte ratio, HD: Hemodialysis, NM: Not mentioned, CV: Cardiovascular, HR: Hazard ratios, CI: Confidence interval, G1: Group 1, G2: Group 2, G3: Group 3, G4, Group 4.
Meta-analysis outcomes
All-cause mortality
HD patients with high NLR had an increased all-cause mortality risk (3.83 times higher) than those with low NLR significantly (95% CI: 1.85-7.93; p=0.0003; I2=83%) [Figure 1]. An I2 value of 83% indicated significantly high data heterogeneity. This could be due to the different high NLR thresholds provided in the included studies. Thus, we conduced sensitivity analysis and subgroup analysis to provide the best results.
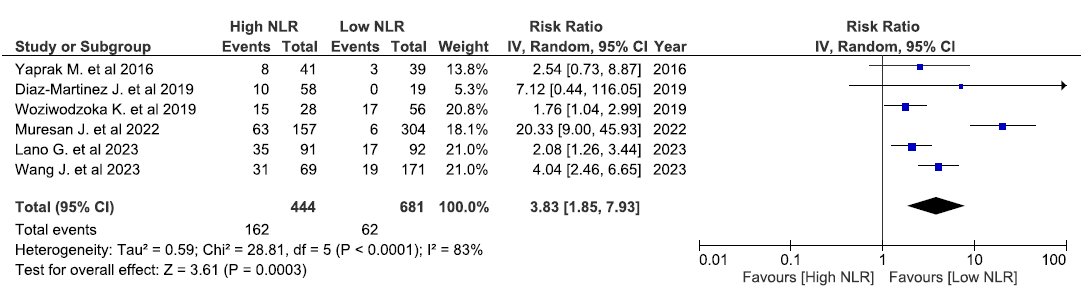
- Forest plot hemodialysis with high NLR versus low NLR and the risk of all-cause mortality. CI: Confidence interval, IV: Inverse variance, NLR: Neutrophil-to-lymphocyte ratio.
Based on Duval and Tweedie’s trim-and-fill analysis, we found that the exclusion of Mureșan et al.’s study24 resulted in a pooled RR of 2.53 (p < 0.00001) with moderate heterogeneity (I2 = 37%) [Figure 2]. This might be due to the study’s short follow-up period (1 month), resulting in more variable outcome measures, combined with different NLR thresholds. Subgroup analysis, regarding the most used NLR thresholds, (3.5-3.9) was further done to minimize the heterogeneity caused by different NLR thresholds.
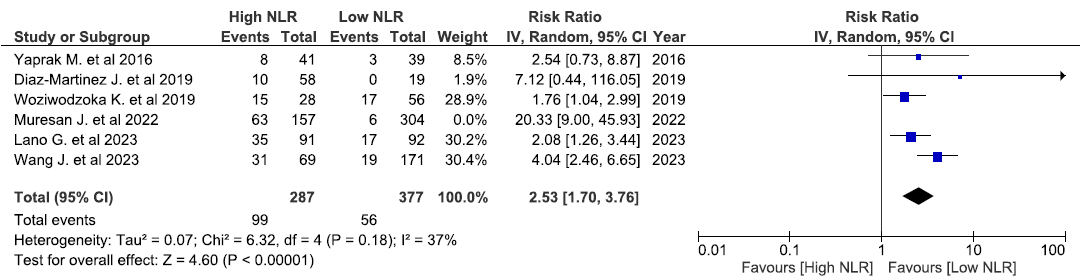
- Sensitivity analysis hemodialysis with high NLR versus low NLR and the risk of all-cause mortality (exclude Mureșan et al.24). CI: Confidence interval, IV: Inverse variance, NLR: Neutrophil-to-lymphocyte ratio.
Based on subgroup analysis limited to NLR threshold 3.5-3.9, HD patients with high NLR had a significantly increased risk of all-cause mortality (2.47 times higher) than those with low NLR (95%CI: 1.50-4.07; p=0.0004; I2=65%) [Figure 3]. The characteristics of the included studies for the all-cause mortality meta-analysis have been presented in Supplementary Table 1.
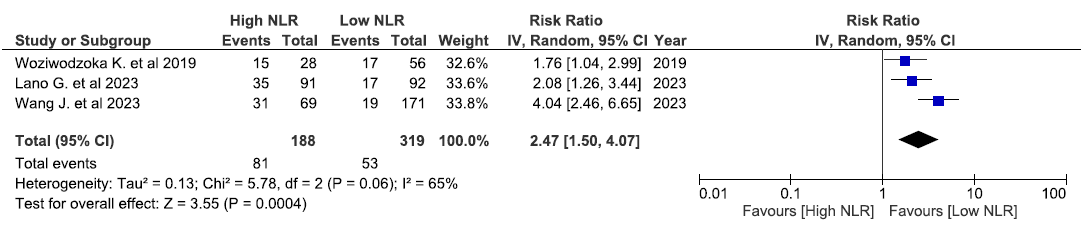
- Subgroup analysis hemodialysis with high NLR versus low NLR and the risk of all-cause mortality (NLR threshold 3.5-3.9). CI: Confidence interval, IV: Inverse variance, NLR: Neutrophil-to-lymphocyte ratio.
CV-cause mortality
Like the previous analysis of all-cause mortality, HD patients with high NLR had increased CV-caused mortality risk (1.19 times higher) than those with low NLR, though not significantly (95%CI: 0.82-1.72; p=0.37; I2=60%) [Figure 4]. An I2 value of 60% indicated moderate-to-high heterogeneity of data. This could be due to the different number of samples and different high NLR thresholds provided in included studies. Thus, we conducted sensitivity analysis.
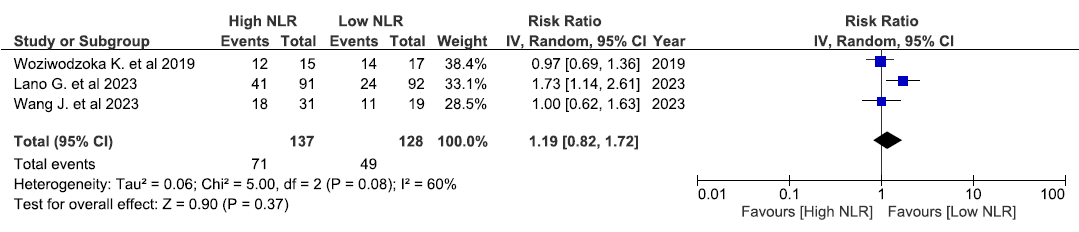
- Forest plot hemodialysis with high NLR versus low NLR and the risk of CV-cause mortality. CI: Confidence interval, IV: Inverse variance, NLR: Neutrophil-to-lymphocyte ratio.
Based on sensitivity analysis, the exclusion of Lano et al.’s study23 produces no heterogeneity (I2= 0%). However, the results were not significant and RR decreased to 0.98 with a 95% CI of 0.74-1.29 [Figure 5]. Thus, this result needs further studies to conclude the association between high NLR and CV-cause mortality in HD patients. The characteristics of the included studies for the CV-cause mortality meta-analysis have been presented in Supplementary Table 2.
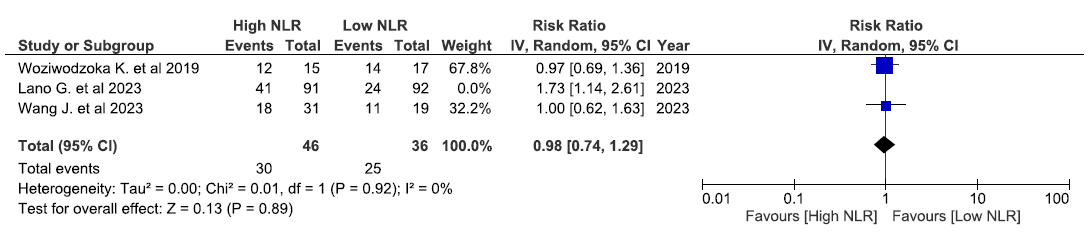
- Sensitivity analysis hemodialysis with high NLR versus low NLR and the risk of CV-cause mortality (exclude Lano et al.23). CI: Confidence interval, CV: Cardiovascular, IV: Inverse variance, NLR: Neutrophil-to-lymphocyte ratio.
Discussion
NLR is currently being extensively utilized to evaluate the prognosis of various illnesses.26-28 This study examines several cohort studies of patients with CKD on regular HD. These studies utilize NLR as a biomarker to evaluate the risk of death from any cause and CV-related causes. The results showed that a high NLR was associated with an elevated risk of both all-cause and CV mortality when compared with a low NLR.
Elevated NLR readings result from inflammatory disorders, which can stem from a range of factors including infection, trauma, cancer, and chronic diseases.12 In patients undergoing HD, chronic inflammation arises from various factors, including uremia, repeated vascular access, and oxidative stress associated with dialysis.29 A high NLR, characterized by increased neutrophils and decreased lymphocytes, indicates heightened inflammation that contributes to CV disease, the leading cause of death in this population.30 Beyond inflammation, mechanisms linking high NLR to CV risk include endothelial dysfunction and thrombosis. Neutrophils release ROS and enzymes that damage blood vessels, disrupting vascular health.31 They form neutrophil extracellular traps, promoting clot formation and raising the risk of heart attacks and strokes. Low lymphocyte counts further weaken immune surveillance, increasing vulnerability to infections that strain CV health.32 Additionally, metabolic issues common in HD patients, such as insulin resistance and dyslipidemia, are associated with elevated NLR. Neutrophils drive the chronic inflammation underlying these metabolic disorders, while reduced lymphocytes hinder the body’s ability to mitigate their effects, increasing the mortality risk.33
A previous study has demonstrated NLR’s role as a predictor for the severity of sepsis and as a prognostic indicator for mortality in patients with sepsis.34 Similarly, several studies have reported an association between increasing NLR values in CKD and worsening prognosis, leading to an escalation of mortality cases.35 High NLR levels reflect an intensified systemic inflammatory response, often due to tissue damage in patients with chronic inflammatory diseases, leading to vascular injury and multiple organ failure.28 Numerous cohort studies have reported higher mortality rates among CKD patients with elevated NLR, particularly with regard to CV-related mortality.36 While NLR is a valuable marker for assessing inflammation and its systemic impact, it does not replace kidney biomarkers such as urea, creatinine, and glomerular filtration rate in diagnosing kidney failure.37,38 Instead, NLR complements these biomarkers by providing additional prognostic information, which is especially beneficial in settings with limited access to comprehensive kidney function tests.
This MA is not without limitations. The varied NLR cut-off values in the studies pose challenges in determining the NLR cut-off. For instance, NLR values of 1.75 and 8.19 represent the lowest and highest cut-offs for all-cause mortality risk, respectively, while 3.49 and 4.0 (Woziwodzoka et al.,)20 are the lowest and highest cut-offs for CV-cause mortality risk. This is because numerous studies did not exclude alternative factors including malnutrition, malignancy, and hematological disease contributing to elevated NLR values apart from acute infection. The exclusion criteria varied across these studies, representing a second limitation. The absence of standardized blood sampling times among the included studies further contributed to the inconsistency in baseline NLR values. This variance complicates the determination of the cut-off value. Therefore, we use the NLR value ranges from 1.75 to 8.19 and 3.49 to 4 as cut-offs to assess all-cause mortality risk and CV-cause mortality risk, respectively. Future recommendations should aim to identify NLR cut-off values with minimal variation. The sensitivity analysis performed in this study obtained the lowest heterogeneity (I2=37%) by eliminating one study (Mureșan et al.),24 in which the NLR cut-off range obtained was 1.7521 to 4 (Wang et al.)25 with RR 2.53. This NLR cut-off (1.75 - 4) can be used as a recommendation for further research, particularly in assessing the prognosis of chronic renal failure patients receiving HD therapy. Therefore, identifying the sample, particularly the inclusion and exclusion criteria, will pose a challenge in obtaining appropriate cut-off values. Since the subject’s characteristics are the key factor that determine the cut-off value of NLR in patients with CKD, it is necessary for each country to establish its own recommended threshold. Hence, additional investigation is necessary within the identical geographical region, specifically targeting a group with a significantly higher prevalence of CKD.
In conclusion, this MA has shown the association between high NLR value and mortality in HD patients. This study has concluded that high NLR is associated with higher risk leading to mortality compared to low NLR. High NLR significantly increased the risk of all-cause mortality (3.83 times higher) compared with those with low NLR (95% CI: 1.85-7.93; p=0.0003; I2=83%) in HD patients, and the risk of CV-cause mortality (1.19 times higher) compared with those with low NLR, though not significantly (95%CI: 0.82-1.72; p=0.37; I2=60%). According to the results, the use of NLR might help in planning management of the patients with CKD, especially those on routine HD. However, due to the high heterogeneity of studies included in this MA, further studies regarding this topic are required.
Acknowledgments
The authors are grateful to all colleagues for all support and contributions provided.
Conflicts of interest
There are no conflicts of interest.
References
- Analysis of the global burden of disease study highlights the global, regional, and national trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney Int. 2018;94:567-81.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology of chronic kidney disease: An update 2022. Kidney Int Suppl (2011). 2022;12:7-11.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence of chronic kidney disease in Asia: A systematic review and analysis. BMJ Glob Health. 2022;7:e007525.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Impact and perspective on chronic kidney disease in an Asian developing country: A large-scale survey in North Vietnam. Nephron Clin Pract. 2008;109:c25-32.
- [CrossRef] [PubMed] [Google Scholar]
- The etiology of advanced chronic kidney disease in Southeast Asia: A meta-analysis. J Epidemiol Glob Health. 2024;14:740-64.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence of chronic kidney disease in China: Results from the sixth china chronic disease and risk factor surveillance. JAMA Intern Med. 2023;183:298-310.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Chronic kidney disease and its complications. Prim Care. 2008;35:329-44, vii.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- US renal data system 2020 annual data report: Epidemiology of kidney disease in the United States. Am J Kidney Dis. 2021;77:A7-8.
- [CrossRef] [PubMed] [Google Scholar]
- Alterations in symptoms and health-related quality of life as kidney function deteriorates: A cross-sectional study. J Clin Nurs. 2021;30:1787-96.
- [CrossRef] [PubMed] [Google Scholar]
- Predictors of mortality in hemodialysis patients. Pan Afr Med J. 2019;33:61.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Neutrophil-to-lymphocyte ratio, past, present and future perspectives. Bratisl Lek Listy. 2021;122:474-88.
- [CrossRef] [PubMed] [Google Scholar]
- Neutrophil to lymphocyte ratio: An emerging marker of the relationships between the immune system and diseases. Int J Mol Sci. 2022;23:3636.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Harnessing innate immune pathways for therapeutic advancement in cancer. Signal Transduct Target Ther. 2024;9:68.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Could a simple biomarker as neutrophil-to-lymphocyte ratio reflect complex processes orchestrated by neutrophils? J Transl Autoimmun. 2022;6:100159.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Lymphocyte cell ratios and mortality among incident hemodialysis patients. Am J Nephrol. 2017;46:408-16.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- High neutrophil/lymphocyte ratio is associated with poor renal outcomes in Japanese patients with chronic kidney disease. Ren Fail. 2019;41:238-43.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Neutrophil-lymphocyte ratio predicts cardiovascular and all-cause mortality in hemodialysis patients. Ren Fail. 2016;38:70-6.
- [CrossRef] [PubMed] [Google Scholar]
- Platelet-to-lymphocyte ratio predicts mortality better than neutrophil-to-lymphocyte ratio in hemodialysis patients. Int Urol Nephrol. 2016;48:1343-8.
- [CrossRef] [PubMed] [Google Scholar]
- High neutrophil-to-lymphocyte ratio predicts cardiovascular mortality in chronic hemodialysis patients. Mediators Inflamm 2017:9327136.
- [CrossRef] [Google Scholar]
- Neutrophil-to-lymphocyte ratio predicts long-term all-cause mortality in patients with chronic kidney disease stage 5. Folia Med Cracov. 2019;59:55-70.
- [CrossRef] [PubMed] [Google Scholar]
- The relationship of blood neutrophil-to-lymphocyte ratio with nutrition markers and health outcomes in hemodialysis patients. Int Urol Nephrol. 2019;51:1239-47.
- [CrossRef] [PubMed] [Google Scholar]
- Biological basis of lymphocyte ratios for survival prediction in hemodialysis patients: A longitudinal study. Int Urol Nephrol. 2020;52:1345-56.
- [CrossRef] [PubMed] [Google Scholar]
- Neutrophil:lymphocyte ratio correlates with the uremic toxin indoxyl sulfate and predicts the risk of death in patients on hemodialysis. Nephrol Dial Transplant. 2022;37:2528-37.
- [CrossRef] [PubMed] [Google Scholar]
- The predictive value of NLR, MLR, and PLR in the outcome of end-stage kidney disease patients. Biomedicines. 2022;10:1272.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Combined evaluation of geriatric nutritional risk index and neutrophil to lymphocyte ratio for predicting all-cause and cardiovascular mortality in hemodialysis patients. PLoS One. 2023;18:e0287696.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Combination of neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios as a novel predictor of cardiac death in patients with acute decompensated heart failure with preserved left ventricular ejection fraction: a multicenter study. J Am Heart Assoc. 2023;12:e026326.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The relation between neutrophil-to-lymphocyte ratio and coronary chronic total occlusions. BMC Cardiovasc Disord. 2014;14:130.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The neutrophil-lymphocyte ratio in children with atopic dermatitis: A case-control study. Clin Ter. 2017;168:e262-5.
- [CrossRef] [PubMed] [Google Scholar]
- The relationship between neutrophil-to-lymphocyte ratio and inflammation in end-stage renal disease patients. Ren Fail. 2012;34:155-9.
- [CrossRef] [PubMed] [Google Scholar]
- The neutrophil-to-lymphocyte ratio is associated with all-cause and cardiovascular mortality among individuals with hypertension. Cardiovasc Diabetol. 2024;23:117.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The association between neutrophil to lymphocyte ratio and endothelial dysfunction in people living with HIV on stable antiretroviral therapy. Expert Rev Anti Infect Ther. 2022;20:113-20.
- [CrossRef] [PubMed] [Google Scholar]
- Low lymphocyte count and cardiovascular diseases. Curr Med Chem. 2011;18:3226-33.
- [CrossRef] [PubMed] [Google Scholar]
- Associations between inflammation, hemoglobin levels, and coronary artery disease in non-albuminuric subjects with and without type 2 diabetes mellitus. Int J Mol Sci. 2023;24:14131.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Diagnostic and prognostic role of neutrophil-to-lymphocyte ratio in early and late phase of sepsis. Indian J Crit Care Med. 2018;22:660-3.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Neutrophil-to-lymphocyte ratio in relation to trauma severity as prognosis factors in patients with multiple injuries complicated by multiple organ dysfunction syndrome: A retrospective analysis. Immun Inflamm Dis. 2023;11:e1031.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Neutrophil-to-lymphocyte ratio and incident end-stage renal disease in Chinese patients with chronic kidney disease: Results from the Chinese Cohort Study of Chronic Kidney Disease (C-STRIDE) J Transl Med. 2019;17:86.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract.. 2012;120:c179-84.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic kidney disease diagnosis and management: A review. JAMA. 2019 Oct;322:1294-1304.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]








